Published online Aug 7, 2009. doi: 10.3748/wjg.15.3631
Revised: June 22, 2009
Accepted: June 29, 2009
Published online: August 7, 2009
AIM: To evaluate the accuracy of spot urinary Na/K and Na/creatinine (Cr) ratios as an alternative to 24-h urinary sodium in monitoring dietary compliance in patients with liver cirrhosis and ascites treated with diuretics.
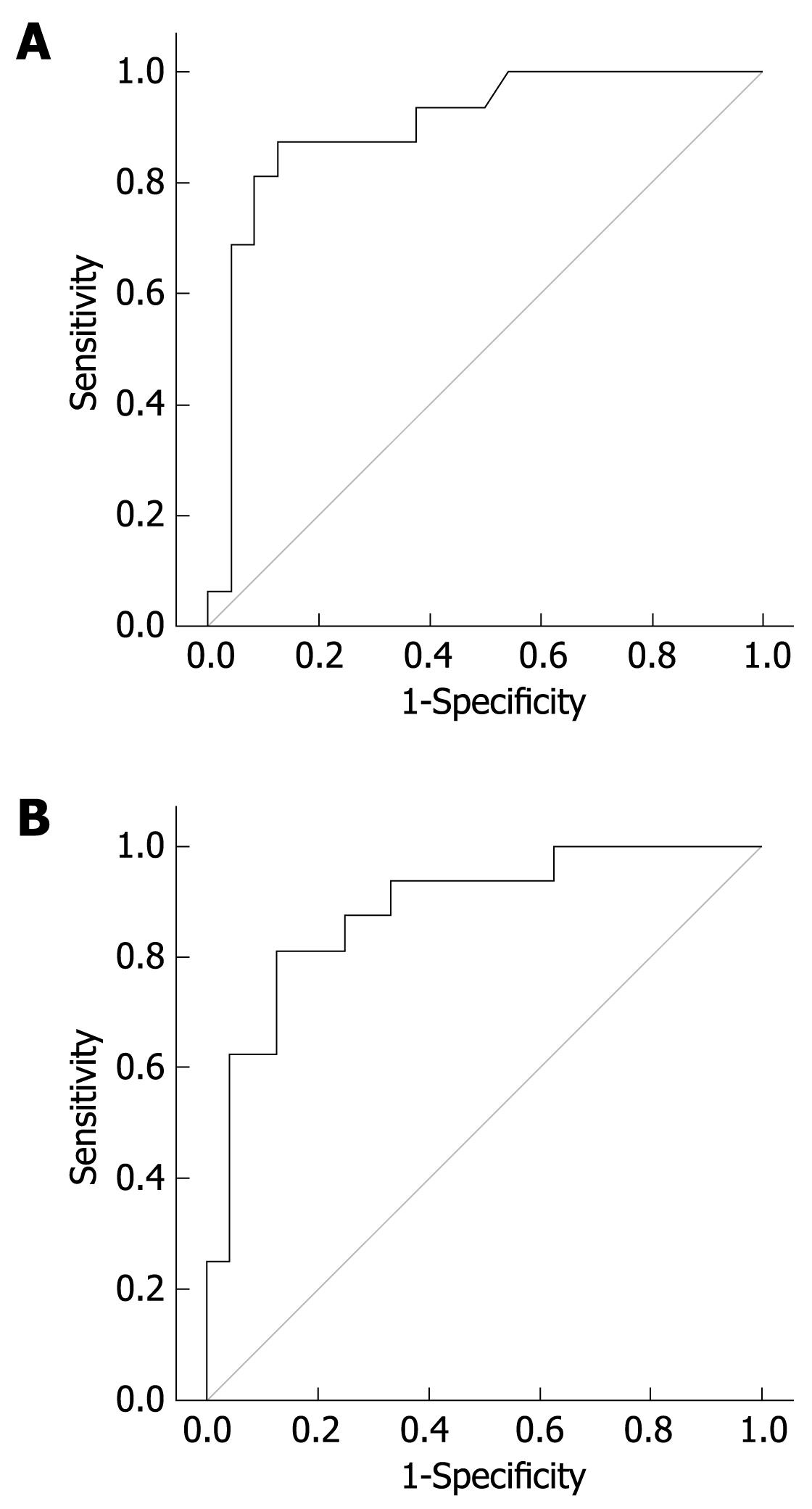
METHODS: The study was carried on 40 patients with liver cirrhosis and ascites treated with diuretic therapy. Patients were divided into two groups according to 24-h urinary sodium. We measured spot urine Na/K ratio, Na/Cr ratio and 24-h urinary sodium. Student’s t test was used to compare the interval variables and χ2 test to compare the nominal variables between the two groups. Receiver operator characteristic curve was used to identify the best cutoff point for Na/K and Na/Cr ratio.
RESULTS: The best cutoff point for Na/K ratio was 2.5 (P < 0.001) and area under the curve (AUC) was 0.9, and for Na/Cr ratio, the best cutoff point was 35 (P < 0.001) and AUC was 0.885. Na/K ratio showed higher sensitivity and accuracy compared to Na/Cr ratio (87.5% and 87% for Na/K ratio; 81% and 85% for Na/Cr ratio, respectively).
CONCLUSION: Spot urine Na/K ratio has adequate accuracy for assessment of dietary sodium restriction compared with 24-h urinary sodium in patients with liver cirrhosis and ascites.
- Citation: El-Bokl MA, Senousy BE, El-Karmouty KZ, Mohammed IEK, Mohammed SM, Shabana SS, Shalaby H. Spot urinary sodium for assessing dietary sodium restriction in cirrhotic ascites. World J Gastroenterol 2009; 15(29): 3631-3635
- URL: https://www.wjgnet.com/1007-9327/full/v15/i29/3631.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.3631
Ascites is considered to be the most common of the three major complications of cirrhosis; other complications are hepatic encephalopathy and variceal bleeding. It is estimated that about 50% of patients with compensated cirrhosis will develop ascites within 10 years of observation[1]. The development of ascites in patients with liver cirrhosis is associated with poor prognosis and an increased risk of mortality, as approximately 50% of patients with ascites are expected to succumb within 2 years[2].
The development of ascites is secondary to renal retention of sodium and water because of underlying activation of neurohormonal mechanisms[3]. Therefore, patients who accumulate ascites have urinary excretion of sodium that is significantly lower than their dietary salt intake. This means that, in order to achieve successful ascites mobilization, patients should have a negative sodium balance. This can be achieved through education regarding dietary sodium restriction (2 g/d) in addition to oral diuretic therapy[4]. The usual diuretic regimen starts with single morning doses of oral spironolactone (100 mg) and furosemide (40 mg). Efficacy of therapy is monitored through the goal of average weight loss of 300-500 g/d in patients without peripheral edema and 800-1000 g/d in those with peripheral edema. Doses can be increased gradually in patients who show inadequate response, to reach a maximum of 400 mg/d spironolactone and 160 mg/d furosemide[5].
This approach is effective in approximately 90% of patients and 10% are considered diuretic-resistant and second-line therapy is indicated for ascites mobilization[6]. However, patients who are not compliant with diet may also show inadequate response to maximum diuretic doses. Assessment of dietary compliance is important in order to avoid mislabeling patients with refractory ascites, while their problem is inadequate dietary salt restriction[7]. Several methods have been suggested for assessment of dietary compliance: (1) The usual method is measuring 24-h urinary sodium excretion. Patients who gain weight despite excreting more than 78 mEq Na/d are not compliant with the diet[8]. However, the main problem here is that it may be difficult for the patient to accurately collect 24 h urine. At the same time, using spot urinary sodium is easier for the patient but it is not accurate because of the lack of uniform excretion of sodium throughout the day. (2) Furosemide-induced natriuresis can be used. A single intravenous 80-mg dose of furosemide is given and urinary sodium is measured in the next 8 h. Patients with diuretic resistance have sodium excretion < 50 mEq/8 h[910]. (3) There is some evidence that spot urinary Na/K ratio may be as helpful as 24-h urinary sodium collection, with adequate accuracy, when the ratio more than a given cut value (one in some studies) is equivalent to 24 h sodium more than 78 mmol Na/d[1112].
The aim of this study was to assess the accuracy of spot urinary Na/K and Na/creatinine (Cr) ratio for assessment of dietary sodium restriction in patients with liver cirrhosis and ascites treated with diuretic therapy.
The study was conducted on 40 patients (28 male and 12 female; mean age 50 ± 4.5 years) with liver cirrhosis and ascites treated with diuretics, who were admitted to the Department of Internal Medicine in Ain Shams University Hospitals. The study was performed according to the ethical standards for human experimentation and was approved by the scientific committee of Ain Shams University. Informed consent was obtained from the selected patients after explaining the aim of the study and the nature of the investigations required. Liver cirrhosis was documented by clinical assessment, laboratory findings and evidence of liver cirrhosis upon abdominal ultrasound. Ascitic fluid analysis was done to exclude malignancy and spontaneous bacterial peritonitis. Patients with evidence of portosystemic encephalopathy or intrinsic renal disease were excluded from the study. All patients had normal kidneys upon ultrasound and no proteinuria or active urinary sediment upon urine analysis. Daily monitoring of patient weight and lack of response to diuretics was defined according to the consensus conference of the International Ascites Club, which is mean weight loss of < 0.8 kg over 4 d[5].
Collection of 24-h urine sample for calculation of sodium was done in sterile plastic containers by recording the volume in 24 h, starting at 08:00. Verbal instructions were given to assure completeness of collection. Samples were centrifuged and sodium concentration was measured in mEq/L using a Beckman Synchron CX5 ISE (NJ, USA) chemistry analyzer. All samples were processed on the day of collection. In order to obtain the whole 24-h urinary sodium, we multiplied sodium concentration by the volume in liters. Spot urine samples were collected for measurement of sodium, potassium and creatinine. Samples were handled as previously described for 24-h samples, except that volume was not recorded, as it has no significance in this setting. Patients were divided into two groups according to 24-h urinary sodium.
Data were collected, revised, verified and edited on a PC. Data were then analyzed statistically using SPSS statistical package version 25 (SPSS, Chicago, IL, USA). Patients were divided according to 24-h urinary sodium excretion into diuretic-resistant (16 patients with 24-h urinary sodium < 78 mEq) and diuretic-sensitive (24 patients with 24-h urinary sodium ≥ 78 mEq). Data were reported in the form of mean ± SD. Student’s t test was used to compare the interval variables and the χ2 test was used to compare the nominal variables between the two groups. Correlation between 24-h urinary sodium and other variables was done using Pearson correlation. In order to identify the best cutoff point for Na/K ratio and Na/Cr ratio, a receiver operator characteristic (ROC) curve was used. P < 0.05 was considered statistically significant.
According to the type of diuretic used, 28 patients were taking furosemide and spironolactone in combination; four, furosemide alone; three, spironolactone alone; and five, spironolactone in combination with bumetanide. There was no significant difference between the two groups with regard to type of diuretics used.
As shown in Table 1, there was no significant difference between the groups as regards age, sex, serum creatinine, serum potassium, liver enzymes, serum bilirubin, total proteins, international normalized ratio or partial thromboplastin time. The following parameters were significantly lower in the diuretic-resistant group: serum sodium, serum albumin, white blood cell (WBC) count and platelet count. However, the diuretic-resistant patients had higher blood urea nitrogen (BUN) and higher Child score. Table 2 shows that 24-h urinary sodium, spot urine Na/K ratio and spot urine Na/Cr ratio were significantly lower in the diuretic-resistant patients.
| Diuretic-resistant group (n = 24) | Diuretic-sensitive group (n = 16) | P | |
| Age (yr) | 50 ± 4 | 49 ± 4 | NS |
| Sex ratio (Male/female) | 17/7 | 11/5 | NS |
| Weight loss (yes/no) | 0/24 | 9/7 | 0.001 |
| Serum creatinine (mg/dL) | 1.1 ± 0.2 | 0.9 ± 0.2 | NS |
| BUN (mg/dL) | 23.5 ± 8.3 | 18.5 ± 8.3 | 0.033 |
| Serum sodium (mEq/L) | 128 ± 5 | 136 ± 5 | 0.001 |
| Serum potassium (mEq/L) | 4.3 ± 0.6 | 4.3 ± 0.5 | NS |
| AST (U/L) | 68 ± 34 | 69 ± 40 | NS |
| ALT (U/L) | 56 ± 27 | 57 ± 27 | NS |
| ALP (U/L) | 283 ± 56 | 246 ± 84 | NS |
| Total bilirubin (mg/dL) | 3.8 ± 1.7 | 3.2 ± 1.8 | NS |
| Direct bilirubin (mg/dL) | 1.9 ± 1.1 | 1.6 ± 0.9 | NS |
| Total proteins (g/dL) | 7.1 ± 0.4 | 7.2 ± 0.5 | NS |
| Serum albumin (g/dL) | 2.4 ± 0.4 | 2.8 ± 0.4 | 0.012 |
| WBC count (× 109/L) | 6.6 ± 2.4 | 8.8 ± 4.3 | 0.045 |
| Hemoglobin (g/dL) | 9.7 ± 1.7 | 9.5 ± 2.6 | NS |
| Platelet count (× 109/L) | 73 ± 24 | 108 ± 58 | 0.014 |
| INR | 2.9 ± 1.3 | 1.5 ± 0.2 | NS |
| PTT (s) | 36 ± 9 | 32 ± 7 | NS |
| Child classification (B/C) | 1/23 | 6/10 | 0.011 |
| Diuretic-resistant group (n = 24) | Diuretic-sensitive group (n = 16) | P | |
| 24 h urinary sodium (mEq) | 33 ± 19 | 126 ± 46 | 0.001 |
| Spot urine Na/K ratio | 1.3 ± 1.3 | 3.7 ± 1.6 | 0.001 |
| Spot urine Na/Cr ratio | 21 ± 18 | 100 ± 87 | 0.001 |
Significant correlation was noted between 24-h urinary sodium and Na/K ratio (r = 0.76, P = 0.001), Na/Cr ratio (r = 0.56, P = 0.001), serum sodium (r = 0.59, P = 0.001), serum BUN (r = -0.31, P = 0.046) and Child score (r = -0.31, P = 0.05).
Figure 1A represents the ROC curve for the best cutoff point to differentiate between diuretic sensitivity and resistance using spot urine Na/K ratio. Area under the curve (AUC) was 0.9 and P < 0.001. According to the curve, the best cutoff point was 2.5, with 87.5% sensitivity and specificity and 85% accuracy. Using higher or lower cutoff points shows lower accuracy although sensitivity or specificity may be higher (Table 3).
| Ratio | Sens (%) | Spec (%) | PPV (%) | NPV (%) | Acc (%) | |
| Na/K ratio | 1 | 93.8 | 58.3 | 76.7 | 90.0 | 80.0 |
| 2.5 | 87.5 | 87.5 | 91.3 | 82.4 | 87 | |
| 3.5 | 50 | 95.8 | 92.3 | 55.6 | 67.5 | |
| Na/Cr ratio | 20 | 93.8 | 66.7 | 82.1 | 91.7 | 85.0 |
| 35 | 81 | 87.5 | 91 | 77.8 | 85.0 | |
| 45 | 62.5 | 87.5 | 88.2 | 60.9 | 72.5 |
During treatment of ascites in patients with liver cirrhosis, excess sodium intake can be misinterpreted as diuretic unresponsiveness, as in the present study, seven patients showed no weight loss in response to diuretics, while their 24-h sodium excretion was > 78 mEq. Appropriate identification of such patients is also important to avoid complications of unnecessary increase in diuretic dosage (mainly encephalopathy and electrolyte disturbance) and complications of unnecessary large volume paracentesis (mainly mechanical trauma, post-paracentesis circulatory dysfunction and possible increased incidence of spontaneous bacterial peritonitis caused by ascitic fluid protein depletion)[13].
Measuring 24-h urinary sodium is used currently to identify such patients; however, it may be difficult for patients to collect urine appropriately and lack of appropriate collection can lead to false low results, and again, false-labeling of the patient as unresponsive to diuretics. Using 24-h urinary creatinine has been proposed as a method to ensure adequate collection of urine[14], but even this may not be accurate, because patients with advanced liver cirrhosis can have muscle wasting, and therefore, lower creatinine excretion in urine, even with complete collection[15].
The present study shows that spot urine Na/K ratio can be used as an easier alternative to 24-h urinary sodium excretion, with adequate accuracy. At the best cutoff point, Na/K ratio was shown to be more accurate than Na/Cr ratio, with better sensitivity and specificity. Similar observations as regards spot urine Na/K ratio have been made by others[1112]. However, according to these other studies, the best cutoff point is 1, while in the present study, the best sensitivity, specificity and accuracy was noted at a cutoff point of 2.5. This difference may have been caused by a difference in types of diuretics used, which may affect urinary sodium and potassium excretion. Further studies are needed with classification of patients into groups according to types of diuretics used in order to document any significant effect on Na/K ratio.
Another test used is furosemide-induced natriuresis, which can identify diuretic unresponsiveness with adequate accuracy[910]. However, it still needs urine collection for 8 h after furosemide administration. At the same time, it can identify patients with refractory ascites (those who do not respond to maximum doses of diuretics), even before reaching the maximum dose, which is an advantage over spot urine Na/K ratio. Probably we should use Na/K ratio for routine assessment of sodium restriction during diuretic therapy, and keep the furosemide-induced natriuresis test for patients that we suspect are completely resistant to medical treatment, therefore, we can make early referral for liver transplantation or procedures like transjugular intrahepatic portosystemic shunt.
Patients with more advanced liver disease have more deterioration in liver function and marked degrees of circulatory dysfunction and neurohumoral activation [including antidiuretic hormone (ADH)], which results in enhanced sodium renal tubular reabsorption, and therefore, more diuretic resistance[16]. It has been shown also by another study that lower urinary sodium in cirrhotic patients with ascites is associated with reduced survival[17]. This was noted in the present study, as patients with lower urinary sodium had more advanced liver disease in the form of lower serum albumin and higher Child-Pugh score. Also, lower serum sodium in the resistant group represents more impairment of free water excretion because of a high level of ADH that leads to dilutional hyponatremia in patients with more resistant ascites[718].
According to the main theory of ascites formation, the initial step in pathogenesis is the development of portal hypertension[16]. Platelet and WBC counts are already suggested as noninvasive tests for prediction of esophageal varices[1920], another complication of portal hypertension. The lower platelet and WBC counts associated with diuretic resistance in the present study may also represent more advanced liver disease and more severe portal hypertension in the unresponsive patients.
One of the results of neurohormonal activation in advanced liver disease is renal vasoconstriction, which may reduce the glomerular filtration rate (GFR) and present later as hepatorenal syndrome[621]. The reduction in GFR in these patients may be masked by serum creatinine concentration that appears to be within the normal range, with a GFR as low as 20 mL/min[1522]. In the present study, patients in the resistant group had higher BUN, which was similar to that in a previous study[12]. This may represent impairment in renal function masked by normal serum creatinine.
In conclusion, dietary sodium restriction is essential in mobilization of ascites caused by liver cirrhosis in addition to diuretics. Monitoring of dietary compliance is essential and exclusion of excess sodium intake is important in patients who appear unresponsive to diuretics. However, this is often missed, perhaps because of the difficulty of 24-h urine collection. Using spot urine Na/K ratio may be as accurate as 24-h urinary sodium measurement, with the advantage of being more applicable for the patient. However, further studies are still needed before accepting this test in practice, mainly testing the effect of the type of diuretic used on the best cutoff value. Another point we recommend testing is whether there is diurnal variation for this ratio, and if there is a preference for a first morning voiding sample.
Monitoring dietary compliance is an important aspect in treatment of ascites caused by liver cirrhosis. The standard test used is 24-h urinary sodium, however, its use is limited by difficulty of urine collection over 24 h. Few studies have evaluated spot urine Na/K ratio as an alternative.
In the present study, the standard 24-h urine test was compared to spot urine Na/K and Na/creatinine (Cr) ratio in patients with ascites caused by cirrhosis, treated with diuretics.
The present study showed adequate accuracy for spot urine tests when compared to 24-h urinary sodium assessment. The accuracy, sensitivity and specificity of Na/K ratio are higher than those for Na/Cr ratio. Also, the study showed greater deterioration in liver function in patients who had lower urinary sodium excretion.
Na/K ratio may be used in clinical practice to monitor dietary sodium compliance in patients with ascites and liver cirrhosis. It should be more convenient for the patient compared to the 24-h urinary sodium test.
Spot urinary Na/K ratio was previously proposed a few years ago as a substitute for 24-h urinary sodium. Nevertheless the first communications were only published as abstracts. As far as we know, this is the first full publication regarding this issue. The statistical procedures are adequate and the methods of the research are good. The only criticism is the low sample size. This paper should be useful for readers of the journal.
| 1. | Ginés P, Quintero E, Arroyo V, Terés J, Bruguera M, Rimola A, Caballería J, Rodés J, Rozman C. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7:122-128. [Cited in This Article: ] |
| 2. | D'Amico G, Morabito A, Pagliaro L, Marubini E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31:468-475. [Cited in This Article: ] |
| 3. | Yu AS, Hu KQ. Management of ascites. Clin Liver Dis. 2001;5:541-568, viii. [Cited in This Article: ] |
| 4. | Ginès P, Cárdenas A, Arroyo V, Rodés J. Management of cirrhosis and ascites. N Engl J Med. 2004;350:1646-1654. [Cited in This Article: ] |
| 5. | Moore KP, Wong F, Gines P, Bernardi M, Ochs A, Salerno F, Angeli P, Porayko M, Moreau R, Garcia-Tsao G. The management of ascites in cirrhosis: report on the consensus conference of the International Ascites Club. Hepatology. 2003;38:258-266. [Cited in This Article: ] |
| 6. | Cárdenas A, Ginès P. Management of refractory ascites. Clin Gastroenterol Hepatol. 2005;3:1187-1191. [Cited in This Article: ] |
| 7. | Ginès P, Cárdenas A. The management of ascites and hyponatremia in cirrhosis. Semin Liver Dis. 2008;28:43-58. [Cited in This Article: ] |
| 8. | Runyon BA. Management of adult patients with ascites due to cirrhosis. Hepatology. 2004;39:841-856. [Cited in This Article: ] |
| 9. | Spahr L, Villeneuve JP, Tran HK, Pomier-Layrargues G. Furosemide-induced natriuresis as a test to identify cirrhotic patients with refractory ascites. Hepatology. 2001;33:28-31. [Cited in This Article: ] |
| 10. | Cho HS, Park GT, Kim YH, Shim SG, Kim JB, Lee OY, Choi HS, Hahm JS, Lee MH. [The significance of urine sodium measurement after furosemide administration in diuretics-unresponsive patients with liver cirrhosis]. Taehan Kan Hakhoe Chi. 2003;9:324-331. [Cited in This Article: ] |
| 11. | Karatapanis S, Ketikoglou I, Skorda L, Kopanakis D, Metaxaki P, Lisgos F, Komnianides K, Artikis V. The role of spot urine Na+/K+ ratio in the management of ascites in cirrhotic patients. Gut. 2003;52:A53. [Cited in This Article: ] |
| 12. | Stiehm AJ, Mendler MH, Runyon BA. Detection of diuretic-resistance or diuretic-sensitivity by spot urine Na/K ratios in 729 specimens from cirrhotics with ascites: approximately 90 percent accuracy as compared to 24-hr urine Na excretion (abstract). Hepatology. 2002;36:222A. [Cited in This Article: ] |
| 13. | Runyon BA, Antillon MR, Montano AA. Effect of diuresis versus therapeutic paracentesis on ascitic fluid opsonic activity and serum complement. Gastroenterology. 1989;97:158-162. [Cited in This Article: ] |
| 14. | Pirlich M, Selberg O, Böker K, Schwarze M, Müller MJ. The creatinine approach to estimate skeletal muscle mass in patients with cirrhosis. Hepatology. 1996;24:1422-1427. [Cited in This Article: ] |
| 15. | Caregaro L, Menon F, Angeli P, Amodio P, Merkel C, Bortoluzzi A, Alberino F, Gatta A. Limitations of serum creatinine level and creatinine clearance as filtration markers in cirrhosis. Arch Intern Med. 1994;154:201-205. [Cited in This Article: ] |
| 16. | Cárdenas A, Bataller R, Arroyo V. Mechanisms of ascites formation. Clin Liver Dis. 2000;4:447-465. [Cited in This Article: ] |
| 17. | Arroyo V, Bosch J, Gaya-Beltrán J, Kravetz D, Estrada L, Rivera F, Rodés J. Plasma renin activity and urinary sodium excretion as prognostic indicators in nonazotemic cirrhosis with ascites. Ann Intern Med. 1981;94:198-201. [Cited in This Article: ] |
| 18. | Ginés P, Berl T, Bernardi M, Bichet DG, Hamon G, Jiménez W, Liard JF, Martin PY, Schrier RW. Hyponatremia in cirrhosis: from pathogenesis to treatment. Hepatology. 1998;28:851-864. [Cited in This Article: ] |
| 19. | Giannini EG, Zaman A, Kreil A, Floreani A, Dulbecco P, Testa E, Sohaey R, Verhey P, Peck-Radosavljevic M, Mansi C. Platelet count/spleen diameter ratio for the noninvasive diagnosis of esophageal varices: results of a multicenter, prospective, validation study. Am J Gastroenterol. 2006;101:2511-2519. [Cited in This Article: ] |
| 20. | Gue CS, Yap CK, Ng HS. The correlation between cytopenia and esophageal varices in patients with liver cirrhosis. Med J Malaysia. 2004;59:604-608. [Cited in This Article: ] |
| 21. | Bataller R, Ginès P, Guevara M, Arroyo V. Hepatorenal syndrome. Semin Liver Dis. 1997;17:233-247. [Cited in This Article: ] |