Summary
Abstract
Risperidone (Risperdal®), a psychotropic atypical antipsychotic agent, is thought to act via dopamine D2 and serotonin (5-HT [5-hydroxytryptamine])2A receptor antagonism. The clinical efficacy of oral risperidone in the treatment of bipolar mania and schizophrenia in adult patients is well established. In the US, risperidone is also approved for the treatment of irritability associated with autistic disorder in children and adolescents aged 5–16 years, for the treatment of schizophrenia in adolescents aged 13–17 years and, as monotherapy, for the short-term treatment of acute manic and mixed episodes associated with bipolar I disorder in children and adolescents aged 10–17 years.
Oral risperidone treatment was better than placebo treatment in reducing irritability and other behavioral symptoms associated with autistic disorder in children and adolescents in two well designed short-term trials, with these benefits maintained in those receiving risperidone for up to 6 months. The drug had a clinically manageable tolerability profile, with most adverse events being of mild to moderate intensity. There are some aspects of treatment, such as weight gain, somnolence, and hyperglycemia, that require monitoring, and the long-term safety of risperidone in children and adolescents with autistic disorder remains to be fully determined. With these issues in mind, risperidone offers a valuable emerging option for the treatment of irritability associated with autistic disorder in children and adolescents.
Pharmacologic Properties
Although the mechanism of action of risperidone, a benzisoxazole derivative, is unknown, its pharmacodynamic effects are thought to be mediated via dopamine D2 and serotonin 5-HT2A receptor antagonism. Risperidone and its active metabolite 9-hydroxyrisperidone have high in vitro binding affinity for these receptors, which results in significant inhibition of both serotonin and dopamine, with the pharmacologic effects of risperidone attributed to the combined effects of risperidone plus 9-hydroxyrisperidone. The neurotransmitter binding profile of risperidone may provide the putative mechanisms for its antipsychotic effects and generally lower incidence of adverse effects relative to older antipsychotic agents.
Risperidone is absorbed rapidly and has a high bioavailability (70%). In autistic children, peak plasma levels of risperidone and 9-hydroxyrisperidone were achieved ≈1 and 1–4 hours post dose. The drug is 90% plasma protein bound and undergoes extensive hepatic metabolism, largely via cytochrome P450 (CYP) 2D6-mediated hydroxylation to 9-hydroxyrisperidone, and to a small extent via N-dealkylation. In autistic children, the mean terminal half-lives of risperidone and 9-hydroxyrisperidone were ≈2 and 11–16 hours, which were 30–35% lower than those in adults. Risperidone and its metabolites are eliminated largely via the urine and partly via the feces.
Dosage adjustments are required in patients with moderate to severe renal impairment due to reduced clearance, and in patients with hepatic impairment due to an increase in the free fraction of the drug. Coadministration of CYP2D6 and/or CYP3A inhibitors (e.g. clozapine and fluoxetine) may interfere with the conversion of risperidone to 9-hydroxyrisperidone, whereas coadministration of inducers (e.g. carbamazepine and rifampin [rifampicin]) may decrease the combined plasma concentrations of the drug and its metabolite.
Therapeutic Efficacy
In two 8-week, randomized, double-blind trials (n = 101 and 55) in autistic children and adolescents (aged 5–17 years), patients receiving oral risperidone (mean modal dosage of 1.37–1.96 mg/day) had significantly greater improvements from baseline in irritability scores than those receiving placebo (primary endpoint). In modified intent-to-treat analyses, parent-rated mean Aberrant Behavior Checklist-Irritability Subscale (ABC-IS) scores were reduced by 56.9% and 65.0% from baseline in the risperidone groups versus a decrease of 14.1% and 34.7%, respectively, in the placebo groups. There were also significantly greater improvements from baseline for some of the other ABC subscale mean scores (Stereotypic behavior, lethargy/social withdrawal, and/or hyperactivity/noncompliance subscales) in risperidone groups than in placebo groups and a significantly higher proportion of patients in risperidone groups achieved a positive response. Other secondary endpoints also favored risperidone treatment in one or both of these short-term trials, including those for repetitive behavior and measures of relatedness and impaired communication (assessed using the parent-rated modified Ritvo-Freeman Real Life Rating Scale [RFRLRS], the validated clinician-rated Children’s Yale-Brown Obsessive Compulsive Scale [CYBOCS], and the clinician-rated Maladaptive Behavior Domain of Vineland Adaptive Behavior Scales [MBD-VABS]), scores for the conduct problem, hyperactive, and overly sensitive subscales of the parent-rated Nisonger Child Behavior Rating Form, and the score for hyperactivity on the visual analog scale for the most troublesome symptoms.
The benefits of up to 6 months’ risperidone treatment (mean modal dosage of risperidone was 1.96 mg/day), in terms of mean ABC-IS scores (no clinically relevant change) and clinician-rated Clinical Global Impression-Improvement scores (coprimary endpoints), were maintained in an open-label extension and double-blind, placebo-controlled, discontinuation trial (n = 63). Efficacy was also maintained in the longer term, according to secondary endpoints, including changes from baseline in most other mean ABC subscales, and in RFRLRS, CYBOCS, and MBD-VABS scores. In addition, patients receiving risperidone showed significant improvements in adaptive behavior for areas of communication, daily living skills, and socialization. Of note, significantly fewer patients in the risperidone-treatment group than in the placebo-treatment group relapsed during the placebo-controlled discontinuation phase; as a consequence, the discontinuation phase was stopped early.
Tolerability
Risperidone had a clinically manageable tolerability profile in children and adolescents with autistic disorder receiving up to 6 months’ treatment in short- and longer-term clinical trials. Most treatment-emergent adverse events were of mild to moderate intensity, with most resolving spontaneously or being effectively managed with dosage adjustments. In short-term trials, very few patients discontinued treatment due to an adverse event. In a pooled descriptive analysis of short-term clinical trials, the most common treatment-emergent adverse events (i.e. those occurring in >10% of patients receiving risperidone [n = 76] and at a rate that was at least twice that in the placebo group [n = 80]) were somnolence, increased appetite, fatigue, upper respiratory tract infection, increased saliva, constipation, dry mouth, tremor, and dystonia. The most common of these was somnolence, which was generally transient in nature.
There was a higher incidence of adverse events associated with extrapyramidal symptoms in the risperidone group than in the placebo group in a pooled analysis of short-term trials evaluating risperidone treatment. In clinical trials, tardive dyskinesia occurred in 2 of 1885 children and adolescents with autistic disorder or other psychiatric disorders receiving risperidone, with these cases resolving upon discontinuation of treatment. Risperidone treatment was associated with weight gain in short- and longer-term trials, with these increases being in excess of developmentally expected norms. There was no correlation between serum leptin levels and weight gain in 63 children and adolescents with autistic disorder receiving risperidone for up to 6 months. In double-blind trials, 49% of children and adolescents receiving risperidone had elevated serum prolactin levels compared with 2% of patients in the placebo group. Galactorrhea, amenorrhea, gynecomastia, and impotence have been reported in patients receiving prolactin-elevating compounds. In addition, when long-standing hyperlactinemia is associated with hypogonadism, patients of both genders may experience a decrease in bone density. In a retrospective analysis of pooled data from five clinical trials in 572 evaluable children (aged 5–15 years) with disruptive behavior disorders, there were no statistically or clinically relevant effects on growth, or the onset or progression of puberty with risperidone treatment for up to 1 year.
Similar content being viewed by others
1. Introduction
Autistic disorder or autism is a subtype of pervasive developmental disorders (PDD); PDD includes conditions covered by autism spectrum disorders (i.e. autistic disorder, Asperger syndrome and PDD not otherwise specified), Rett syndrome, and childhood disintegrative disorder. Autistic disorder is a lifelong condition that appears to be increasing in prevalence, with recent evidence suggesting that the estimated prevalence is 10–20 per 10 000 population.[1–4] Onset of autistic disorder typically occurs during the first 3 years of life, with the disorder affecting approximately four times more males than females; approximately two-thirds of patients also have intellectual disability and one-third of individuals develop epilepsy.[4,5] The three key manifestations of autistic disorder are communication impairment, abnormal social interaction, and a restricted range of interests and behaviors, all of which are exacerbated by behavioral problems, such as severe tempers, aggression and irritability.[4,6]
There is no cure for autistic disorder, with management of the disorder taking a multimodal approach that focuses on ameliorating symptoms, thereby improving the patient’s and their caregiver’s quality of life.[7,8] Educational and behavioral interventions are the cornerstone for treatment; however, despite these interventions, many autistic patients remain significantly impaired, and thus pharmacotherapy may be initiated to alleviate symptoms, such as irritability and aggression.[7,8] Antipsychotic agents are the most frequently prescribed psychoactive agents for the management of these symptoms.[9] Although extensive clinical experience has shown that the typical antipsychotic agent haloperidol is an effective agent for the management of these behavioral problems, its use is limited because of the high rate of drug-related tardive and withdrawal dyskinesia.[7,8] Hence, attention has turned to the use of atypical antipsychotic agents, including risperidone (Risperdal®)Footnote 1, which generally have a better tolerability profile than typical antipsychotic agents.[9]
This review focuses on the clinical use of risperidone in children and adolescents with autistic disorder; the pharmacologic properties of this well established agent are also briefly overviewed. Discussion of the use of risperidone in patients with other PDD, in autistic pediatric patients less than 5 years of age, and in adult patients with autistic disorder is beyond the scope of this review.
2. Pharmacologic Properties
This section provides a brief overview of the pharmacologic properties of risperidone, which have been extensively reviewed previously.[10–12]
2.1 Pharmacodynamic Properties
Although the mechanism of action of risperidone is unknown, its pharmacodynamic effects are thought to be mediated via dopamine D2 and serotonin (5-HT [5-hydroxytryptamine])2A receptor antagonism.[10,13] In in vitro studies, risperidone (a benzisoxazole derivative) and its active metabolite 9-hydroxyrisperidone have similar pharmacologic activity and show high affinity for serotonin 5-HT2A receptors and dopamine D2 receptors (inhibitory constant [Ki] ≤4 nmol/L), resulting in significant inhibition of serotonin and dopamine.[10,11] Their high (Ki ≤11 nmol/L) affinity for α1 and α2 adrenergic and weak to moderate (Ki 16–670 nmol/L) affinity for other neurotransmitter receptors, including H1 histaminergic receptors, serotonin 5-HT1A, and muscarinic receptors, has also been documented.[10,13] The pharmacologic effects of risperidone may be attributed to the combined effects of risperidone plus 9-hydroxyrisperidone (section 2.2).[13]
Inhibition of dopamine D2 receptors in the brain reduces psychosis via inhibition of the mesolimbic pathway; however, dopamine deficiency in the nigrostriatal dopamine pathway and the tuberoinfundibular dopamine pathway may result in motor adverse events (e.g. extrapyramidal side effects and tardive dyskinesia) and hyperprolactinemia, respectively.[10,11,14] Different binding profiles of atypical antipsychotic agents may result in differences in their efficacy and tolerability profiles.[15] For example, in clinical trials, risperidone was associated with hyperprolactinemia (section 4), olanzapine[16] and ziprasidone[17] were associated with modest increases in serum prolactin levels (clinical significance unknown), and clozapine,[18] quetiapine,[19] and aripiprazole[20] (partial antagonist of serotonin 5-HT1A and dopamine D2 receptors and antagonist of serotonin 5-HT2A receptor) had little or no effect on serum prolactin levels.
Two theories have been proposed to explain the mechanism of action of atypical antipsychotic agents such as risperidone.[10,14,15] According to one theory, serotonin 5-HT2A receptor antagonism by antipsychotic agents results in the release of dopamine in the nigrostriatal dopamine pathway, thereby reducing motor adverse effects. Antipsychotic actions remain largely unaffected since the mesolimbic dopamine pathway has few serotonin 5-HT2A receptors.[10,14] The second theory suggests that transient occupancy of and rapid dissociation from the dopamine D2 receptors results in just enough inhibition to induce antipsychotic effects, but not to induce motor adverse events.[10,14,15,21] Thus, agents like risperidone with more potent serotonin 5-HT2A receptor antagonistic activity than affinity for dopamine D2 receptors would have fewer motor adverse events.
Antipsychotic agents, like risperidone, induce weight gain and metabolic effects such as hyperprolactinemia (section 4), which may be mediated via complex interactions between the antipsychotic agent and brain neurotransmitter receptors.[10,22] The relative affinity of the antipsychotic agents for neurotransmitter receptors may influence the magnitude of the effect, with those with low to moderate affinity (relative to haloperidol) for dopamine D2, α2 adrenergic, and serotonin 5-HT1A receptors and moderate to high affinity for histamine H1, α1 adrenergic, muscarinic, serotonin 5-HT2A, and 5-HT2C receptors being associated with excessive weight gain.[22] Thus, weight gain is moderate with risperidone and greatest with clozapine and olanzapine.[10,22]
2.2 Pharmacokinetic Properties
This section focuses on pharmacokinetic data from a trial in six autistic children (mean age 4.7 years; range 3–7 years) who received single-dose oral risperidone 0.015 or 0.03 mg/kg.[23] Where data for pediatric patients are not available, data from healthy adult volunteers[24] and from the US prescribing information (patient population not always identified)[13] are reported.
Risperidone, with or without food, is absorbed rapidly.[13,23] The mean absolute bioavailability in healthy adult volunteers was 70% after a single oral dose of risperidone 1mg.[13,24] In autistic children, peak plasma risperidone levels (Cmax) of 10 and 15 ng/mL in patients receiving single-dose risperidone 0.015 and 0.03 mg/kg were achieved ≈1 hour post dose; Cmax for the main metabolite 9-hydroxyrisperidone was reached within 1–4 hours (Cmax of 8.2 and 11.7 ng/mL for 0.015 and 0.03 mg/kg doses).[23] After correcting for dose differences these values were generally similar to those observed in adults.[23]
Following oral administration, a linear relationship between risperidone (<16mg) dose and plasma levels has been observed.[11] Steady-state levels of risperidone are reached by day 1 in extensive cytochrome P450 (CYP) 2D6 metabolizers and are expected to reach steady state in ≈5 days in poor metabolizers, whereas steady-state levels of the metabolite 9-hydroxyrisperidone are reached in 5–6 days in extensive metabolizers.[13]
Risperidone is rapidly distributed, the mean volume of distribution being 1–2 L/kg.[13] Ninety percent of risperidone and 77% of 9-hydroxyrisperidone is bound to albumin and α1-acid glycoprotein in plasma; neither agent displaces the other from plasma binding sites.[11,13]
Risperidone undergoes extensive hepatic metabolism, largely via CYP2D6-mediated hydroxylation to 9-hydroxyrisperidone, which shows similar pharmacologic activity to the parent compound (section 2.1), and to a small extent via N-dealkylation.[11,13] CYP2D6 is subject to genetic polymorphism, with 6–8% of Caucasians and a very low percentage of Asians being poor metabolizers.[13] Poor metabolizers have higher risperidone and lower 9-hydroxyrisperidone levels than extensive metabolizers; however, the single- and multiple-dose pharmacokinetics of risperidone and 9-hydroxyrisperidone combined are similar in both populations.[13,24]
In autistic children, the mean terminal half-lives of risperidone and 9-hydroxyrisperidone were ≈2 and 11–16 hours, respectively, which were 30–35% lower than those in adults.[23] The drug and its metabolites are eliminated largely via the urine and partly via the feces.[11,13] Following a single, radiolabeled, oral dose of risperidone 1mg in three healthy adult male volunteers, 70% of the dose was recovered in the urine and 14% in the feces.[11,13]
Patients with moderate to severe renal impairment showed a 60% reduction in the clearance of risperidone and 9-hydroxyrisperidone relative to healthy young subjects, consequently a dosage reduction is recommended in these patients.[13] Dosage reduction is also recommended in patients with hepatic impairment since reduced levels of albumin and α1-acid glycoprotein in these patients results in a 35% increase in the mean free fraction of risperidone.[13] Although no study has evaluated the effect of gender or race on the pharmacokinetics of risperidone, data from a population pharmacokinetic analysis suggest that these factors may not affect the pharmacokinetic profile of the drug.[13]
Pharmacokinetics of risperidone may be affected by coadministration of CYP2D6 and/or CYP3A4 inhibitors (e.g. quinidine, clozapine, fluoxetine, and paroxetine) which may interfere with the conversion of risperidone to 9-hydroxyrisperidone, or by the coadministration of inducers (e.g. carbamazepine, phenytoin, and rifampin [rifampicin]) which may decrease the combined plasma concentrations of the drug and its metabolite.[10,13] For example, coadministration of carbamazepine reduced the steady-state plasma concentrations of risperidone and 9-hydroxyrisperidone by ≈50%.[13] Drugs metabolized by other CYP isoenzymes including 1A1, 1A2, 2C9, and 2C19 may also weakly inhibit risperidone metabolism.[13]
Additionally, cimetidine and ranitidine increase the bioavailability of risperidone by 64% and 26%; ranitidine also increased the area under the plasma concentration-time curve of risperidone plus 9-hydroxyrisperidone by 20%.[13] In vitro studies suggest that risperidone is a weak inhibitor of CYP2D6 and is not expected to significantly affect the pharmacokinetics of drugs metabolized by the isoenzyme (e.g. donepezil and galantamine).[13] The pharmacokinetics of valproate semisodium are not affected by concomitant administration of risperidone.[10,13]
3. Therapeutic Efficacy
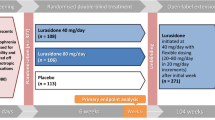
The clinical efficacy of oral risperidone for the treatment of irritability in autistic children and adolescents has been evaluated in two 8-week well designed trials[25,26] and a prespecified longer-term, open-label extension and double-blind, placebo-controlled, discontinuation trial[27] of one[26] of these trials (table I; see table for dosage and design details). All data from these trials and subgroup analyses of the data are published in full.
Efficacy of oral risperidone (RIS) in children and adolescents with autistic disorder. Summary of 8-week, randomized, double-blind, multicenter trials[25,26] and a 6-month, open-label extension (4 months’ duration) and double-blind, discontinuation (2 months’ duration) trial[27] of one[26] of these trials. Patients (pts) were aged 5–12 (mean age ≈7 years)[25] or 5–17 years (mean age 8.8[26] or 8.6[27] years). All analyses were based on the modified intent-to treat population (i.e. those who received at least one dose of study drug and had a baseline and ≥1 post-baseline assessment)
Participants were aged 5–12 (mean age ≈7 years)[25] or 5–17 years (mean age 8.8[26] or 8.6[27] years). All patients met the Diagnostic and Statistical Manual-IV criteria for autistic disorder;[25–27] other inclusion criteria were a score of ≥30 (i.e. at least mild autistic disorder) on the Childhood Autism Rating Scale,[25] having significant tantrums, aggression, self-injurious behavior and/or agitation,[26,27] weighing ≥15 kg,[26,27] and having a mental age of ≥18 months.[26,27] Exclusion criteria included the presence of a psychiatric disorder[25–27] or significant medical problems,[26,27] patients who had had a seizure within the previous 3 months,[25] and those receiving treatment with psychotropic medication other than anticonvulsants for seizure control, where the patient had been on a stable dose of anticonvulsant for ≥4 weeks and had not had a seizure in the previous 6 months.[26,27] There were no between-group differences in baseline characteristics in individual trials, including mean scores on the parent-rated Aberrant Behavior Checklist (ABC) subscales, with the exception of the score for inappropriate speech subscale in one trial[26] (4.8 in risperidone group vs 6.5 in placebo group; p = 0.03) and, in another study,[25] more patients in the placebo group had an intelligence quotient above 84 (0% vs 25% in the placebo group; p = 0.02).
In the Research Units of Pediatric Psychopharmacology Autism Network (RUPP) trial,[26] after 8 weeks of double-blind treatment, children who met the predefined criteria for a response in the risperidone group, and those in the placebo group who showed no improvement in their behavior, were eligible to enroll in a 4-month extension phase of open-label treatment with risperidone, followed by a 2-month placebo-controlled discontinuation phase. A positive response was defined as showing a 25% reduction in the ABC-Irritability Subscale (ABC-IS) and a rating of ‘much improved’ or ‘very much improved’ on the Clinical Global Impression improvement (CGI-I) scale, as assessed by a blinded investigator.[27] Relapse during the discontinuation phase was defined as a 25% increase in the ABC-IS and, on at least 2 consecutive weeks, a CGI-I rating of ‘much worse’ or ‘very much worse’ compared with the prediscontinuation baseline, as assessed by a blinded investigator.[27]
The primary efficacy measure in all trials was the change from baseline in the ABC-IS score.[25–27] In addition, in the longer-term trial,[27] ratings in the clinician-rated CGI-I scale were a coprimary endpoint. All analyses were based on the modified intent-to-treat population (i.e. those who received at least one dose of study drug and had a baseline and ≥1 post-baseline assessment). A mixed-effect linear regression model was used in analyses of ABC subscale data (see table I for further details);[25,26] in the RUPP trial,[26] analyses were adjusted for multiple comparisons using Bonferroni correction. Effect size was determined using Cohen’s standardized difference in means.
3.1 Short-Term Trials
After 8 weeks’ treatment, patients receiving risperidone experienced significantly greater improvements in mean ABC-IS scores than those in the placebo group (primary endpoint), with a 56.9%[26] and 65.0%[25] decrease from baseline in the mean score in risperidone groups (table I). In addition, there were also significantly greater improvements from baseline for some of the other ABC subscale mean scores in the risperidone than in placebo groups (secondary endpoints) [table I].
Relative to placebo, a significantly higher proportion of patients receiving risperidone achieved a positive response in both short-term trials.[25,26] In the RUPP trial,[26] a positive response occurred in 69% of patients in the risperidone group versus 12% of those in the placebo group (p < 0.001), with respective positive response rates in the other trial of 58.3% and 21.4% (p = 0.04).[25]
Several other prespecified secondary efficacy measures for assessing behavioral symptoms also generally favored risperidone treatment. For example, in the RUPP trial, the behavior of a significantly (p < 0.001) higher proportion of children and adolescents in the risperidone than in the placebo group was rated as ‘much improved’ or ‘very much improved’ on the CGI-I scale after 4 (60% vs 16% in the placebo group; data estimated from graph) and 8 weeks (75.5% vs 11.5%).[26] There were significantly greater improvements in the parent-rated Nisonger Child Behavior Rating Form (N-CBRF) for the categories of conduct problem, hyperactive, and overly sensitive subscale scores in those receiving risperidone in the other trial (figure 1).[25] However, there were no between-group differences for mean changes in various behavioral symptom scores on the visual analog scale for the most troublesome symptoms (lower scores indicate fewer symptoms) in this smaller study, with the exception of a significantly (p < 0.05) greater improvement from baseline in mean score for hyperactivity in the risperidone than in the placebo group (39.7 vs 80.5 at study end; baseline values 68.7 vs 96.3).
Efficacy of risperidone (RIS) in children and adolescents with autistic disorder. Changes in Nisonger-Child Behavior Rating Form categories after 8 weeks of RIS (25 or 26 patients per category) or placebo (PL; 26 or 28 patients per category) treatment in a randomized, double-blind, multicenter trial.[25] Reductions from baseline (b/line; values given in brackets) represent an improvement; see table I for dosage and design details. * p < 0.05, ** p = 0.005 vs PL.
Patients in the risperidone group also generally showed greater improvements in repetitive behavior and measures of relatedness and impaired communication than those in the placebo group in prespecified secondary analyses in the modified intent-to-treat population of the RUPP trial.[28] These endpoints were assessed using the parent-rated modified Ritvo-Freeman Real Life Rating Scale (RFRLRS) for children with autistic disorder, which assesses social relationship to people and language, the validated clinician-rated Children’s Yale-Brown Obsessive Compulsive Scale (CYBOCS), and the clinician-rated Maladaptive Behavior Domain of Vineland Adaptive Behavior Scales (MBD-VABS), which assesses symptoms such as mood- and anxiety-related symptoms (part 1), and more severe symptoms such as psychosis, self-injury, and property destruction (part 2). Compared with placebo, mean overall scores for RFRLRS and those for the sensory motor behaviors, affectual reactions, and sensory responses subscales were all significantly (p ≤ 0.004) improved from baseline at study end. For example, mean overall scores in the risperidone group were reduced from 0.94 at baseline to 0.54 at 4 weeks and 0.45 at 8 weeks, whereas respective values in the placebo group were 1.03, 0.84, and 0.88. There was no between-group difference for social relationship to people and language subscales of the RFRLRS. For the CYBOCS, the mean score decreased by approximately 4 points (15.51 at baseline to 11.65 at study end) in the risperidone group compared with an approximately 1 point reduction in the placebo group (15.18 vs 14.21), with a significant (p = 0.005) interaction between study group and time. Furthermore, there were also significantly (p ≤ 0.02) greater reductions from baseline in overall, part 1, and part 2 MBD-VABS scores in the risperidone than in the placebo group. For example, overall scores in the risperidone group were reduced from 33.26 to 20.34 versus a reduction from 33.51 to 30.27 in the placebo group (p < 0.001), with an effect size of 1.03 at study end.[28]
Risperidone treatment does not appear to significantly affect the nutritional balance of children and adolescents with autistic disorder, based on a pilot study[29] of 20 patients who participated in the RUPP trial. Based on the quantitative Food Frequency Questionnaire, there was high interpatient variability in macronutrient, vitamin, and mineral intake at baseline, with mean intakes exceeding the Dietary Reference Intakes. In evaluable patients, weight (increased by 3.7 vs 1.6kg) and vitamin K intake (increased by 19μg vs a decrease of 16μg) altered to a significantly (p < 0.05) greater extent in the risperidone than in the placebo group after 8 weeks of treatment. There were no significant changes in nutrient intake during the extension phase of this trial. It should be noted that this subgroup study was initiated part way through the RUPP trial and thus, there is potential for bias due to the small sample size; the sample size was also too small to determine whether there was a potential relationship between nutritional intake and risperidone-related weight gain (section 4).[29]
Parent-rated targeted symptoms (i.e. symptoms of the most concern to patient/caregiver) were reduced to a greater extent in the risperidone than in the placebo group in the RUPP trial (2.8 vs 4.5 points; p < 0.001), with 94 caregivers participating in this consumer-orientated subanalysis.[30] The key concerns of caregivers, the most common of which were tantrums, aggression, and hyperactivity, were collected at baseline, 4, and 8 weeks, with blinded clinical investigators rating the change from baseline on a 9-point scale (0 = normalized, 5 = unchanged, 9 = disastrous). Interestingly, ratings from this 9-point scale significantly (p < 0.001) correlated with the ABC-IS (primary endpoint) and CGI-I scores at 8-week assessment, with an effect size of 1.4 on the 9-point scale and 1.2 on the ABC-IS. [30]
3.2 Longer-Term Trial
The beneficial effects of risperidone therapy on behavioral symptoms in children and adolescents with autistic disorder were maintained during the extension phase of the RUPP trial, according to the coprimary endpoint of mean change from baseline in ABC-IS score (table I).[27] Although the ABC-IS score showed a statistically significant deterioration from baseline, this minor deterioration was not considered clinically relevant. Compared with baseline, the majority of patients (82.5%; 52 of 63 patients) had a rating of ‘much improved’ or ‘very much improved’ on the CGI-I scale at study end (coprimary endpoint). The total duration of treatment was 6 months in those initially randomized to risperidone and 4 months for those initially receiving placebo, with 81% of patients completing the open-label extension phase. There was very little change in the mean risperidone dosage over the extension phase (mean dosage initially 1.80 vs 2.08 mg/day at study end).[27]
The efficacy of risperidone treatment in the management of behavioral symptoms in autistic children and adolescents was also maintained according to secondary endpoints.[27,28] There was no change from the baseline score for most of the secondary subscale parameters of the ABC, with the exception of the mean stereotypic behavior subscale score, which increased slightly indicating that there was a deterioration in this behavior (table I).[27] There was also no significant change from baseline in mean RFRLRS, CYBOCS, and MBD-VABS scores during the extension phase.[28]
Furthermore, patients receiving risperidone showed significant (p < 0.01) improvements in adaptive behavior for areas of communication, daily living skills, and socialization in the RUPP trial.[31] Based on baseline socialization growth rates, children and adolescents experienced a >6% improvement beyond that expected in the area of socialization, with patients gaining an average of 7.8 age-equivalent months.
During the placebo-controlled discontinuation phase, significantly fewer patients in the risperidone-treatment than in the placebo-treatment group relapsed (12.5% vs 62.5%; p = 0.01), as assessed in an interim per-protocol analysis conducted after 32 patients had completed treatment.[27] Moreover, the median time to relapse was significantly longer for those continuing to receive risperidone during this discontinuation phase (57 vs 34 days; p = 0.009 in log rank test). During the discontinuation phase, the median dosage of risperidone was decreased by 25% per week for those in the placebo group. On the basis of results from this planned interim analysis, the discontinuation phase was stopped earlier than planned.[27]
4. Tolerability
Risperidone (≤6 months’ treatment) had a clinically manageable tolerability profile in children and adolescents with autistic disorder who participated in clinical trials discussed in section 3.[25–27] Most treatment-emergent adverse events were of mild to moderate severity, with most resolving spontaneously or being effectively managed with dosage adjustments.[25,26] Very few patients (one risperidone recipient and one placebo recipient) in the two 8-week trials discontinued treatment due to an adverse event.[13]
Pooled descriptive analysis reported in the US prescribing information[13] indicated that the most common treatment-emergent adverse events (i.e. those occurring in >10% of patients receiving risperidone [n = 76] and at a rate that was at least twice that in the placebo group [n = 80]) were somnolence (67% vs 23%), increased appetite (49% vs 19%), fatigue (42% vs 13%), upper respiratory tract infection (34% vs 15%), increased saliva (22% vs 9%), constipation (21% vs 8%), dry mouth (13% vs 6%), tremor (12% vs 1%), and dystonia (12% vs 0%).[13] Treatment-emergent adverse events that occurred in significantly more patients in the risperidone than in the placebo group in the RUPP trial are presented in figure 2.[26]
Tolerability profile of oral risperidone (RIS) in children and adolescents with autistic disorder. Incidence of treatment-emergent adverse events that occurred significantly more frequently in the RIS (n = 49) than in the placebo (PL; n = 51) group in the 8-week, randomized, double-blind RUPP trial.[26] The occurrence of adverse events was reported at each visit, based on the clinician’s enquiries and a 32-item questionnaire given to the patient/caregiver. See table I for dosage and design details and trial acronym. p-Values that were <0.10 were considered statistically significant, as determined by chi-square test with Yates’ correction. * p < 0.10, ** p ≤ 0.01, *** p < 0.001 vs PL.
Somnolence, the most frequently reported adverse event in autistic children and adolescents, was generally of mild to moderate severity (96% of cases), with the highest incidence occurring during the first 2 weeks of risperidone treatment.[13] It was usually transient in nature, with a median duration of 16 days. Dosage modification may be beneficial in those with persistent somnolence, with the total daily dose adjusted, given once daily at bedtime, or as a divided dose (section 5).[13]
There was a higher incidence of adverse events reflecting extrapyramidal symptoms (EPS) in the risperidone than in the placebo groups in a pooled analysis of the two 8-week clinical trials (27.6% vs 10.0%).[13] In addition, in the larger RUPP trial,[26] there was a significant between-group difference in the incidence of tremor (figure 2). The severity of these EPS was assessed using the objective Simpson-Angus Rating Scale (SARS),[26] Abnormal Involuntary Movement Scale (AIMS),[26] and the Extrapyramidal Symptom Rating Scale (ESRS).[25] Pooled data indicate that the mean reduction from baseline to study end in ESRS was 0.3 in the risperidone group versus 0.4 in the placebo group, with the median change in both groups being zero.[13] In the RUPP trial, there was no change in AIMS and SARS scores in autistic children and adolescents receiving risperidone for up to 6 months.[32] In clinical trials, tardive dyskinesia occurred in 2 of 1885 children and adolescents with autistic disorder or other psychiatric disorders receiving risperidone, with these cases resolving upon discontinuation of treatment.[13]
Risperidone treatment was associated with weight gain in short- and longer-term trials discussed in section 3,[26,27] with these increases being in excess of developmentally expected norms.[33] According to the US prescribing information,[13] weight gain occurred in 9% of patients receiving risperidone and in none of those receiving placebo in a pooled analysis of the two 8-week trials discussed in section 3. The RUPP trial reported a significantly higher weight gain in the risperidone than in the placebo group (mean increase 2.7 vs 0.8kg; p < 0.001).[26] Of note, there was no correlation between serum leptin levels and weight gain in 63 children and adolescents with autistic disorder receiving up to 6 months’ risperidone treatment in the RUPP trial.[33] In long-term, open-label trials in patients with autistic disorder or psychiatric disorders, the mean increase in weight after 12 months’ risperidone treatment was 7.5kg, which was higher than the predicted normal weight gain of approximately 3–3.5kg per year adjusted for age.[13]
As is the case with adults, risperidone treatment was associated with elevated serum prolactin levels in children and adolescents, with 49% of children and adolescents receiving risperidone experiencing elevated serum prolactin levels in double-blind clinical trials compared with 2% of those receiving placebo.[13,34] In the RUPP trial, [35] there was no between-group difference in serum prolactin levels at baseline (9.3 ng/mL in risperidone [n = 42] and placebo [n = 36] groups). However, after 8 weeks, serum prolactin levels were significantly higher in the risperidone than in the placebo group (39.0 vs 10.1 ng/mL; p < 0.001), with levels remaining elevated relative to baseline at the end of ≤6 months’ risperidone treatment (32.4 ng/mL; p < 0.001; n = 43) and at 22 months’ follow-up (25.3 ng/mL; p < 0.001; n = 30). The 2- to 4-fold elevation in levels of serum prolactin reported in autistic children and adolescents at these two timepoints did not appear to be associated with adverse effects in this study.[35] However, galactorrhea, amenorrhea, gynecomastia, and impotence have been reported in patients receiving prolactin-elevating compounds.[13] When long-standing hyperlactinemia is associated with hypogonadism, patients of both genders may experience a decrease in bone density.[13]
The long-term effects of risperidone on growth and sexual maturation remain to be fully evaluated.[13] In a retrospective analysis of pooled data from five clinical trials in 572 evaluable children (aged 5–15 years) with disruptive behavior disorders receiving risperidone for up to 1 year, there were no statistically significant or clinically relevant effects on growth or the onset or progression of puberty.
Although there were no reports of hyperglycemic episodes in participants in clinical trials discussed in section 3, as with all atypical antipsychotic agents, epidemiologic studies suggest that there is an increased risk of treatment-emergent hyperglycemia-related adverse events in patients receiving risperidone, with case reports of hyperglycemia (some of which were associated with ketoacidosis or hyperosmolar coma or death).[13]
5. Dosage and Administration
Risperidone is approved in the US for the treatment of irritability associated with autistic disorder in children and adolescents aged 5–16 years.[13] The recommended dosages of risperidone in these patients are summarized in table II. Based on clinical trial data, the effective dosage range of risperidone is 0.5–3.0 mg/day. Caution is advised in children weighing <15 kg.[13] To achieve an optimal balance between efficacy and safety, a gradual lowering of the dosage should be considered after a sufficient clinical response has been achieved and maintained; risks and benefits should be periodically re-evaluated during long-term therapy. Risperidone is also approved in the US for the treatment of schizophrenia in adolescents aged 13–17 years and, as monotherapy, for the short-term treatment of acute manic and mixed episodes associated with bipolar I disorder in children and adolescents aged 10–17 years; in depth discussion of these indications is beyond the scope of this review.[13]
Recommended dosages of risperidone for autistic children and adolescents aged 5–16 years[13]
In patients experiencing persistent somnolence, risperidone may be administered once daily at bedtime or administered as a divided dose twice daily, or the dosage may be reduced.[13] The dosage of risperidone should be titrated when administered concomitantly with CYP2D6 inhibitors or inducers (see section 2.2). Dosage reduction is also recommended in patients with hepatic impairment or moderate to severe renal impairment (see section 2.2).[13]
Local manufacturer’s prescribing information should be consulted for comprehensive dosage and administration guidelines.
6. Place of Risperidone in the Treatment of Irritability Associated with Autistic Disorder in Children and Adolescents
The management of autistic disorder is very challenging, given the heterogeneity of the condition and the high prevalence of coexisting morbidities (e.g. fragile X syndrome, epilepsy, and tuberous sclerosis), and requires an individualized multidisciplinary approach that takes into consideration the needs of both the patient and their caregiver.[9,36–38] Although behavioral and educational programs are the mainstay of treatment, in many instances pharmacologic intervention with psychotropic medications may be necessary for managing severe behavioral symptoms that compound the clinical features of autistic disorder.[37] In addition to minimizing severe behavioral symptoms, such as aggression, irritability, and self-harm, medical interventions may also facilitate access to developmental, educational, habilitative, and behavioral therapies and, for many patients, will be an integral part in the management of autistic disorder.[36]
Medical treatments also have a role to play in the management of comorbid psychiatric disorders, such as mood disorder, anxiety, and obsessive-compulsive disorders, that are commonly associated with autism spectrum disorders, including autistic disorder.[36] Selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine and fluvoxamine, have proven beneficial in the management of this type of comorbidity, with some evidence also indicating that they may improve behavior, language, cognition, and social relatedness.[7,36] However, to date, there have been no systematic reviews or randomized controlled trials comparing SSRIs with placebo in children with autistic disorder; thus, the position of these agents in the management of behavioral symptoms in children and adolescents remains to be fully determined.[4,7] SSRIs are generally well tolerated and have a better tolerability profile than typical and atypical antipsychotic agents. Adverse events associated with SSRI treatment, albeit that these are relatively uncommon, include restlessness, hyperactivity, agitation, and insomnia.[36]
Pharmacologic management in autistic patients also requires careful consideration of potential pharmacokinetic drug interactions between concommitantly administered agents, with many of the coadministered agents being metabolized by and/or inducers of CYP isoenzymes. For instance, anticonvulsant agents are commonly used in the management of comorbidity in autistic patients, with a significant minority of autistic patients developing epilepsy (section 1). Many anticonvulsant agents (e.g. carbamazepine and phenytoin), are metabolized by and/or induce CYP isoenzymes; hence, the concomitant use of risperidone with these agents (section 2.2), as is the case with some other atypical antipsychotics (e.g. aripiprazole, olanzapine), requires monitoring of plasma levels and/or dosage adjustment of risperidone, particularly during the initiation or discontinuation of concomitant treatment.
Of note, there are currently no specific guidelines for the medical management of severe behavioral symptoms in children and adolescents with autistic disorder, with no one medication having been shown to consistently benefit these patients.[36,39] Up until 10 years ago there was very little clinical trial evidence to support the safety and efficacy of the various pharmacotherapies that were being used in the management of behavioral symptoms in autistic disorder, with their use based on ‘off-label’ treatment.[39–41] In addition to showing efficacy in children and adolescents with autistic disorder (section 3), risperidone has also shown efficacy in those with other PDD in an 8-week, randomized, double-blind, placebo-controlled trial,[42] although discussion of studies in patients with other PDD is beyond the scope of this review. The newer atypical antipsychotic agents aripiprazole and ziprasidone have also shown promise in small trials in patients with PDD, with more robust data required before the position of these agents in the management of autistic disorder and other PDD may be determined.[39] On the other hand, recent limited clinical trial experience has failed to support the efficacy of the atypical antipsychotic quetiapine[7,39] and that of the polypeptide secretin[7,40,41] in children with autistic disorder. To date, there have been no controlled clinical trials evaluating clozapine in this patient population;[7,39] moreover, the propensity for clozapine to cause seizures and agranulocytosis places considerable limitations on the potential of this agent in the management of behavioral symptoms in autistic disorder and other PDD.[7] Similarly, efficacy data relating to the use of olanzapine is extremely limited and robust data are required before its relative position in the management behavioral symptoms associated with autistic disorder may be determined.[7,8,39] At this time, no head-to-head clinical trials comparing antipsychotic agents have been conducted in children and adolescents with autistic disorders.
The greatest body of evidence from clinical trials supporting the use of medical interventions relates to the use of the typical (namely haloperidol) and atypical (namely risperidone) antipsychotic agents.[36] As discussed earlier in section 1, the high incidence of dyskinesias associated with haloperidol treatment, places limitations on the use of this agent, with its use reserved for the most severely symptomatic patients.[7] Therefore, focus has turned to the use of atypical antipsychotic agents, particularly risperidone, for the management of severe behavioral symptoms in children and adolescents with autistic disorder. Currently this is the only atypical antipsychotic approved by the US FDA for use in children and adolescents for the treatment of irritability associated with autistic disorders.
In two well designed, 8-week, clinical trials in children and adolescents, risperidone treatment provided better efficacy than placebo treatment for the management of behavioral symptoms, including improvements in the mean ABC-IS (primary endpoint) and other ABC subscale scores (section 3.1). Other secondary endpoints also generally favored risperidone treatment in one or both of these short-term trials, including the higher proportion of patients achieving a positive response, and improvements in scores for RFRLRS, CYBOCS, MBD-VABS, and some subscales of the N-CBRF (section 3.1). The benefits, in terms of mean ABC-IS scores (no clinically relevant change) and clinician-rated CGI-I scores (coprimary endpoints), were maintained in a 6-month, open-label extension and double-blind, discontinuation trial of one of these short-term trials (section 3.2). Secondary endpoints also indicated that the efficacy of risperidone treatment was maintained in the longer term (section 3.2). The efficacy of risperidone in children under 5 years of age has not been established, with data limited to a small (n = 24) randomized, double-blind trial (discussion of which is beyond the scope of this review);[43] thus, its use in these pediatric patients is not recommended.
Medical treatments for behavioral symptoms in children and adolescents with autistic disorder will depend upon the benefit-risk profile of each individual agent. Risperidone had a clinically manageable tolerability profile in this patient population in short- and longer-term trials of up to 6 months’ duration, with most adverse events being of mild to moderate severity and resolving spontaneously or being clinically manageable with dosage adjustments (section 4). There are issues relating to increased appetite, weight gain and somnolence that require consideration prior to and during risperidone treatment, as they do with some other atypical antipsychotic agents (e.g. olanzapine). In addition, as with all atypical antipsychotic agents, epidemiologic studies suggest that there is an increased risk of treatment-emergent hyperglycemia-related adverse events in patients receiving risperidone, with case reports of hyperglycemia (some of which were associated with ketoacidosis or hyperosmolar coma or death);[13] hence, patients receiving atypical antipsychotic agents should be monitored for signs of hyperglycemia and those with diabetes mellitus or known to have risk factors for the disease should have regular monitoring of blood glucose levels.[13,16–20] Notably, the incidence of tardive dyskinesia appeared to be very low in a pooled analysis of approximately 1800 children and adolescents with autistic disorder and other psychiatric disorders (section 4).[13] The long-term safety of risperidone, including the potential effects on growth and sexual maturation, and of hyperprolactinemia,[44] in children and adolescents with autistic disorder remain to be fully determined.
In conclusion, oral risperidone treatment was better than placebo treatment in reducing irritability and other behavioral symptoms associated with autistic disorder in children and adolescents in two well designed short-term trials, with these benefits maintained in those receiving risperidone for up to 6 months. The drug had a clinically manageable tolerability profile, with most adverse events being of mild to moderate intensity. There are some aspects of treatment, such as weight gain, somnolence, and hyperglycemia, that require monitoring, and the long-term safety of risperidone in children and adolescents with autistic disorder remains to be fully determined. With these issues in mind, risperidone offers a valuable emerging option for the treatment of irritability associated with autistic disorder in children and adolescents.
Disclosure
During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on this article; changes based on any comments were made on the basis of scientific and editorial merit.
Notes
The use of trade names is for product identification purposes only and dose not imply endorsement.
References
Fombonne E. Epidemiology of autistic disorder and other pervasive developmental disorders. J Clin Pyschiatry 2005; 66Suppl. 10: 3–8
Filipek PA, Accardo PJ, Ashwal S, et al. Practice parameter: screening and diagnosis of autism: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society [online]. Available from URL: http://www.neurology.org/misc/reprints.shtml [Accessed 2007 Sep 3]
Scahill L, Koenig K, Carroll DH, et al. Risperidone approved for the treatment of serious behavioral problems in children with autism. J Child Adolesc Psychiatric Nurs 2007; 20(3): 188–90
Parr J. Autism. Clin Evid 2005; 14: 275–84
Rapin I. The autistic-spectrum disorders. N Engl J Med 2002; 347(5): 302–3
Morgan S, Taylor E. Antipsychotic drugs in children with autism. BMJ 2007; 334(7603): 1069–70
Posey DJ, McDougle CJ. The pharmacotherapy of target symptoms associated with autistic disorder and other pervasive developmental disorders. Harv Rev Psychiatry 2000; 8(2): 45–63
Barnard L, Young AH, Pearson J, et al. A systematic review of the use of atypical antipsychotics in autism. J Psychopharmacol 2002; 16(1): 93–101
Jesner OS, Aref-Adib M, Coren E. Risperidone for autism spectrum disorder. Cochrane Database Syst Rev 2007; (3): CD005040
Fenton C, Scott LJ. Risperidone: a review of its use in the treatment of bipolar mania. CNS Drugs 2005; 19(5): 429–44
Bhana N, Spencer CM. Risperidone: a review of its use in the management of the behavioural and psychological symptoms of dementia. Drugs Aging 2000; 16(6): 451–71
Swainston Harrison T, Goa K. Long-acting risperidone: a review of its use in schizophrenia. CNS Drugs 2004; 18(2): 113–32
L.P. Janssen. Risperdal® (risperidone): US prescribing information [online]. Available from URL: http://www.risperdal.com/risperdal/shared/pi/risperdal.pdf [Accessed 2007 Sep 24]
Stahl S. Describing an atypical antipsychotic: receptor binding and its role in pathophysiology. Primary Care Companion to J Clin Psychiatry 2003; 5Suppl. 3: 9–13
Schotte A, Janssen PFM, Gommeren W, et al. Risperidone compared with new and reference antipsychotic drugs: in vitro and in vivo receptor binding. Psychopharmacology 1996; 124(1-2): 57–73
Eli Lilly and Company. Zyprexa® (olanzapine tablets): US prescribing information [online]. Available from URL: http://pi.lilly.com/us/zyprexa-pi.pdf [Accessed 2007 Sep 24]
Pfizer. Geodon® (ziprasidone HCL) capsules: US prescribing information [online]. Available from URL: http://www.fda.gov/cder/foi/label/2007/020825s024,020919s0141bl.pdf [Accessed 2007 Sep 24]
Novartis. Clozaril® (clozapine) tablets: US prescribing information [online]. Available from URL: http://www.pharma.us.novartis.com/product/pi.jsp#C [Accessed 2007 Sep 24]
AstraZeneca. Seroquel® (quetiapine fumarate) tablets: US prescribing information [online]. Available from URL: http://www.astrazeneca-us.com/pi/seroquel.pdf [Accessed 2007 Sep 24]
Bristol-Myers Squibb Company. Abilify® (aripiprazole) tablets, Abilify® Discmelt™ (aripiprazole) orally disintegrating tablets and Abilify® (aripiprazole) oral solution: US prescribing information [online]. Available from URL: http://www.fda.gov/cder/foi/label/2006/021436s013,021713s008,021729s0011bl.pdf [Accessed 2007 Sep 24]
Kapur S, Seeman P. Does fast dissociation from the dopamine D2 receptor explain the action of atypical antipsychotics?: a new hypothesis. Am J Psychiatry 2001; 158(3): 360–9
Baptista T, Kin NMKNY, Beaulieu S, et al. Obesity and related metabolic abnormalities during antipsychotic drug administration: mechanisms, management and research perspectives. Pharmacopsychiatry 2002; 35(6): 205–19
Casaer P, Walleghem D, Vandenbussche I, et al. Pharmacokinetics and safety of risperidone in autistic children [abstract no. 29]. Pediatr Neurol 1994; 11(2): 89
Heykants J, Huang ML, Mannens G, et al. The pharmacokinetics of risperidone in humans: a summary. J Clin Psychiatry 1994; 55(5 Suppl.): 13–7
Pandina GJ, Bossie CA, Youssef E, et al. Risperidone improves behavioral symptoms in children with autism in a randomized, double-blind, placebo-controlled trial. J Autism Dev Disord 2007; 37(2): 367–73
McCracken JT, McGough J, Shah B, et al. Risperidone in children with autism and serious behavioral problems (Research Units of Pediatric Psychopharmacology Autism Network). N Engl J Med 2002; 347(5): 314–21
Risperidone treatment of autistic disorder: longer-term benefits and blinded discontinuation after 6 months (Research Units on Pediatric Psychopharmacology Autism Network). Am J Psychiatry 2005; 162(7): 1361–9
McDougle CJ, Scahill L, Aman MG, et al. Risperidone for the core symptom domains of autism: results from the study by the Autismn Network of the Research Units on Pediatric Psychopharmacology. Am J Psychiatry 2005; 162(6): 1142–8
Lindsay RL, Arnold LE, Aman MG, et al. Dietary status and impact of risperidone on nutritional balance in children with autism: a pilot study. J Intellect Dev Disabil 2006; 31(4): 204–9
Arnold LE, Vitiello B, McDougle C, et al. Parent-defined target symptoms respond to risperidone in RUPP autism study: customer approach to clinical trials. J Am Acad Child Adolesc Psychiatry 2003; 42(12): 1443–50
Williams SK, Scahill L, Vitiello B, et al. Risperidone and adaptive behavior in children with autism. J Am Acad Child Adolesc Psychiatry 2006; 45(4): 431–9
Aman MG, Arnold LE, McDougle CJ, et al. Acute and long-term safety and tolerability of risperidone in children with autism. J Child Adolesc Psychopharmacol 2005; 15(6): 869–84
Martin A, Scahill L, Anderson GM, et al. Weight and leptin changes among risperidone-treated youths with autism: 6-month prospective data. Am J Psychiatry 2004; 161(6): 1125–7
Dunbar F, Kusumakar V, Daneman D, et al. Growth and sexual maturation during long-term treatment with risperidone. Am J Psychiatry 2004; 161(5): 918–20
Anderson GM, Scahill L, McCracken JT, et al. Effects of short- and long-term risperidone treatment on prolactin levels in children with autism. Biol Psychiatry 2007; 61(4): 545–50
American Academy of Pediatrics Committee on Children with Disabilities. Technical report: the pediatrician’s role in the diagnosis and management of autistic spectrum disorder in children. Pediatrics 2001; 107(5): 1–18
Filipek PA, Steinberg-Epstein R, Book TM. Intervention for autistic spectrum disorders. Neurotherapeutics 2006; 3(2): 207–16
American Academy of Child and Adolescent Psychiatry. Summary of the practice parameters for the assessment and treatment of children, adolescents, and adults with autism and other pervasive developmental disorders. J Am Acad Child Adolesc Psychiatry 1999; 38(12): 1611–5
Chavez B, Chavez-Brown M, Sopko MA, et al. Atypical antipsychotics in children with pervasive developmental disorders. Pediatr Drugs 2007; 9(4): 249–66
Lilienfeld SO. Scientifically unsupported and supported interventions for childhood psychopathology: a summary. Pediatrics 2005; 115(3): 761–4
Volkmar FR, Pauls D. Autism. Lancet 2003; 362(9390): 1133–41
Shea S, Turgay A, Carroll A, et al. Risperidone in the treatment of disruptive behavioral symptoms in children with autistic and other pervasive developmental disorders. Pediatrics 2004; 114(5): e634–41
Luby J, Mrakotsky C, Stalets MM, et al. Risperidone in preschool children with autistic spectrum disorders: an investigation of safety and efficacy. J Child Adolesc Psychopharmacol 2006; 16(5): 575–87
Haddad PM, Wieck A. Antipsychotic-induced hyperprolactinaemia: mechanisms, clinical features and management. Drugs 2004; 64(20): 2291–314
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: B. Chavez, Ernest Mario School of Pharmacy, Rutgers State University of New Jersey, Piscataway, New Jersey, USA; B. Coffey, Department of Child and Adolescent Psychiatry, New York University Child Study Center, Institute for Tourette and Tic Disorders, New York School of Medicine, New York, New York, USA; J.A. Hellings, Department of Psychiatry, University of Kansas Medical Center, Kansas City, Kansas, USA; C. Prakash, Auckland District Health Board, St. Lukes Community Mental Health Centre, Auckland, New Zealand; A. Sandler, Olson Huff Center, Mission Children’s Hospital, Asheville, North Carolina, USA.
Data Selection
Sources: Medical literature published in any language since 1980 on ‘risperidone’, identified using MEDLINE and EMBASE, supplemented by AdisBase (a proprietary database of Wolters Kluwer Health | Adis). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the manufacturer.
Search strategy: MEDLINE, EMBASE and AdisBase search terms were ‘risperidone’ and ‘autism’. Searches were last updated 24 September 2007.
Selection: Studies in children and adolescents with autistic disorder who received risperidone. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Risperidone, atypical antipsychotic, autistic disorder, pharmacodynamics, pharmacokinetics, therapeutic use tolerability.
Rights and permissions
About this article
Cite this article
Scott, L.J., Dhillon, S. Risperidone. Pediatr-Drugs 9, 343–354 (2007). https://doi.org/10.2165/00148581-200709050-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00148581-200709050-00006