Abstract
Objective: The aim of this study was to investigate the analgesic efficacy of Neodolpasse®, a fixed-dose combination of orphenadrine and diclofenac, compared with those of its single active ingredients in a human pain model.
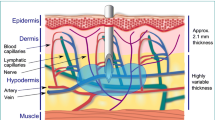
Methods: The study was designed as a randomised, double-blind, placebo-controlled, four-period crossover study. Twenty-four healthy female and male subjects received single infusions of Neodolpasse®, orphenadrine, diclofenac or saline solution over 60 minutes. Infusions were separated by a 1-week washout period. Neurogenic inflammation and hyperalgesia were induced by topical occlusive application of a 1% capsaicin solution for 30 minutes on defined skin areas on the back. The pain response to CO2 laser pulses applied to the capsaicin- pretreated skin was measured by event-related vertex EEG recordings. This allowed us to study the influence of a single infusion on the central P2- and peripheral N1-components of laser-induced somatosensory-evoked potentials (LSEP) as a measure of pain response.
Results: Although none of the active treatments had a significant effect on the peripheral N1-component, all active treatments reduced the P2-component of the LSEP, reflecting central/spinal analgesic (anti-hyperalgesic) effects. These effects were statistically significant for orphenadrine (p < 0.0001) and for the combination of orphenadrine and diclofenac (p < 0.0013). The single ingredient diclofenac reduced the P2-component by a value just below clinical relevance (p < 0.0848).
Conclusion: This study demonstrated the efficacy of Neodolpasse® in a human pain model. The observed effect was mainly caused by central mechanisms and was found to be superior for the fixed-dose combination of orphenadrine and diclofenac compared with the individual ingredients. Both components contributed to the effect of the combination in an additive fashion, which can be explained by the different molecular mechanisms of action of each drug.








Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Menasse R, Hedwall PR, Kraetz J, et al. Pharmacological properties of diclofenac sodium and its metabolites. Scand J Rheumatol Suppl 1978; 22: 5–16
Ku EC, Lee W, Kothari HV, et al. Effect of diclofenac sodium on the arachidonic acid cascade. Am J Med 1986; 80: 18–23
Todd PA, Sorkin EM. Diclofenac sodium: a reappraisal of its pharmacodynamic and pharmacokinetic properties, and theraperpeutic cacy. Drugs 1988; 35: 244–85
Jurna I, Brune K. Central effect of the non-steroid anti-inflammatory agents, indomethacin, ibuprofen, and diclofenac, determined in C fibre-evoked activity in single neurones of the rat thalamus. Pain 1990; 41: 71–80
Bijlsma UG, Harms AF, Funcke ABH, et al. The pharmacology of gB-dimethylaminoethyl-2-methylbenzhydrylether hydrochloride. Arch Int Pharmacodyn Ther 1956; 1: 332–68
Ginzel KH. The blockade of reticular and spinal facilitation of motor function by orphenadrine. J Pharmacol Exp Ther 1966; 154: 128–41
Onuaguluchi G, Lewis JJ. Some aspects of the pharmacology of orphenadrine. J Pharm Pharmacol 1963; 15: 329–36
Smith CM. Relaxation of decerebrate rigidity by orphenadrine. Proc Soc Exp Biol Med 1964; 116: 75–6
Steinbrecher W. Myotonolyse durch Orphenadrincitrat. Arzneimittel Forschung 1966; 16: 147–53
Hunskaar S, Donell D. Clinical and pharmacological review of the efficacy of orphenadrine and its combination with paracetamol in painful conditions. J Int Med Res 1991; 19: 71–87
Schaffler K, Reitmeir P. Analgesic effects of low-dose intravenous orphenadrine in the state of capsaicin hyperalgesia: a randomized, placebo-controlled, double-blind cross-over study: using laser somatosensory evoked potentials obtained from capsaicin-irritated skin in healthy volunteer. Arzneimittel Forschung 2004; 54: 673–9
Winter L, Post A. Analgesic combinations with orphenadrine in oral post surgical pain. J Int Med Res 1979; 7: 240–6
Raffa RB. Antihistamines as analgesics. J Clin Pharm Ther 2001; 26: 81–5
Olsen UB, Eltorp CT, Ingvardsen BK, et al. ReN 1869, a novel tricyclic antihistamine, is active against neurogenic pain and inflammation. Eur J Pharmacol 2002; 435: 43–57
Jones B, Kenward MG. Design and analysis of cross-over trials. London: Chapman and Hall, 1989
Schaffler K, Wauschkuhn CH, Gierend M. Analgesic potency of a new anticonvulsant drug versus acetylsalicylic acid via laser somatosensory evoked potentials: randomised placebo-controlled double blind (5-way) crossover study. Arzneimittel Forschung 1991; 41: 427–35
Schaffler K, Seibel K, Thomsen M, et al. Effect of the new H1-antagonist ReN1869 on capsaicin-induced hyperalgesia in human skin/Human phase-I trial using somatosensory evoked potentials induced by a CO2 laser. Arzneimittel Forschung 2004; 54: 187–91
Schaffler K, Wauschkuhn CH, Brunnauer H, et al. Evaluation of the local anaesthetic activity of dimethindene maleate by means of laser algesimetry in healthy volunteers. Arzneimittel Forschung 1992; 42: 1332–5
Schaffler K, Medert G. The analgesic, anti-inflammatory profile of dexketoprofen trometamol (vs tramadol). Schmerz 1998; 12 (S1): 69–70
Bromm B, Jahnke MT, Treede RD. Responses of human cutaneous afferents to CO2 laser stimuli causing pain. Exp Brain Res 1984; 55: 158–66
Putt M, Chinchilli VM. A mixed effects model for the analysis of repeated measures cross-over studies. Stat Med 1999; 18: 3037–58
Zecca L, Ferrario P, Costi P. Determination of diclofenac and its metabolites in plasma and cerebrospinal fluid by high-performance liquid chromatography with electrochemical detection. J Chromatogr 1991; 567: 425–32
Valtonen EJ. A controlled clinical trial of chlormezanone, orphenadrine, orphenadrine/paracetamol and placebo in the treatment of painful skeletal muscle spasms. Ann Clin Res 1975; 7: 85–8
Hough LB, Nalwalk JW, Svokos K, et al. Pain-relieving drugs and the brain histaminergic system: multiple analgesic mechanisms from histamine, improgan and cimetidine. Inflamm Res 2004; 53 Suppl. 1: S43–4
Kashiba H, Fukui H, Senba E. Histamine H1 receptor mRNA is expressed in capsaicin-insensitive sensory neurons with neuropeptide Y-immunoreactivity in guinea pigs. Brain Res 2001; 901: 85–93
Diamond BI, Bluhm RE, Borison RL, et al. Brain histamine: an endogenous system for mediating pain [abstract]? Anaesthesiology 1981; 55: A286
Eguiagaray JG, Egea J, Bravo-Cordero JJ, et al. Neurotransmisores, senales de calcio y comunication neuronal [Neurotransmitters, calcium signalling and neuronal communication]. Neurocirugia 2004; 15: 109–18
Vane JR, Bahlke YS, Botting RM. Cyclooxygenases 1 and 2. Annu Rev Pharmacol Toxicol 1998; 38: 97–120
Pinardi G, Sierralta F, Miranda HF. Adrenergic mechanisms in antinociceptive effects of non steroidal anti-inflammatory drugs in acute thermal nociception in mice. Inflamm Res 2002; 51: 219–22
Pinardi G, Sierralta F, Miranda HF. Atropine reverses the antinociception of nonsteroidal anti-inflammatory drugs in the tail-flick test of mice. Pharmacol Biochem Behav 2003; 74: 603–8
Kornhuber J, Parsons CG, Hartmann S, et al. Orphenadrine is an uncompetitive n-methyl-d-aspartate (NMDA) receptor antagonist: binding and patch clamp studies. J Neural Transm Gen Sect 1995; 102: 237–42
Rumore MM, Schlichting DA. Analgesic effects of antihistamines. Life Sci 1985; 36: 403–16
Pubill D, Canudas AM, Pallas M, et al. Assessment of the adrenergic effects of orphenadrine in rat vas deferens. J Pharm Pharmacol 1999; 51: 307–12
Seibel K, Schaffler K, Reeh P, et al. Comparison of two different preparations of ibuprofen with regard to the time course of their analgesic effect: using laser somatosensory evoked potentials from UV-irritated skin in healthy volunteers. Drug Res 2004; 54: 444–51
Acknowledgements
The authors wish to thank Gerd Hoerl, PhD and Peter Schaffer, PhD for their valuable contributions in planning this clinical study, and Fresenius Kabi Austria GmbH for financial support for the study. The authors had no other financial support other than that provided by the study sponsor. They have no potential conflicts of interest that are relevant to the contents of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schaffler, K., Reitmeir, P., Gschanes, A. et al. Comparison of the Analgesic Effects of a Fixed-Dose Combination of Orphenadrine and Diclofenac (Neodolpasse®) with its Single Active Ingredients Diclofenac and Orphenadrine. Drugs R D 6, 189–199 (2005). https://doi.org/10.2165/00126839-200506040-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00126839-200506040-00001