Growth perturbations from stimulant medications and inhaled corticosteroids
Introduction
Monitoring physical growth in children and adolescents is an integral part of pediatric practice. Deviation from normal growth patterns, in the form of growth attenuation or acceleration, can be the initial manifestation of a variety of systemic illnesses and endocrine disorders (1). Growth deceleration during childhood and adolescence remains an important reason for referral to pediatric endocrinologists. The differential diagnosis of growth failure in children is extensive, and includes genetic factors, malnutrition, chronic systemic illnesses and endocrine disorders. In addition, many medications prescribed for non-endocrine conditions have the potential to lead to growth attenuation. This review focuses on the growth effects of two classes of medications that are commonly prescribed in pediatrics—stimulant medications for the treatment of attention deficit hyperactivity disorder (ADHD); and inhaled glucocorticoids for the treatment of asthma.
Stimulant medications
The effects of stimulant medications such as methylphenidate and dexamphetamine for ADHD on growth have been debated for many years. Several review papers including Poulton (2) and Faraone et al. (3) have summarized the literature on this topic and concluded there are growth deficits, but admitted to knowledge gaps warranting additional studies. Since stimulant therapy is the standard of care for ADHD management, randomized controlled trials (RCT) with placebo arms are not feasible. Therefore, the majority of studies are prospective observational studies or retrospective reviews. We discuss findings from more recent studies in this section. Observations from key studies are summarized in Table 1.
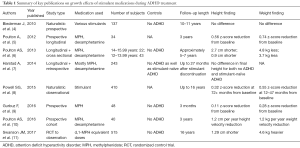
Full table
Suppression of appetite in children while on stimulant medications is well recognized by parents; consequent declines in the weight gain and height growth of children is well known to general pediatricians. The magnitude of the height deficit has been a focus of many studies. Several groups have reported height deficits of 1 to 1.4 cm per year during the first 2 years of stimulant treatment (12-14). This may be followed by a period of catch-up growth (12). The decreased height velocity is seen in children as young as the preschool aged population (14).
Multiple studies have evaluated the change in height trajectories associated with stimulant medication, using z-score comparisons. In their observational study where subjects received stimulant medication for a mean of 6 years (up to 16 years), Powell et al. found the decrease in height z-scores was significant from baseline, with a total absolute reduction of 0.32 (7). They report attenuation in the decrease in growth after 12–47 months of treatment, but baseline values were not reached even after 72 months; effects were dose-related, and there was no relation to comorbid conditions (8). Harstad et al. studied a cohort until adulthood (7), and reported that subjects on stimulant treatment for at least 3 years (n=171, mean treatment duration 53 months) had a decrease in mean height z-score from 0.48 at the beginning to 0.33 at the end of treatment. They concluded that there was no clinically significant height deficit at adulthood (7).
Many studies have investigated clinical correlates of growth outcomes in children on stimulant medications. Decreased height velocity and lower height z-scores have been associated with higher doses of stimulant medication (10,15,16). Greater changes in height z-scores from baseline were found in younger subjects (10,16,17). Faraone et al. found that the biggest reduction in expected height was in the tallest children (16). Spencer et al. reported that drug holidays of at least 30 days did not significantly affect growth (17), and concluded that drug holidays are of questionable utility in limiting the adverse effects of stimulants on growth.
One question that has vexed investigators is whether the changes in growth are intrinsically related to ADHD itself, or are exclusively due to stimulant medication. The Multimodal Treatment Study of ADHD (MTA), a naturalistic study published in 2004, compared 521 subjects with ADHD treated with medication to those treated by other means such as behavioral modification (13). Those taking stimulant medication were found to be 3.7 cm shorter than those never take stimulant medication after 14 months of treatment; those taking medication were also noted to be 1.69 cm shorter at baseline (13). Evaluation of data from the National Epidemiologic Survey on Alcohol and Related Conditions 2004–2005 compared adult heights of subjects with ADHD receiving stimulant therapy to subjects with ADHD not taking stimulants to controls without ADHD: 68.29, 67.9 and 66.93 inches respectively; there was no significant difference between the groups after adjustments (18). Separate studies have also concluded that neither ADHD itself, nor stimulant therapy significantly affected adult height (4,7).
Young adult outcomes in the follow-up of the MTA were recently published (11). The MTA began as a randomized clinical trial of 579 children between 7–10 years of age with ADHD combined type that lasted for 14 months (13); most subjects were on immediate-release methylphenidate. After that trial, the majority of participants (n=515) were followed as an observational study until an average age of 25 years (11); 289 classmates (258 without ADHD) were added as a comparison group. The primary objective of the study was to assess adult symptom severity. Adult height was a secondary outcome. Methylphenidate dose equivalent to 10 mg per day at least 50% of the days was considered the minimum treatment. Subjects were classified into three groups, based on medication compliance with the minimum treatment at the various assessed intervals: ‘consistent’, ‘inconsistent’, and ‘negligible’. Overall, participants with ADHD were 1.29±0.55 cm shorter than the comparison group (11). Although this was statistically significant, the authors concluded that this may not be clinically significant. When analyzed based on medication compliance, those in the ‘consistent’ or ‘inconsistent’ categories were 2.55±0.73 cm shorter than those in the ‘negligent’ group. Those in the ‘consistent’ group were 2.36±1.13 cm shorter than those in the ‘inconsistent’ group. The adult height difference was 4.7 cm when comparing those in the ‘consistent’ medication group to those in the ‘negligent’ medication group. The mean height z-score was −0.2685 for males in the ‘consistent’ group and −0.2152 for females in the ‘consistent’ group. Interestingly, subjects in the ADHD group were 4.6±1.78 kg heavier than the comparison group. Regression analysis suggested a decrease in adult height with an increase in cumulative stimulant dose. Despite noting suppressed final adult height in those with extended use of medication, symptom severity was not improved (11). The authors contrasted the findings of the significant growth suppression in this study with those of previous studies that did not show growth suppression (4,7,18). They related their findings to changes in the clinical use of medication over the past 50 years, with consistent increases in the cumulative stimulant (methylphenidate equivalent, ME) doses from the 1960s to the 1990s (11).
Poor weight gain during treatment with stimulant medications is well recognized. Poulton et al. found that weight was more affected than height, with the change in weight z-score being 2.4 times higher than the change in height z-score after 30 months of stimulation medication (12). Powell et al. reported that subjects who lost weight in the first year of treatment had the largest relative weight loss (8). Weight gain may be more sensitive to growth effects with stimulant use, so changes in weight gain may happen at lower stimulant doses than changes in height velocity (15). Faraone et al. reported significant correlation between height and weight loss (r =0.40), but, they only shared 16% of variance (16). Thus, the authors suggested improved nutrition will likely only minimally decrease the expected height deficit (16).
Factors such as puberty and bone age are also important considerations when evaluating effects of stimulant medications on growth. Consistent with the notion of delayed growth with chronic illnesses and stimulant medication use, the age of peak height velocity for males treated with stimulants was significantly later than for those with ADHD but no stimulant therapy (7). A study of 65 adolescent boys aged 12–16 years at recruitment and followed for a mean of 6.3 years concluded that stimulant medication does not delay the onset of puberty, but slows the rate of pubertal progression and delays the timing of peak growth velocity (6). Bone age was not delayed for those with ADHD on stimulant medications (10).
It has also been proposed that the appetite changes associated with stimulant medications may play a role in altering growth patterns. Gurbuz et al. evaluated hormones associated with appetite regulation (9). They reported that after treatment with methylphenidate, levels of leptin (an appetite-suppressing hormone) increased, and levels of ghrelin (an appetite-stimulating hormone) decreased significantly. Levels of insulin-like growth factor 1 (IGF-1), a marker of growth hormone (GH) action and nutritional status, decreased significantly after 3 months of stimulant treatment; but levels of insulin-like growth factor binding protein-3 (IGFBP-3), a more selective marker of GH action, did not change. For the 71% of males treated with methylphenidate who had a decreased appetite, weight z-scores and BMI z-scores were reduced significantly. The authors suggested that a decreased appetite leads to reductions in body weight and BMI and ultimately, decreased height z-scores (9).
Poulton et al. investigated alterations of body composition during treatment with stimulant medication for 3 years in 34 prepubertal children with ADHD, compared with 241 healthy controls (5). Subjects on stimulant medication experienced early fat loss during the first 6 months. Bone densitometry and serum markers of bone turnover showed that lean tissue and bone mineral density increased more slowly during the 3 years of treatment, than would be expected for growth in height (5). More definitive long-term studies are necessary to assess whether these adverse effects on body composition persist into adulthood.
There has been increasing interest in studying the effects of stimulant medications on growth among children who are on combined treatment with stimulants for ADHD and GH therapy for a multitude of reasons, including growth hormone deficiency (GHD) and idiopathic short stature (ISS). The availability of post-marketing surveillance databases maintained by many manufacturers of GH facilitates such investigations. Frindik et al. retrospectively evaluated prepubertal children with ISS or GHD taking GH ± medication for ADHD using data from the Genentech’s National Cooperative Growth Study database (19). After adjusting for various factors, those receiving both GH and ADHD medication had a lower growth rate after a year of GH, compared to those only on GH: 8.5±2 and 9.4±2.6 cm/year, respectively; the difference was not clinically significant (19). Rose et al. reported on growth outcomes in children on GH therapy enrolled in the American Norditropin Studies: Web-Enabled Research (ANSWER) Program (20). They compared children only on GH therapy, to children on GH therapy and stimulant medication for ADHD, for the first four years of GH therapy. After adjusting for baseline age, height, weight, BMI, and sex, the change in BMI z-score was greater for the patients taking ADHD stimulant medication, implying that GH treatment may reduce the appetite suppression seen with stimulant medication. However, after matching for baseline measurements, ADHD stimulant medication did not have an effect on the linear growth response of children treated with GH (20).
Miller et al. evaluated growth in children enrolled in the KIGS (Pfizer International Growth Study) database receiving GH therapy (21). They concluded that ADHD may affect the ability of a child with ISS and ADHD to respond well to GH therapy, but even children with ADHD had improved growth on GH therapy. Children with idiopathic GHD on stimulant medication grew 1.1 cm less than children without ADHD in the first year of GH treatment. Among children with ISS, those treated with stimulants were 0.74 cm shorter, and those with ADHD not treated with stimulants were 0.69 cm shorter (21).
Renes et al. investigated a cohort of children born small for gestational age (SGA) receiving GH therapy, with or without stimulant therapy for ADHD (22). The authors compared 39 children treated with GH for SGA and methylphenidate for ADHD to 39 matched children treated with GH for SGA, without ADHD. Those on stimulant therapy received methylphenidate for at least 6 months (mean duration 3.7±2.5 years). There was a significant decrease in height growth velocity between 6 and 12 months among subjects treated with a stimulant. After 3 years, subjects receiving stimulant medication had a 0.2 z-score reduced height gain compared to children not taking stimulant therapy. However, both groups had similar adult heights at −1.9 standard deviation score (22).
Inhaled corticosteroids (ICS)
Endogenous glucocorticoids derived from the adrenal gland are essential for growth. In fact, the presence of glucocorticoids at physiologic levels is necessary for the differentiation and maturation of somatotropes, the cells in the pituitary responsible for releasing GH (23). Physiologic glucocorticoids also directly increase GH release through various mechanisms involving growth hormone releasing hormone (GHRH), GH secretagogue receptors, GH, IGF-1 and insulin-like growth factor binding protein-1 (IGF-BP1) (23). At the same time, sustained or supra-physiologic glucocorticoid exposure blunts these positive effects by inhibiting GH release and disrupting the pulsatility of GH secretion, thereby limiting its biologic action (24). Supra-physiologic and sustained glucocorticoids further limit growth through peripheral actions including inhibition of chondrocyte mitosis, collagen synthesis and GH receptor at the epiphyseal growth place, decreased IGF-1 synthesis and activity and decreased mineral retention (25). Thus, the overall impact of glucocorticoids on growth is dependent on both the concentration of glucocorticoids and duration of exposure.
ICSs are the first line therapy for persistent asthma (26), a common childhood illness affecting up to 8.4% of all children in the United States (27,28). In addition to their intended effect of reducing airway inflammation, ICS can exert unintended effects, including growth suppression, via binding at glucocorticoid receptors when absorbed systemically, either directly via lung deposition or through gastrointestinal absorption from swallowed portion. The frequency and severity of growth suppression (and other potential adverse effects) varies significantly based on the systemic bioavailability and binding affinity of the specific ICS and formulation, administration technique and patient characteristics. In general, ICS are considered very potent with an approximate 10–20 times higher binding affinity for glucocorticoid receptor compared to dexamethasone (29,30). As a result, even small changes in systemic absorption could significantly increase the risk for growth suppression and other potential adverse effects.
Several large prospective RCTs have helped clarify the short-term effects of ICS on growth in prepubertal children. Results from these studies have consistently demonstrated a small, but significant decrease in growth velocity and height during the first year of therapy with beclomethasone CFC 400 mcg/day. For example, in a multi-center international study examining growth rates in prepubertal children naïve to ICS (31), growth velocity of children receiving beclomethasone CFC 200 mcg twice daily was 0.78 cm/year slower than children receiving placebo over a 56-week period (95% CI, −1.06 to −0.46; growth velocity 4.86 vs. 5.64 cm/year). Meta-analysis by Sharek et al. (32) of four additional studies using beclomethasone CFC 400 mcg/day demonstrated similar findings with a decreased growth velocity in treatment group of −1.51 cm/year compared to controls (n=450).
Prospective RCTs evaluating short term effects of other ICS formulations demonstrate variable effects. For budesonide, the majority of studies demonstrate similar findings to beclomethasone, with mild growth suppression most pronounced during the first year of therapy. Two major studies highlighting this finding include the Childhood Asthma Management Program (CAMP), and a large multicenter international study conducted by Pauwels et al. In the CAMP study (33), children ages 5–12 years were randomized to either budesonide 200 mcg twice daily (n=311) or placebo (n=208) and followed for mean duration of 4.3 years. At the end of treatment, mean height increase among children in the treatment group was 1.1 cm less compared to those in the placebo group. This difference was primarily accounted for by decreased growth velocity during year 1 of treatment with no difference in growth velocity between groups at the end of treatment (33). Similarly, Pauwels et al. (34) found a mean difference in growth velocity of −0.43 cm/year (95% CI, −0.54 to −0.32) when evaluating effects of budesonide in children ages 5–15 years over a 3-year period (children >12 years received budesonide 400 mcg/day and <12 years received <200 mcg/day). In children less than 11 years, this effect was noted to be more pronounced during year 1 compared to years 2 and 3 (growth reduction 0.58 in year 1, 0.43 in year 2 and 0.33 in year 3) (34).
In contrast, studies evaluating the effect of fluticasone and ciclesonide on linear growth did not consistently exhibit growth suppression. A study by Allen et al. (35) found no difference in growth velocity over a 1-year period in prepubertal children randomized to receive either fluticasone 50 mcg twice daily (n=85), fluticasone 100 mcg twice daily (n=96) or placebo (n=87) with growth velocities of 5.91±0.16, 5.67±0.13 and 6.1±0.17 cm/year respectively (P=0.313). Likewise, Sorkness et al. (36) reported no difference in growth velocity for children (n=285, ages 6–14 years) randomized to receive either fluticasone 100 mcg twice daily (n=96), fluticasone 100 mcg daily combined with salmeterol 50 mcg twice daily (n=94) or montelukast 5 mg daily (n=95) over a 48-week period (−0.4 cm/year with 95% CI, −0.93 to 0.13; −0.46 cm/year with 95% CI, −0.99 to 0.07 and 0.06 cm/year with 95% CI, −0.47 to 0.59). Evaluation of growth effects from ciclesonide therapy in a study by Skoner et al. (37) comparing prepubertal children (n=661) randomized to receive either ciclesonide 40 mcg daily (n=221), 160 mcg daily (n=219) or placebo (n=221) also did not demonstrate any difference in growth velocity over a 1-year period with growth velocities of 6.2, 6.59 and 6.49 cm/year respectively. Interestingly, while the majority of RCT evaluating the impact of fluticasone on growth do not demonstrate growth suppression individually, meta-analysis by Zhang et al. (38) found a small effect when analyzed collectively with mean difference in growth velocity at 1 year following fluticasone 100–200 mcg/day of −0.39 cm/year (95% CI, −0.63 to −0.15). This was not the case for ciclesonide (38).
Studies evaluating dose-effect relationship between ICS and growth outcomes have shown a small, but statistically significant effect when comparing high versus low ICS doses. Meta-analysis by Pruteanu et al. (39) demonstrated an increased growth velocity over 12 months of 0.2 cm/year (95% CI, 0.02–0.39) in children receiving low dose ICSs (n=339) compared to those receive high dose corticosteroids (n=389). However, there was no effect on height z-scores at 1 year (+0.08, 95% CI, −0.03 to 0.2) (39). Of note, the majority of these studies evaluated newer formulations and/or delivered ICS as hydrofluoroalkane (HFA) propellant as compared to previous studies which primarily evaluated older formulations and ICSs administered via chlorofluorocarbon (CFC) propellant (35,37,40).
In summary, short-term treatment with ICS is associated with a small, but statistically significant decrease in linear growth velocity in most cases. Meta-analysis performed on RCTs (38) found the magnitude of this effect to be −0.48 cm/year (95% CI, −0.65 to −0.3 cm/year) during 1 year of treatment reflecting a change in height z-score of −0.13 (95% CI, −0.24 to −0.01). There is also a small, but statistically significant dose-effect relationship.
While it is generally accepted that ICS result in temporary growth suppression, controversy persists over long-term effects and impact on final adult height. In the only randomized controlled double-blind study assessing final adult heights to date, Kelly et al. (41) found that compared to children who did not receive ICS for asthma management (n=208), mean adult heights in children who received ICS for asthma management (budesonide 200 mcg twice daily, n=311) was 1.2 cm lower (95% CI, −1.9 to −0.5, P=0.001). This was roughly equivalent to the difference seen at the end of treatment period suggesting that the initial growth suppression seen during the first 2 years of therapy was sustained, but not further augmented by continued therapy. Other studies have found no difference on ICS therapy for management of asthma and final adult height. In a prospective, non-randomized control study by Agertoft et al. (42), measured final adult height compared to target height did not differ between children who received ICSs for asthma management (n=270 at enrollment, adult height data available for 142) compared to controls with asthma who did not receive ICSs (n=62, adult height data available for 18) or their healthy siblings (n=51). Adult height minus target height was 0.3 cm (95% CI, −0.6 to 1.2), −0.2 cm (95% CI, −2.4 to 2.1) and 0.9 cm (95% CI, −0.4 to 2.2) for each group respectively. No differences were seen when evaluating by dose adjusted for weight, cumulative dose or duration of therapy (42). The study did note mild growth suppression during the first few years of therapy, with growth velocity during pre-treatment period of 6.1 cm/year compared to growth velocity of 5.1 cm/year (95% CI, 4.7 to 5.5) during year 1 and 5.5 cm/year (95% CI, 5.1 to 5.0) during year 2 similar to other studies; however this effect was not sustained over time (42). Similarly, a retrospective review of final adult height in adults with asthma by Van Bever et al. (43) did not find any difference in final height or height SDS between adults who received ICS during childhood (n=42) compared to those who did not (n=43; height SDS 0.66±1.1 vs. 0.89±1.0, P=0.31). Due to the retrospective nature of this study, asthma severity and duration and dosing of ICS therapy were not controlled.
Additional research is needed to assess the effects of newer ICS formulations and administration route on growth outcomes. Newer ICS formulations such as mometasone, fluticasone propionate and ciclesonide have increased binding affinity at the glucocorticoid receptor compared to beclomethasone and budesonide. As a result, equivalent systemic doses of newer formulations may exert more potent growth suppression as compared to older formulations (44). The administration route has a significant impact of the systemic availability of ICSs. For example, the mass median aerodynamic diameters (MMADs) of newer HFA propelled meter dose inhalers (MDIs) is smaller than the MMAD of CFC MDIs which increases drug delivery to the small airways when given at the same doses (45). While this is beneficial from a therapeutic standpoint, it also increases systemic bioavailability and therefore the risk for systemic effects such as growth suppression (29). In general, dry powder inhalers contain larger MMADs and therefore have decreased delivery to small airways and systemic absorption when compared to their HFA-MDI counterparts, although this difference can vary significantly between formulations (29,45). Additional factors that contribute to systemic bioavailability include administration technique and spacer use.
Individual factors such as age, pubertal status, adherence and concomitant use of other growth suppressing medications can also influence growth effects of ICS. The majority of knowledge regarding growth effects of ICS is derived from evaluation in prepubertal subjects. Historically, periods of rapid growth such as during toddlerhood and puberty were thought to be protected from growth suppressive effects of ICS, based on available evidence. In an early study by Storr et al. (46), no difference in height gain was demonstrated over an 18 month period (4.23 vs. 4.42 cm; P not significant) in children randomized to receive either beclomethasone 300 mcg/day (n=15) or placebo (n=14). A more recent and larger study by Wasserman et al. (47) of children ages 24 to 47 months identified no difference in growth velocity when comparing treatment groups (fluticasone 50 mcg/day, n=114; 100 mcg/day, n=108) versus placebo over a 12-week period. Lack of effect on growth velocity in toddlers/preschoolers was also demonstrated by Bisgaard et al. (48) in a study evaluating growth rates in children ages 12–47 months over a 52-week period. In this study no difference in growth rate (−2.4 mm/year; 95% CI, −6.6 to 1.8) was seen in children randomized to receive either fluticasone propionate 100 mcg daily with babyhaler (n=471) or sodium cromolyn glycate 5 mg four times daily (n=154) (48). In contrast, Guilbert et al. (49) demonstrated slow growth velocity in children receiving fluticasone 176 mcg/day via aerochamber valve chamber with mask compared to controls during 1 year of treatment (mean age 3±0.6 years; growth velocity 6.6 vs. 7.3 cm/year, P=0.005). Despite no difference in growth velocity during year 2 of therapy and a period of increased growth velocity during year 3 of the study (after discontinuation of fluticasone), at the end of the 3-year study height gain in children in treatment group was 0.7 cm less than those receiving placebo (P=0.008) (49). This effect was more pronounced in children younger than 3 years of age with lower weight (>10 mcg/kg/day) suggesting that age and weight based dose-effect may modify growth response to ICSs (49).
Data on effects of ICSs on growth during puberty is limited. In a recent retrospective study by De Leonibus et al. (50), adolescents receiving ICSs for asthma management (n=113) demonstrated reduced peak growth velocity (boys −6.54 vs. 8.18 cm/year, P=0.006; girls 5.36 vs. 7.1 cm/year, P=0.015), reduced pubertal height gain-SDS (−0.21 vs. 0.03 boys, P=0.036; −0.35 vs. 0.02 girls, P=0.012) and reduced overall final adult height (−2.5 cm ± 2.89 boys; P=0.028 and 2.0 cm ± 2.03 girls; P=0.047) compared to adolescents without asthma (50). While this study was limited by its retrospective nature and use of controls without asthma, the findings suggest possible growth inhibition during puberty with lack of “catch-up” growth at final adult height which has not been previously demonstrated. Additional information from prospective, randomized controlled studies is needed to elucidate the presence and magnitude of this effect.
In addition to age and puberty, other factors that can influence individual variation include adherence rates and administration timing. Children with high adherence to prescribed treatment regimen are more likely to exhibit growth suppression (45). Likewise, children who receive twice daily dosing, particularly if dosing is administered in the late evening, are theorized to have increased growth suppression due to disruption of physiologic diurnal cortisol pattern which is essential for pulsatile GH release (45). Finally, children who are on other potentially growth suppressing medications, such as stimulants or selective serotonin reuptake inhibitors, in addition to ICSs may have an increased risk for growth suppression due to additive or synergistic effects from these medications which are proposed to exert their influences via different mechanisms (27).
Discussion
Stimulant medications form the mainstay of treatment of ADHD, and their use significantly improves daily function of affected children and adolescents in various settings, both at home and at school. Adverse effects include appetite suppression, sleep difficulties, poor weight gain (or weight loss), and behavioral problems. Attenuation of growth while on treatment with stimulant medications for ADHD has long been a focus of investigation, and is generally thought to be a consequence of appetite suppression. Growth deficits of 1–1.4 cm per year, mainly in the first 2 years of treatment has been observed (12,14), with later catch-up (12). Growth attenuation has been observed in children as young as in preschool (14), and the tallest children may have the greatest height deficits (16). Dose dependency of growth effects has also been reported (10,15,16).
Studies in which subjects have been followed into adulthood have reported divergent findings. Harstad et al. reported that among subjects who received stimulant treatment for a minimum of 3 years, there was no clinically significant height deficit at adulthood (7). Studies by Peyre et al. (18) and Biederman et al. (4) reached similar conclusions. Results of the Multimodal Treatment Study of ADHD (MTA) offer additional insight. The initial 14-month RCT phase of stimulant medication treatment showed a clinically significant height deficit (13). However, when subjects were then observed until adulthood, height differences were much smaller in magnitude, with group differences noted based on degree of compliance with medication (11). Taken together, the results of the multiple studies imply that subjects who have experienced the highest cumulative stimulant medication exposure are at increased risk for growth attenuation, and warrant close monitoring through adulthood.
The reported decrease in bone mineral accrual among prepubertal children treated with stimulants is of concern (5). It remains to be seen whether pubertal maturation will mitigate this effect, although long-term studies are lacking in this regard.
ICSs are an integral part of the management of persistent asthma. The overall safety profile of ICS is advantageous with their numerous benefits, including reduced frequency of asthma exacerbations and improved pulmonary function, outweighing the risk of mild growth suppression. In fact, the use of ICS may reduce the overall systemic glucocorticoid burden by decreasing the need prolonged courses of oral glucocorticoids, which have a worse adverse effect profile. In the short term, ICS have a small but statistically significant effect on growth, with reductions in growth rates between 0.4 and 1.5 cm/year. These effects are primarily seen in the first year of treatment and are generally transient (31-34). There is, however, significant variation in this effect related to systemic bioavailability which varies by pharmacologic agent, dose exposure and mode of delivery. Based on current available evidence, ICS therapy for asthma management is associated with a limited impact on adult height of approximately −1.2 cm (41). Factors affecting individual variation in the growth suppressing effect of ICS include age, pubertal status, adherence to therapy, timing of administration, and concomitant use of other medications that suppress growth.
The most serious potential adverse effect associated with ICS therapy is adrenal insufficiency (51), and requires constant vigilance. Children with growth suppression or other systemic effects from ICS should be screened for adrenal insufficiency by obtaining AM cortisol and plasma adrenocorticotrophic hormone (ACTH). In the presence of other risk factors, hyperglycemia and adverse effect on bone mineral density are additional considerations (51).
Since the growth attenuation attributable to treatment with stimulant medications and ICS will be mild and transient in most children, caution must be exercised with children who have clinically significant growth deceleration. Additional etiologies should be sought under those circumstances.
Conclusions and key points
- The therapeutic benefits of ICS for management of asthma and stimulant medications for management of ADHD outweigh the potential risk for growth suppression, based on current knowledge. ICS reduce exacerbations and hospitalizations from asthma, improve pulmonary function, improve quality of life and reduce asthma related death;
- To minimize risk for growth suppression and other potential adverse effects, prescribers should use the lowest dose necessary to achieve optimal disease management, and frequently reassess whether dose titration is possible;
- When growth suppression is present, children should be evaluated for other potential adverse effects including adrenal insufficiency, in the case of ICSs;
- Future studies are needed to ascertain more information about the long-term effects of growth suppressing medications on final adult height (newer formulations for ICS and more RCT prospective studies for stimulants).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Backeljauw PF, Dattani MT, Cohen P, et al. Disorders of growth hormone/insulin-like growth factor secretion and action. In: Sperling MA. editior. Pediatric Endocrinology, 4th edition. Philadelphia, PA: Elsevier Saunders, 2014:292-404.
- Poulton A. Growth on stimulant medication; clarifying the confusion: a review. Arch Dis Child 2005;90:801-6. [Crossref] [PubMed]
- Faraone SV, Biederman J, Morley CP, et al. Effect of stimulants on height and weight: a review of the literature. J Am Acad Child Adolesc Psychiatry 2008;47:994-1009. [PubMed]
- Biederman J, Spencer TJ, Monuteaux MC, et al. A naturalistic 10-year prospective study of height and weight in children with attention-deficit hyperactivity disorder grown up: sex and treatment effects. J Pediatr 2010;157:635-40, 640.e1.
- Poulton A, Briody J, McCorquodale T, et al. Weight loss on stimulant medication: how does it affect body composition and bone metabolism? - A prospective longitudinal study. Int J Pediatr Endocrinol 2012;2012:30. [Crossref] [PubMed]
- Poulton AS, Melzer E, Tait PR, et al. Growth and pubertal development of adolescent boys on stimulant medication for attention deficit hyperactivity disorder. Med J Aust 2013;198:29-32. [Crossref] [PubMed]
- Harstad EB, Weaver AL, Katusic SK, et al. ADHD, stimulant treatment, and growth: a longitudinal study. Pediatrics 2014;134:e935-44. [Crossref] [PubMed]
- Powell SG, Frydenberg M, Thomsen PH. The effects of long-term medication on growth in children and adolescents with ADHD: an observational study of a large cohort of real-life patients. Child Adolesc Psychiatry Ment Health 2015;9:50. [Crossref] [PubMed]
- Gurbuz F, Gurbuz BB, Celik GG, et al. Effects of methylphenidate on appetite and growth in children diagnosed with attention deficit and hyperactivity disorder. J Pediatr Endocrinol Metab 2016;29:85-92. [Crossref] [PubMed]
- Poulton AS, Bui Q, Melzer E, et al. Stimulant medication effects on growth and bone age in children with attention-deficit/hyperactivity disorder: a prospective cohort study. Int Clin Psychopharmacol 2016;31:93-9. [Crossref] [PubMed]
- Swanson JM, Arnold LE, Molina BS, et al. Young adult outcomes in the follow-up of the multimodal treatment study of attention-deficit/hyperactivity disorder: symptom persistence, source discrepancy, and height suppression. J Child Psychol Psychiatry 2017;58:663-78. [Crossref] [PubMed]
- Poulton A, Cowell CT. Slowing of growth in height and weight on stimulants: a characteristic pattern. J Paediatr Child Health 2003;39:180-5. [Crossref] [PubMed]
- MTA Cooperative Group. National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: changes in effectiveness and growth after the end of treatment. Pediatrics 2004;113:762-9. [Crossref] [PubMed]
- Swanson J, Greenhill L, Wigal T, et al. Stimulant-related reductions of growth rates in the PATS. J Am Acad Child Adolesc Psychiatry 2006;45:1304-13. [Crossref] [PubMed]
- Charach A, Figueroa M, Chen S, et al. Stimulant treatment over 5 years: effects on growth. J Am Acad Child Adolesc Psychiatry 2006;45:415-21. [Crossref] [PubMed]
- Faraone SV, Biederman J, Monuteaux M, et al. Long-term effects of extended-release mixed amphetamine salts treatment of attention- deficit/hyperactivity disorder on growth. J Child Adolesc Psychopharmacol 2005;15:191-202. [Crossref] [PubMed]
- Spencer TJ, Faraone SV, Biederman J, et al. Does prolonged therapy with a long-acting stimulant suppress growth in children with ADHD? J Am Acad Child Adolesc Psychiatry 2006;45:527-37. [Crossref] [PubMed]
- Peyre H, Hoertel N, Cortese S, et al. Long-term effects of ADHD medication on adult height: results from the NESARC. J Clin Psychiatry 2013;74:1123-4. [Crossref] [PubMed]
- Frindik JP, Morales A, Fowlkes J, et al. Stimulant medication use and response to growth hormone therapy: an NCGS database analysis. Horm Res 2009;72:160-6. [Crossref] [PubMed]
- Rose SR, Reeves G, Gut R, et al. Attention-Deficit/Hyperactivity Disorder Medication Treatment Impact on Response to Growth Hormone Therapy: Results from the ANSWER Program, a Non-Interventional Study. J Pediatr 2015;167:1389-96. [Crossref] [PubMed]
- Miller BS, Aydin F, Lundgren F, et al. Stimulant use and its impact on growth in children receiving growth hormone therapy: an analysis of the KIGS International Growth Database. Horm Res Paediatr 2014;82:31-7. [Crossref] [PubMed]
- Renes JS, de Ridder MA, Breukhoven PE, et al. Methylphenidate and the response to growth hormone treatment in short children born small for gestational age. PLoS One 2012;7:e53164. [Crossref] [PubMed]
- Mazziotti G, Giustina A. Glucocorticoids and the regulation of growth hormone secretion. Nat Rev Endocrinol 2013;9:265-76. [Crossref] [PubMed]
- Allen DB. Growth suppression by glucocorticoid therapy. Endocrinol Metab Clin North Am 1996;25:699-717. [Crossref] [PubMed]
- Nilsson O, Marino R, De Luca F, et al. Endocrine regulation of the growth plate. Horm Res 2005;64:157-65. [PubMed]
- Johnson M. Pharmacodynamics and pharmacokinetics of inhaled glucocorticoids. J Allergy Clin Immunol 1996;97:169-76. [Crossref] [PubMed]
- 2015 National Health Interview Survey (NHIS) Data. Current asthma population estimates. Available online: https://www.cdc.gov/asthma/nhis/2015/table3-1.htm
- 2015 National Health Interview Survey (NHIS) Data. Current asthma prevalence percents. Available online: https://www.cdc.gov/asthma/nhis/2015/table4-1.htm
- Allen DB. Inhaled corticosteroids and growth: still an issue after all these years. J Pediatr 2015;166:463-9. [Crossref] [PubMed]
- Daley-Yates PT. Inhaled corticosteroids: potency, dose equivalence and therapeutic index. Br J Clin Pharmacol 2015;80:372-80. [Crossref] [PubMed]
- Becker AB, Kuznetsova O, Vermeulen J, et al. Linear growth in prepubertal asthmatic children treated with montelukast, beclomethasone, or placebo: a 56-week randomized double-blind study. Ann Allergy Asthma Immunol 2006;96:800-7. [Crossref] [PubMed]
- Sharek PJ, Bergman DA. The effect of inhaled steroids on the linear growth of children with asthma: a meta-analysis. Pediatrics 2000;106:E8. [Crossref] [PubMed]
- Childhood Asthma Management Program Research Group, Szefler S, Weiss S, et al. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000;343:1054-63. [Crossref] [PubMed]
- Pauwels RA, Pedersen S, Busse WW, et al. Early intervention with budesonide in mild persistent asthma: a randomised, double-blind trial. Lancet 2003;361:1071-6. [Crossref] [PubMed]
- Allen DB, Bronsky EA, LaForce CF, et al. Growth in asthmatic children treated with fluticasone propionate. Fluticasone Propionate Asthma Study Group. J Pediatr 1998;132:472-7. [Crossref] [PubMed]
- Sorkness CA, Lemanske RF Jr, Mauger DT, et al. Long-term comparison of 3 controller regimens for mild-moderate persistent childhood asthma: the Pediatric Asthma Controller Trial. J Allergy Clin Immunol 2007;119:64-72. [Crossref] [PubMed]
- Skoner DP, Maspero J, Banerji D, et al. Assessment of the long-term safety of inhaled ciclesonide on growth in children with asthma. Pediatrics 2008;121:e1-14. [Crossref] [PubMed]
- Zhang L, Prietsch SO, Ducharme FM. Inhaled corticosteroids in children with persistent asthma: effects on growth. Evid Based Child Health 2014;9:829-930. [Crossref] [PubMed]
- Pruteanu AI, Chauhan BF, Zhang L, et al. Inhaled corticosteroids in children with persistent asthma: dose-response effects on growth. Evid Based Child Health 2014;9:931-1046. [Crossref] [PubMed]
- Skoner DP, Meltzer EO, Milgrom H, et al. Effects of inhaled mometasone furoate on growth velocity and adrenal function: a placebo-controlled trial in children 4-9 years old with mild persistent asthma. J Asthma 2011;48:848-59. [Crossref] [PubMed]
- Kelly HW, Sternberg AL, Lescher R, et al. Effect of inhaled glucocorticoids in childhood on adult height. N Engl J Med 2012;367:904-12. [Crossref] [PubMed]
- Agertoft L, Pedersen S. Effect of long-term treatment with inhaled budesonide on adult height in children with asthma. N Engl J Med 2000;343:1064-9. [Crossref] [PubMed]
- Van Bever HP, Desager KN, Lijssens N, et al. Does treatment of asthmatic children with inhaled corticosteroids affect their adult height? Pediatr Pulmonol 1999;27:369-75. [Crossref] [PubMed]
- Wolfgram PM, Allen DB. Effects of Inhaled Corticosteroids on Growth, Bone Metabolism, and Adrenal Function. Adv Pediatr 2017;64:331-45. [Crossref] [PubMed]
- Wolfgram PM, Allen DB. Factors influencing growth effects of inhaled corticosteroids in children. J Allergy Clin Immunol 2015;136:1711-2.e2. [Crossref] [PubMed]
- Storr J, Lenney CA, Lenney W. Nebulised beclomethasone dipropionate in preschool asthma. Arch Dis Child 1986;61:270-3. [Crossref] [PubMed]
- Wasserman RL, Baker JW, Kim KT, et al. Efficacy and safety of inhaled fluticasone propionate chlorofluorocarbon in 2- to 4-year-old patients with asthma: results of a double-blind, placebo-controlled study. Ann Allergy Asthma Immunol 2006;96:808-18. [Crossref] [PubMed]
- Bisgaard H, Allen DB, Milanowski J, et al. Twelve-month safety and efficacy of inhaled fluticasone propionate in children aged 1 to 3 years with recurrent wheezing. Pediatrics 2004;113:e87-94. [Crossref] [PubMed]
- Guilbert TW, Morgan WJ, Zeiger RS, et al. Long-term inhaled corticosteroids in preschool children at high risk for asthma. N Engl J Med 2006;354:1985-97. [Crossref] [PubMed]
- De Leonibus C, Attanasi M, Roze Z, et al. Influence of inhaled corticosteroids on pubertal growth and final height in asthmatic children. Pediatr Allergy Immunol 2016;27:499-506. [Crossref] [PubMed]
- Kapadia CR, Nebesio TD, Myers SE, et al. Endocrine Effects of Inhaled Corticosteroids in Children. JAMA Pediatr 2016;170:163-70. [Crossref] [PubMed]


