Minimal-invasive approach reduces cardiopulmonary complications in elderly after lung cancer surgery
Introduction
Lung cancer is the leading cause of cancer deaths in Europe, accounting for an estimated 388,000 deaths in 2018 (1). Radical surgical resection still is the main curative treatment modality for patients with early stage lung cancer, even for high-risk patients, including high age (2,3).
Due to ageing population a worldwide increase of surgery for lung cancer in elderly patients is being observed (4). The definition of elderly varies in different publications. While the World Health Organization defines elderly as persons over the age of 65 there is a clear trend to an upward shift over the last years, reaching up to octogenarians.
Surgery in elderly can be associated with a relatively high perioperative morbidity of up to 55.8% (5-7). However, chronological age alone is not anymore a contraindication for lung cancer surgery (8-10). Recent publications have shown an acceptable postoperative morbidity and mortality in elderly patients (11,12). Even in octogenarians, the morbidity and the mortality rates were 8.4–48.0% and 1.1–8.8%, respectively; the 5-year overall survival rate was 27.0–57.5% (12). A thorough preoperative functional evaluation can guide the clinically challenging decision, taking the variety of comorbidities as well as the functional, nutritional and social status into consideration.
A number of papers tried to answer the question whether lung cancer surgery is justified in elderly patients or not (13-15). Risk factors included male gender and operation time (12). However, there is only limited evidence regarding the role of surgical approach in the early postoperative outcome in these patients (11). Minimal-invasive techniques including video-assisted thoracoscopic surgery (VATS) represent a safe and efficient surgical approach for early-stage lung cancer in elderly patients (16). VATS is recommended as an acceptable approach for early stage lung cancer (17) (NCCN 2019).
The aim of the study is to investigate the risk factors of postoperative complications in elderly (>70 years of age) early-stage lung cancer patients at our institution and to answer the question which surgical approach leads to a better early postoperative outcome.
Methods
A retrospective analysis was performed in patients who underwent curative intent anatomical resection for histologically confirmed, clinical stage T1/2 lung cancer (UICC 7th edition of TNM classification and staging system) at our institution. Our prospectively maintained ESTS database of all patients undergoing thoracic surgery for lung cancer was used to identify those patients. Written informed consent was given by all patients and the study was conducted following the approval of the local Ethics Committee (18-8030-BO). Patients with small cell lung cancer, preoperative chemo- or radiotherapy were excluded. Clinical characteristics included age, gender, BMI, functional status, preoperative comorbidity, lung function, tumor histology, clinical and pathological stage (C-stage and P-stage), operative procedure and approach, postoperative cardiopulmonary complications, 30- and 90-day mortality and length of hospital stay. All patients were staged according to the UICC 7th edition of TNM classification and staging system. The extent of lung resection was determined based on the preoperative evaluation criteria proposed by the ESTS-guidelines (8).
All procedures were performed under general anesthesia with single lung ventilation. Postoperative pain management was provided either by continuous administration of epidural (usually fentanyl with bupivacaine 0.05%) until chest drain removal or a combination of an opioid (oxycodone) with a nonsteroidal anti-inflammatory medication (metamizole) at the maximum dose. In all minimal-invasive procedures and in cases where an epidural anesthesia was contraindicated an intercostal block (20 mL Ropivacaine 1%) was utilized. After surgery, all the patients participated in active physiotherapy provided by the physiotherapy department of the certified lung cancer center.
The minimal-invasive approach was the preferred approach. It was the surgeon’s decision to do a uni-, bi- or triportal VATS. Robotic-assisted thoracoscopic surgery (RATS) was done using the Da Vinci robotic system with the 3- or 4-arm robotic approach in selected patients. Conversion from VATS or RATS to a thoracotomy was performed in case of an uncontrollable bleeding or extended adhesions. An open approach (anterolateral, muscle-sparing thoracotomy) was chosen in case of central tumors, bronchial or vascular sleeve resections or extended adhesions. A complete systematic mediastinal and hilar lymph node dissection was performed in all operations (18).
Major cardiopulmonary (MCP) complications were defined according to general thoracic surgery database definitions of the European Society of Thoracic Surgery (ESTS) and Society of Thoracic Surgery (STS) definition (19) as pneumonia, respiratory failure, acute respiratory distress syndrome (ARDS), atelectasis requiring bronchoscopy, initial ventilator support >48 h, reintubation, atrial and ventricular arrhythmias, myocardial infarction, arrhythmia, renal failure, cerebrovascular complications, deep vein thrombosis (DVT) and pulmonary embolism. Operative mortality was defined as all, in- or out-hospital deaths occurring within 30 or 90 days of surgery. The incidence of postoperative cardiopulmonary complications, length of hospital stay and early postoperative outcome (30- and 90-year mortality) were recorded.
The data are presented as frequency and percentage for categorical variables and as median and range for continuous variables. The Wilcoxon rank test were used to compare continuous variables and the chi-square or Fisher’s exact tests were used for categorical variables. P value less than 0.05 was considered significant. The statistical software GraphPad Prism 5.0 (GraphPad Software, La Jolla, CA, USA) was used for all analyses.
Results
The review of the prospective thoracic surgical cases performed from January 2016 to November 2018 identified 505 patients who fulfilled the inclusion criteria. There were 278 males and 227 females, ranging in age from 39 to 88 years (median age of 66). Two groups were studied according to age (<70 years old, 315, 62% and ≥70 years old, 190, 38%) (Table 1). A significantly higher proportion of the elderly patients were male (65%, P=0.009). There was no difference in the preoperative lung function parameters FEV1% and DLCO% (Table 1). Of note, we found a small but significant increase in the proportion of patients with higher BMI (>30) in the below 70 years old subcohort. The main histology was adenocarcinoma (56%) followed by squamous cell carcinoma (32%) and others (12%). Of note, squamous cell carcinoma was significantly more frequent in elderly patients when compared to younger ones (39% vs. 29%). Pathological T2 tumors were significantly more frequent in elderly individuals in comparison to younger patients (49% vs. 40%, P=0.033). The predominant resection type was lobectomy and bilobectomy, whereas pneumonectomy was only performed in 4 patients of each group. Sublobar resection was performed in 7% of all cases. Regarding surgical approach there was no significant difference between elderly or younger patients. In each age group an analysis regarding the surgical approach (minimal-invasive vs. open) was performed. There was a balance between open and minimal-invasive approach (52% vs. 48%). Of all patients, 241, 218 and 46 underwent thoracotomy, VATS and RATS, respectively (Table 1).

Full table
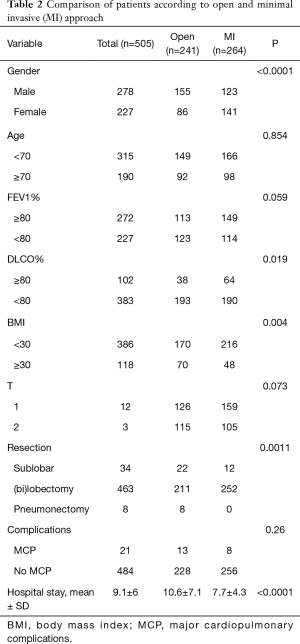
With regards to the comparison of minimally invasive and open groups, open approach was more often employed in male patients while female patients were more frequently operated by a minimally invasive technique (Table 2). Furthermore, the lung function parameters were in part different in the two operation technique groups (Table 2). As expected, the hospital stay was significantly shorter for patients with minimally invasive operations.
Full table
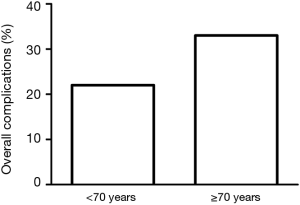
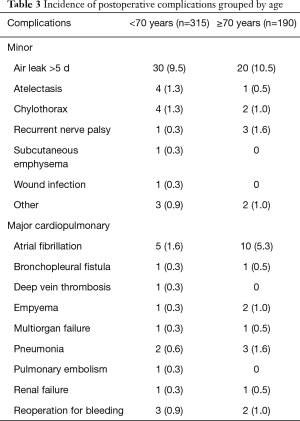
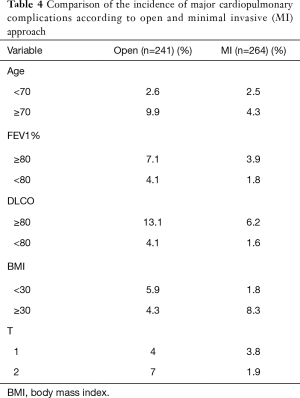
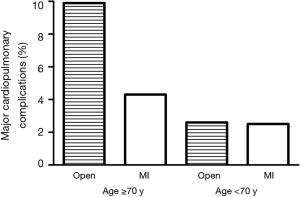
The overall complication rate was 26% in the whole cohort. Table 3 lists all the postoperative complications in detail. The only significant difference was found in atrial fibrillation (P=0.028). The overall complication rate was significantly higher in the elderly group (33% vs. 22%, P=0.0085) (Figure 1). Major cardiopulmonary complications were observed in 4.2% (n=21) patients. One out of 8 pneumonectomy patients had MCP (12.5%), while MCP rates in sublobar resection (2.9%) and (bi)lobectomy (4.1%, P=1.0) were similar. There was no significant difference in major cardiopulmonary complication rate following minimally invasive surgery between patients above or below 70 years of age (4.3% vs. 2.5%, P=0.47). In contrast, major cardiopulmonary complication rate was significantly higher in elderly thoracotomy patients than in patients below 70 years of age (9.9% vs. 2.6%, P=0.035) (Table 4, Figure 2). There was a significant difference in MCP when comparing open and minimal-invasive technique taking age into account (P=0.025). The hospital stay was significantly shorter in elderly patients operated by minimal-invasive compared to open approach (8.1 vs. 11.9 days, P<0.0001). Thirty- and 90-day mortality was comparable with 1.4% and 1.5%, respectively.
Full table
Full table
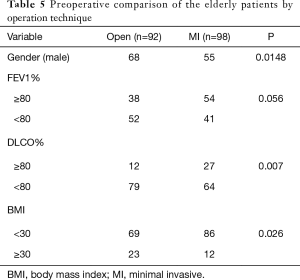
Finally, we further analysed the elderly patient cohort in terms of gender, preoperative lung function and BMI focusing on the open and minimally invasive techniques. Table 5 shows that elderly thoracotomy patients had worse lung function and were more frequently male or obese. Important to note that despite these findings two thirds of the patients with MCP had above 80 FEV1% and more than half of them above 80 DLCO% which is a higher proportion than in the overall patient cohort.
Full table
Discussion
Surgery for lung cancer in elderly patients is increasing worldwide. In the past years, many centers investigated the safety and outcome of lung cancer surgery in elderly patients, mostly in Asian population.
In our study, we collected data of Caucasian patients with clinical T1/2 lung cancer. In our cohort a low incidence of major cardiopulmonary complications was observed. In the minimally invasive cohort, we found no significantly higher rate of major cardiopulmonary complications in the elderly when compared to the younger patients. The main finding was that elderly patients operated by minimal-invasive approach had a significantly lower rate of major cardiopulmonary complications than the elderly thoracotomy group. This suggests that elderly patients may profit more from a minimal-invasive approach. This is consistent with the findings of other authors (14). Port and colleagues reported that VATS independently predicted less postoperative complications after lobectomy for NSCLC in octogenarians (20). Cattaneo et al. found that postoperative complications after pulmonary lobectomy in an elderly patient population occurs with a lower frequency with a minimally invasive VATS approach compared with a traditional, rib-spreading thoracotomy (21). Stamenovic et al. stated a significantly lower rate of pulmonary complications in VATS patients in patients older than 70 years (22). In the study by Cattaneo et al., the rate of pulmonary complications in the thoracotomy group was slightly higher than in the VATS group. This is similar to our finding supporting that minimal-invasive approach limits the chest wall trauma, which in turn lowers the pulmonary morbidity (21).
In our series, the operative mortality was lower than that in other series (23), probably because of the higher number of octogenarians and the relatively large number of patients with pneumonectomy in their cohorts.
Shorter length of hospital stay in elderly patients operated by minimal-invasive approach compared to open approach is consistent with many authors (23). In our study, we observed that the minimal-invasive group had a shorter median length of stay compared with the thoracotomy group by 3.8 days. The difference is even more obvious than in the group Cattaneo investigated (21). In the era of enhanced recovery after surgery (ERAS) (24) the utilization of minimal-invasive techniques, especially in high-risk patients will increasingly play a pivotal role.
Our study tried to answer a relevant and timely issue in an era of increasingly ageing lung cancer patients presented for surgery. The patient data collection including the complications using the ESTS database guaranteed a uniform and consistent recording. However, this study has some limitations. Due to its retrospective design there is a selection bias. In our study elderly was defined as age ≥70 years, and this varies in literature. Furthermore, we did not match patients in the groups. Nevertheless, both age groups were balanced with no major differences in the pattern of the different clinicopathological variables. Moreover, it was the surgeon’s decision what kind of minimal-invasive approach to be used. In our study, we focused on clinical T1/2 lung cancer patients.
Our study emphasizes that pulmonary resection for lung cancer in elderly patients is safe and can be performed with a low morbidity and mortality. In this high-risk population, the utilization of minimal-invasive surgery is associated with a reduced rate of major cardiopulmonary complications and may therefore be the preferred approach. Additional prospective studies are needed to confirm these findings.
Acknowledgments
We thank Ms Baerbel Eigendorf for her continuous support in data maintenance and data extraction.
Funding: This study was supported by the open access fund of the University Duisburg-Essen.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.03.73). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was given by all patients and the study was conducted following the approval of the local Ethics Committee (18-8030-BO).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ferlay J, Colombet M, Soerjomataram I, et al. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer 2018;103:356-87. [Crossref] [PubMed]
- Postmus PE, Kerr KM, Oudkerk M, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2017;28:iv1-iv21. [Crossref]
- Donington J, Ferguson M, Mazzone P, et al. American College of Chest Physicians and Society of Thoracic Surgeons consensus statement for evaluation and management for high-risk patients with stage I non-small cell lung cancer. Chest 2012;142:1620-35. [Crossref] [PubMed]
- Lutz W, Sanderson W, Scherbov S. The coming acceleration of global population ageing. Nature 2008;451:716-9. [Crossref] [PubMed]
- Dell'Amore A, Monteverde M, Martucci N, et al. Lobar and sub-lobar lung resection in octogenarians with early stage non-small cell lung cancer: factors affecting surgical outcomes and long-term results. Gen Thorac Cardiovasc Surg 2015;63:222-30. [Crossref] [PubMed]
- Fanucchi O, Ambrogi MC, Dini P, et al. Surgical treatment of non-small cell lung cancer in octogenarians. Interact Cardiovasc Thorac Surg 2011;12:749-53. [Crossref] [PubMed]
- Rueth NM, Parsons HM, Habermann EB, et al. Surgical treatment of lung cancer: predicting postoperative morbidity in the elderly population. J Thorac Cardiovasc Surg 2012;143:1314-23. [Crossref] [PubMed]
- Brunelli A, Charloux A, Bolliger CT, et al. The European Respiratory Society and European Society of Thoracic Surgeons clinical guidelines for evaluating fitness for radical treatment (surgery and chemoradiotherapy) in patients with lung cancer. Eur J Cardiothorac Surg 2009;36:181-4. [Crossref] [PubMed]
- Rivera C, Dahan M, Bernard A, et al. Surgical treatment of lung cancer in the octogenarians: results of a nationwide audit. Eur J Cardiothorac Surg 2011;39:981-6. [Crossref] [PubMed]
- Dell'Amore A, Monteverde M, Martucci N, et al. Early and long-term results of pulmonary resection for non-small-cell lung cancer in patients over 75 years of age: a multi-institutional study. Interact Cardiovasc Thorac Surg 2013;16:250-6. [Crossref] [PubMed]
- Pei G, Zhou S, Han Y, et al. Risk factors for postoperative complications after lung resection for non-small cell lung cancer in elderly patients at a single institution in China. J Thorac Dis 2014;6:1230-8. [PubMed]
- Hino H, Karasaki T, Yoshida Y, et al. Risk factors for postoperative complications and long-term survival in lung cancer patients older than 80 years. Eur J Cardiothorac Surg 2018;53:980-6. [Crossref] [PubMed]
- Tutic-Horn M, Gambazzi F, Rocco G, et al. Curative resection for lung cancer in octogenarians is justified. J Thorac Dis 2017;9:296-302. [Crossref] [PubMed]
- Berry MF, Onaitis MW, Tong BC, et al. A model for morbidity after lung resection in octogenarians. Eur J Cardiothorac Surg 2011;39:989-94. [Crossref] [PubMed]
- Chambers A, Routledge T, Pilling J, et al. In elderly patients with lung cancer is resection justified in terms of morbidity, mortality and residual quality of life? Interact Cardiovasc Thorac Surg 2010;10:1015-21. [Crossref] [PubMed]
- Mun M, Kohno T. Video-assisted thoracic surgery for clinical stage I lung cancer in octogenarians. Ann Thorac Surg 2008;85:406-11. [Crossref] [PubMed]
- Ettinger DS, Aisner DL, Wood DE, et al. NCCN Guidelines Insights: Non-Small Cell Lung Cancer, Version 5.2018. J Natl Compr Canc Netw 2018;16:807-21. [Crossref] [PubMed]
- Lardinois D, De Leyn P, Van Schil P, et al. ESTS guidelines for intraoperative lymph node staging in non-small cell lung cancer. Eur J Cardiothorac Surg 2006;30:787-92. [Crossref] [PubMed]
- Fernandez FG, Falcoz PE, Kozower BD, et al. The Society of Thoracic Surgeons and the European Society of Thoracic Surgeons general thoracic surgery databases: joint standardization of variable definitions and terminology. Ann Thorac Surg 2015;99:368-76. [Crossref] [PubMed]
- Port JL, Mirza FM, Lee PC, et al. Lobectomy in octogenarians with non-small cell lung cancer: ramifications of increasing life expectancy and the benefits of minimally invasive surgery. Ann Thorac Surg 2011;92:1951-7. [Crossref] [PubMed]
- Cattaneo SM, Park BJ, Wilton AS, et al. Use of video-assisted thoracic surgery for lobectomy in the elderly results in fewer complications. Ann Thorac Surg 2008;85:231-5; discussion 235-6. [Crossref] [PubMed]
- Stamenovic D, Messerschmidt A, Schneider T. Surgery for lung tumors in the elderly: A retrospective cohort study on the influence of advanced age (over 80 years) on the development of complications by using a multivariate risk model. Int J Surg 2018;52:141-8. [Crossref] [PubMed]
- Detillon DDEMA, Veen EJ. Postoperative Outcome After Pulmonary Surgery for Non-Small Cell Lung Cancer in Elderly Patients. Ann Thorac Surg 2018;105:287-93. [Crossref] [PubMed]
- Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS(R)) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;55:91-115. [Crossref] [PubMed]