
Chronic respiratory diseases global mortality trends, treatment guidelines, life style modifications, and air pollution: preliminary analysis
WHO: lessons learnt on noncommunicable disease (NCD) control
Billions of people around the world are affected by NCDs, which comprised 71% of global mortality (41 million) of the 57 million deaths which occurred globally. NCD burden is greatest within low- and middle-income countries (LMIC), where 78% of all NCD deaths and 85% of premature deaths were registered. Cardiovascular diseases (CVD) (31%), cancers (16%), chronic respiratory diseases (CRDs) (7%), and diabetes (3%) these four diseases are largely preventable through public policies that tackle their common risk factors: tobacco use, harmful use of alcohol, unhealthy diets, physical inactivity and air pollution (1).
In the year 2000 foreseeing this situation and taking into account enormous burden of NCD, the 53 World Health Assembly (WHA) gave priority to prevention and control of NCD with special emphasis on developing countries and other deprived populations (WHA resolution 53.17 May 2000) and a lot of activities and programmes have been initiated mainly by the health sectors to globally address this problem.
The Moscow Declaration adopted during the First Global Ministerial Conference on Healthy Lifestyles and NCD Control (Moscow, 28–29 April 2011), underlined that besides health sector many sectors of the society, including finance, trade, agriculture, education and environment, have an impact on risk factors for NCD, and that the responsibility for the NCD agenda can no longer be delegated solely to ministries of health and requires a multisectoral approach (2).
In September 2011, at the United Nations General Assembly in New York, recognizing that NCD constitute one of the major challenges for development in the 21 century, a political declaration was made to strengthen global and national responses to prevent and control NCD (3). Presidents and Prime-Ministers committed to “strengthen their commitment, as Heads of State and Government, to provide strategic leadership for the prevention and treatment of NCD”. As part of the declaration, WHO was given a leadership role, and subsequently established the WHO Global NCD Action Plan for the Prevention and Control of NCD 2013–2020 adopted by the WHA in 2013 (4,5). The Global NCD Action Plan included nine voluntary global targets to be attained by 2025 (4) and global monitoring framework. These targets include 25% relative reduction in risk of premature mortality from major NCD, at least 10% relative reduction in the harmful use of alcohol, a 10% relative reduction in prevalence of insufficient physical activity, a 30% relative reduction in mean population intake of salt/sodium, a 30% reduction in prevalence of current tobacco use, a 25% relative reduction in the prevalence of raised blood pressure, halt the rise in diabetes and obesity, 50% drug therapy coverage and counseling to prevent heart attacks and strokes and 80% availability of basic technologies and essential medicines. Subsequently, WHO Member States agreed to a 25% reduction in premature NCD mortality by 2025 (25×25) and then adopted a set of risk factors and health system targets which, if met, would ensure achievement of the 25×25 mortality target at all stages of the life course, from childhood to old age. These targets are aligned to those for NCD included in the 2030 Agenda for Sustainable Development “by 2030, reduce, by one third, premature mortality from NCD through prevention and treatment, and promote mental health and well-being” as specified in Sustainable Development Goals (STG) target 3.4. adopted at the United Nations Summit on Sustainable Development in September 2015 (6,7) and the WHO 13th General Programme of Work 2019–2023 adopted by the WHA in May2018 (8,9).
Five years after adoption of NCD Action Plan and 3 years after formulation of the STG target 3.4, the WHO Independent High-level Commission on NCD was convened in June 2018 by the WHO Director-General to advise him on bold recommendations on how countries can accelerate progress towards SDG target 3.4 on the prevention and treatment of NCD and the promotion of mental health and well-being. The commission stated that although the number of premature deaths has risen in the years 2000 to 2015, the probability of dying from any one of the four major NCD is declining. This is mainly a result of two factors: a growing population aged 30 to 70 years, and falling mortality in only two categories, CVD and CRD. However, the global rate of decline, 17% between 2000 and 2015, is still not enough to meet the target of a one-third reduction in premature mortality from NCD by 2030, as specified in SDG target 3.4. To date, the most significant reductions in CVD mortality have been achieved through comprehensive tobacco control and comprehensive CVD prevention and treatment programmes (10).
Commission gives no comments concerning reduction in CRD mortality which is one of the major NCD sharing common risk factors and responsible for 7% of total mortality. In view of this we decided to analyze CRD mortality trends associated with implementation of therapeutic guidelines and achievements of the life style modifications against major risk factors along the lines of the WHO global monitoring mechanism (11). Since monitoring mechanism has no data on air pollution which plays an important role in the CRD mortality, we used the information from NCD country profiles 2018 regarding the air pollution level as well as some additional information on CRD treatment (1). Lessons learned could be useful to identify whether countries analyzed are on the right track to achieve 25×25 and SDG 3.4 goals.
WHO: statistics we have and what we can do
Mortality trends
There are different approaches for the analysis of global mortality trends (12) and assessment of different interventions (13). WHO statistics based on the Member States countries unified mortality and causes of death reports is the best source of data for analyzing global NCD mortality trends, and making comparisons and assessments of different types of community-based, country wide interventions (14). Trends from 2000 are based on analysis of latest available national information on levels of mortality and cause distributions as at the beginning of 2018 together with latest available information from usually global WHO programs for causes of public health importance. Analysis includes estimates of age-standardized death rates (ASDR) per 100,000 population by cause, sex and age for Member States. Only countries with multiple years of national death registration data with high completeness and quality of cause-of-death assignment are included in the analysis. Estimates for these countries may be compared and time series may be used for priority setting and policy evaluation. Due to changes in data and some methods, these estimates are not comparable to previously-released WHO estimates. The preparation of these statistics was undertaken by the WHO Department of Information, Evidence and Research in collaboration with WHO technical programs. Documentation and regional-level summary tables are available on the WHO website (14).
Treatment initiatives
Management guidelines
Development in majority countries have been influenced by WHO initiated global initiatives on CRD management: Global Initiative for Asthma (GINA), Global Initiative for Obstructive Lung Disease (GOLD), Allergic Rhinitis and its Impact on Asthma (ARIA), Practical Approach to Lung Health (PAL), Package of Essential Noncommunicable Disease Interventions for Primary Health Care in Low-Resource Settings (PEN), and Global Alliance against Chronic Respiratory Diseases (GARD) country activities initiated and implemented during the assessment period 2000–2016 (15). Above mentioned international treatment guidelines in many countries after adaptation were used for development of national treatment guidelines. Their availability were assessed based on the Member State responses to the 2017 NCD Country Capacity Survey (11) on the evidence-based national guidelines/protocols/standards for the management of major NCD (CVD, cancer, CRD and diabetes) through a primary care approach, recognized/approved by government or competent authorities.
Availability of essential NCD medicines and basic technologies
Essential medicines to treat major NCD were based on the availability of the 10 NCD medicines which include aspirins, statins, angiotensin-converting enzyme inhibitors, thiazide diuretics, long-acting calcium channel blockers, beta-blockers, insulin, metformin, bronchodilators, and inhaled corticosteroids (ICS).
For our purposes we analyzed availability of the short acting bronchodilators and ICS.
The six basic technologies include blood pressure measurement device, weighing scales, height measuring equipment, blood sugar and blood cholesterol measurement devices with strips, and urine strips for albumin assay (1). Among basic technologies we could not find highly relevant for CRD items.
Life style modifications and risk factors
To address the growing burden of NCD, WHO identified a package of 16 “best buy” interventions that are cost-effective, affordable, feasible and scalable in all settings. The “best buys” were well described and introduced in 2010 (16) and were updated in 2017 based on the latest evidence of intervention impact and costs (17). From a financing perspective, these interventions are a practical and achievable starting point for incorporating NCD interventions into health benefit packages for universal health coverage (UHC), costing as little as $1 per person, per year, in lower-income settings between 2018 and 2025, and in the case of taxation not only delivering health benefits but also generating additional government revenues (18). Implementing all 16 “best buys” in all countries between 2018 and 2025 would avoid 9.6 million premature deaths, thus moving countries appreciably towards the NCD mortality reduction targets.
CRD attributable “best buys” concern tobacco use, unhealthy diet, and physical inactivity. Although there is no data that harmful use of alcohol has an impact on CRD mortality (19), this ”best buy” should be also considered in view of its link with other behavioral risk factors like smoking and diet. To quantify the level of Life-style modifications achievement, we gave to fully achieved activities 2 points, partially achieved 1 point, not achieved, no response or don’t know 0 point.
We analyzed the following activities:
Tobacco demand reduction measures
Implementation by Member State the following five demand-reduction measures of the WHO Framework Convention on Tobacco Control (FCTC): (I) reduce affordability by increasing excise taxes and prices on tobacco products; (II) eliminate exposure to second-hand tobacco smoke in all indoor workplaces, public places and public transport; (III) implement plain/standardized packaging and/or large graphic health warnings on all tobacco packages; (IV) enact and enforce comprehensive bans on tobacco advertising, promotion and sponsorship; (V) implement effective mass media campaigns that educate the public about the harms of smoking/tobacco use and second hand smoke.
Harmful use of alcohol reduction measures
Member State has implemented, as appropriate according to national circumstances, the following three measures to reduce the harmful use of alcohol as per the WHO Global Strategy to Reduce the Harmful Use of Alcohol: (I) enact and enforce restrictions on the physical availability of retailed alcohol (via reduced hours of sale); (II) advertising bans (across multiple types of media), or comprehensive restrictions; (III) increase excise taxes on alcoholic beverage.
Unhealthy diet reduction measures
Member State has implemented the following measures to reduce unhealthy diets: (I) adopt national policies to reduce population salt/sodium consumption; (II) adopt national policies that limit saturated fatty acids and virtually eliminate industrially produced trans fatty acids (TFAs) in the food supply.
Public education and awareness campaign on physical activity
Member State has implemented at least one recent national public awareness and motivational communication for physical activity, including mass media campaigns for physical activity behavioral change.
Obesity control is not on the “best buy” list but this risk factor (20) could be also an indicator of physical inactivity and unhealthy diet. Obesity [2016] was assessed in adults as the percentage of the population aged18 years and older having a body mass index (BMI) ≥30 kg/m2, and in adolescents as the percentage of the population aged 10–19 years who are more than 2 SD above the median of the WHO growth reference for children and adolescents (1).
Air pollution both indoor and outdoor should be also taken into account as a major public health problem and one of the key underlying causes of death due to CRD (1) Ambient air pollution in 2016 was assessed as the exceedance of the WHO guideline level for annual mean concentration of particles of ≤2.5 micrometres in the air (proportion) and Household air pollution in 2016 by the percentage of the population with primary reliance on polluting fuels and technologies (1).
WHO: the results we have achieved
Mortality estimates
Total CRD mortality from 2000 to 2016 was analyzed in 49 countries with the interim analysis in 2010 and 2015. Only data based on the multiple years of national death registration data with high completeness and quality of cause of death assignment were used in the analysis. Estimates for these countries may be compared and time series may be used for priority settings and policy evaluation (14). 36 countries (Australia, Austria, Bahamas, Belgium, Brunei Darussalam, Canada, Chile, Croatia, Czechia, Denmark, Estonia, Finland, France, Germany, Hungary, Iceland, Ireland, Israel, Italy, Japan, Latvia, Lithuania, Luxemburg, Malta, Netherlands, New Zealand, Norway, Republic of Korea, Slovakia, Slovenia, Spain, Sweden, Switzerland, Trinidad and Tobago, United Kingdom, United States of America) belong to high income countries (HIC) according to the World Bank classification (21) and 13 countries (Armenia, Brazil, Cuba, Grenada, Guatemala, Kyrgyzstan, Mauritius, Mexico, Republic of Moldova, Romania, Saint Vincent and the Grenadines, the Former Yugoslav Republic of Macedonia, Uzbekistan) belong to middle income countries (MIC).
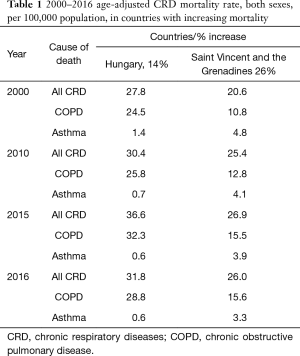
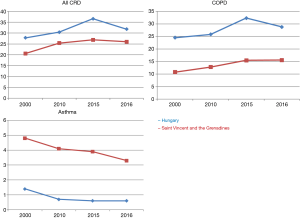
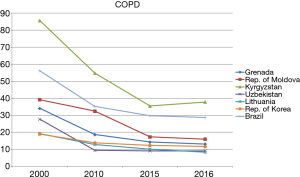
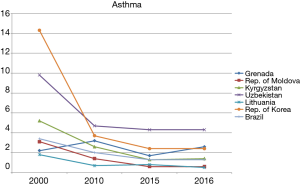
Baseline (year 2000) age-standardized mortality rate in MIC was (47.1±22.6) per 100,000, and in HIC (29.2±11.5) per 100,000 (t=2.73, P<0.01). In average by the year 2016, total CRD mortality declined by 24% in 49 countries. Most visible decline was observed for the first decade from 2000 to 2010. Total CRD mortality has declined by 23% in 43 countries did not changed in two or increased in 4 countries by 7%. To see the difference in CRD mortality decline from 2000 to 2016 in countries with different level of income, we compared 35 HIC and 12 MIC. Hungary and Saint Vincent and the Grenadines were excluded from the analysis because mortality in these countries increased by 14% and 26% accordingly mainly due to chronic obstructive pulmonary disease (COPD) mortality which was growing until 2015 in both countries, then stabilized in Saint Vincent and the Grenadines or began declining in Hungary. On the other hand asthma mortality was gradually declining in St Vincent and the Grenadines and stabilized after 2015 in Hungary (Table 1,Figure 1).
Full table
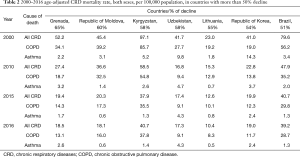
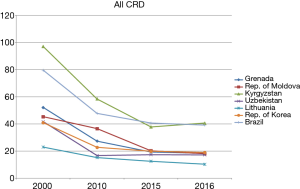
Mean decline of CRD mortality was 23% in HIC and 36% in MIC. It means that higher baseline mortality rate seen in MIC is associated with more visible decline in CRD mortality rate. ASDR and trends in countries with highest, more than 50%, decline (Grenada 65%, Republic of Moldova 60%, Uzbekistan 58%, Kyrgyzstan 58%, Lithuania 55%, Republic of Korea 54% and Brazil 51%) are presented in Table 2 and Figure 2. Five of these countries belong to MIC, upper middle income Grenada and Brazil and lower middle income Republic of Moldova, Uzbekistan and Kyrgyzstan. Lithuania and Republic of Korea belong to HIC. Within the total CRD mortality COPD provides from 46% to 86%, while asthma is responsible for 4–35% of all CRD deaths. It means like in the previous case with increasing CRD mortality COPD is responsible for the majority of CRD deaths. It’s an important observation when we analyze total mortality based on asthma and COPD data since correlations of these diseases with known risk factors are different. It’s interesting that before 2010 CRD mortality declined in all selected countries, after 2010 CRD and COPD mortality continued to decline in six selected countries (Figure 2), becoming less steep in Republic of Korea or even slightly increasing in Uzbekistan. These CRD mortality trends are mainly caused by COPD (Figure 3) while asthma trends demonstrate different direction for instance for Grenada and Lithuania (Figure 4).
Full table
To see the association of CRD treatment status and life style modifications with CRD mortality trends after adoption of the Political Declaration on NCD and implementation of the life-style modifications (3,16) in 2010–2016, we analyzed 28 HIC (Australia, Austria, Bahamas, Belgium, Brunei Darussalam, Canada, Chile, Croatia, Denmark, Estonia, Finland, France, Iceland, Ireland, Italy, Latvia, Lithuania, Luxemburg, Netherlands, New Zealand, Norway, Republic of Korea, Slovakia, Slovenia, Spain, Switzerland, Trinidad and Tobago, United Kingdom) and 8 MIC (Armenia, Brazil, Grenada, Guatemala, Kyrgyzstan, Mexico, Republic of Moldova, Romania) where mortality decreased. At the same time period CRD mortality increased in 13 countries 5 MIC (Cuba, Uzbekistan, The Former Yugoslav Republic of Macedonia, Mauritius, Saint Vincent and the Grenadines) and 8 HIC (Czechia, Israel, Germany, Hungary, Japan, Malta, Sweden and United States of America).
National CRD management guidelines by the year 2016 existed in 34 countries (94%) where the mortality declined and in 11 countries (85%) with increasing mortality. Availability of essential CRD drugs in countries with increased mortality was 69% (9 countries out of 13) and 89% (32 out of 36) in countries with decreasing mortality. In view of this we assume better CRD management is associated with declining CRD mortality.
Based on the WHO Progress monitor 2017, we have analyzed the following “best buy” life style modification measures: tobacco, alcohol, diet and physical activity. The quantification of interventions (see above) is based on the level of the achieved measures (Table 3).
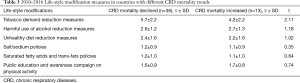
Full table
Only tobacco demand reduction measures demonstrated statistically significant difference between countries with different CRD dynamics trends. Implementation of the tobacco demand reduction measures was statistically more effective in 36 countries where CRD mortality declined ( =5.7±2.2) compared with 13 countries where CRD mortality increased (
=5.7±2.2) compared with 13 countries where CRD mortality increased ( =4.2±2.2, t=2.11, P<0.05).
=4.2±2.2, t=2.11, P<0.05).
No statistically significant differences were found for alcohol, diet and physical activity measures between the groups. It was interesting to see whether the above mentioned country-wide life-style modification measures have a link with the CRD risk factors level (Table 4). Also we found no statistically significant difference between groups we see a tendency towards a higher level of risk factors in countries with increasing CRD mortality. Obesity status remains practically the same in both groups of countries.
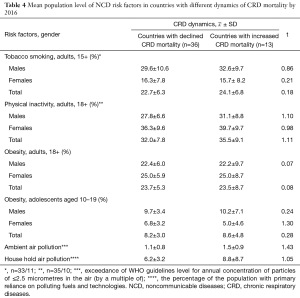
Full table
WHO: what’s important?
Increasing CRD mortality from 2000 to 2016 seen in two countries Hungary and Saint Vincent and the Grenadines could be explained by practically zero anti-tobacco activities in Saint Vincent and the Grenadine, no CRD management guidelines and lack of essential CRD medicines (1,11). In Hungary we observed fairly high for Europe prevalence of smoking 33% for males and 23% for females and twice higher than normal level of ambient air pollution. For instance HIC have 29% smoking prevalence among men and 19% among women (1).
Evidence-based national therapeutic guidelines, protocols, standards for the management of CRD through a primary health care approach, recognized or approved by government or competent authorities play a crucial role in CRD control and declining of mortality.
From 2000 to 2010 global CRD management guidelines initiated by WHO (GINA, GOLD, ARIA, PAL) and global WHO/CRD partnership (GARD) have been actively working in more than 80 countries. These evidence-based approaches worked either under their own names in many countries or have been used for development of national management protocols and supported national authorities in implementing these evidence-based guidelines (15). In all countries with positive CRD dynamics WHO introduced activities remained active. By 2010 all of them have been well functioning globally both in developed and developing countries. Among seven countries with the highest decline in CRD mortality, four countries (Kyrgyzstan, Lithuania, Republic of Korea and Brazil) are active members of WHO/GARD partnership, and Uzbekistan is actively implementing PAL which has been initiated in LMIC with successful TB control programme (22). Thus, before “best buy“ launch WHO initiated activities produced a good basis for further CRD movement and by the year 2010 we see a visible positive trend in CRD mortality in 43 countries.
We have still a fairly short period of the ”best buy” life-style modifications just 4–5 years but this approach has enormous perspective and if succeed will facilitate moving countries appreciably towards the NCD mortality reduction targets. Our analysis has demonstrated that this approach is feasible. However not all “best buy” modifications have links with CRD or have even different influence on major CRD.
Tobacco use
Last GOLD report (23) shows that across the world, cigarette smoking is the most commonly encountered risk factor for COPD. Cigarette smokers have a higher prevalence of respiratory symptoms and lung function abnormalities, a greater annual rate of decline in Forced expiratory volume in one second (FEV1), and a greater COPD mortality rate than non-smokers. Other types of tobacco (e.g., pipe, cigar, water pipe) and marijuana are also risk factors for COPD. Passive exposure to cigarette smoke, also known as environmental tobacco smoke (ETS), may also contribute to respiratory symptoms and COPD by increasing the lung’s total burden of inhaled particles and gases. Smoking during pregnancy may pose a risk for the fetus, by affecting lung growth and development in utero, and possibly the priming of the immune system.
ETS has been confirmed as a risk factor for asthma, both in childhood and adulthood. Prenatal exposure to tobacco smoke is also important. This is considered to be a causal relationship, implying that the prevalence (and severity) of asthma would reduce if exposure to tobacco smoke was reduced (24).
Global activities against tobacco led to decrease the global prevalence of tobacco smoking from 27% in 2000 to 20% (1). Our analysis demonstrates that in countries where tobacco demand-reduction measures are better accomplished total CRD mortality was declining.
Taking into account that not all people are smokers or exposed to ETS and smoking prevalence is decreasing we analyzed other NCD risk factors having impact on the whole population.
Diet
The correlation between diet and CRD is less obvious comparatively with tobacco.
Salt/sodium policies
In some population-based cross-sectional studies the association between salt intake, bronchial symptoms (25) and asthma was found in children (26). There where an improvement in pulmonary function with low salt diet (27) and promising results of trials on reduction of salt in exercise induced asthma (28). Limitation of dietary salt intake to less than 5 grams per day is a difficult task to achieve. Estimates from 2010 show that globally people consume an average of 9–12 grams of salt each day twice the recommended daily intake (1). Salt reduction policy is a key element of the WHO NCD Action Plan (4), mainly due to increase the risk of raised blood pressure, coronary heart disease (CHD) and stroke. The global NCD targets include a sodium reduction target of a 30% relative reduction in mean population salt intake by 2025. Regarding CRD we can expect some beneficial effect of this reduction on childhood asthma since there is no data on association between salt consumption and COPD a major contributor to CRD mortality.
Saturated fatty acids and trans-fats policies
There is no data that total fat consumption within WHO Population Nutrient Intake Goal 15–30% has negative effect on CRD as well as reduction of Saturated Fatty Acids intake less than 10% (20).
TFAs appear during the process of partial hydrogenation of Polyunsaturated Fatty Acids. This process creates TFA and also removes the critical double bonds in essential fatty acids necessary for the action. Most TFA are contributed by industrially hardened oils, deep fried fast foods and baked goods (29). Several large cohort studies have found that intake of TFA increase the risk of CHD, central adiposity and diabetes (30,31). However, these acids are slowly disappearing from the American diet (32). There is only very limited data about the association between consumption of TFA and asthma. In cross sectional studies higher prevalence of asthma is observed in those countries that have higher levels of TFA intake (33). Higher levels of margarine consumption are also associated with the increased risk of asthma (34,35). Two large prospective studies in US demonstrated an increased risk of development COPD in men and women associated with diet rich in desserts and French fries (36,37). In view of this saturated fatty acids and trans-fats policies could be beneficial for CRD.
Physical inactivity
Physical inactivity is closely linked with increasing magnitude of NCD. People who are insufficiently physically active have an increased risk of all-cause mortality, compared with those who engage in at least 30 minutes of moderate-intensity physical activity most days of the week. Additionally, physical activity lowers the risk of stroke, hypertension and depression (38). Recognizing these strong links between physical activity and physical and mental health, a global target of a 10% reduction in levels of physical inactivity by 2025 was adopted by Member States at the Sixty-sixth World Health Assembly in 2013 (4). In 2018, WHO launched a global action plan to promote physical activity, to provide updated guidance to countries and promote a framework of effective and feasible policy actions to increase physical activity at all levels (39). Globally in 2016, 28% three of all adults aged 18 years and older were insufficiently physically active-defined as not meeting the WHO recommendation to perform at least 150 minutes of moderate-intensity physical activity per week, or the equivalent (40). More than one third of the population was insufficiently physically active in one third of countries (55 of 168 countries). Women were less active than men, with 32% of women and 23% of men not achieving the recommended levels for physical activity. This was not only the case globally but also in 159 out of the 168 countries analyzed, and in nearly all WHO regions. There is evidence that physical activity is decreased in COPD patients (41). As such, there has been tremendous interest in implementing behavior-targeted interventions with the aim of improving physical activity. Promoting and maintaining physical activity is a key element of pulmonary rehabilitation, including community and home-based. This is an approach with clear evidence of benefits (42).
Obesity
Obesity, including in children, is increasing in all countries, with the most rapid rises occurring in LMIC countries. Obesity is associated with premature onset of diabetes or heart disease, increased risk of other NCD, and has the potential to negate many of the health benefits that have contributed to increased life expectancy. Governments need to accept primary responsibility for taking action, along with other actors, to create an enabling environment and to promote equitable coverage of interventions to reduce unhealthy diets (high in sugars, fats, and sodium) and physical inactivity to all age groups, including integration within UHC (1,43). Obesity appears to be associated with the increased prevalence of asthma and lower lung function in developed (44-47) and developing countries as well as in deprived populations (48,49). Fast food restaurant attendance may be a risk factor for asthma (50). Moreover, in asthma, obesity is a risk factor for dyspnoea (51) and poor control of the disease (52). In COPD, obesity is also proposed to be a risk factor for dyspnoea and the severity of the disease (53). Although the weight loss problem in the clinical cases of COPD stands beyond the main purpose of the WHO strategy, while analyzing weight losing activities in COPD (adult) patients and asthma (often children) and obstructive sleep apnoea patients and in the whole population, it is difficult to expect achieving significant difference in obesity prevalence. Between 1975 and 2016, the worldwide prevalence of obesity nearly tripled, and continues to rise in LMIC countries, although it was once considered a problem of HIC (1). Most of the world’s population lives in countries where overweight and obesity kills more people than underweight. Shifts in eating behavior towards diets containing energy-dense foods, high in fat and sugars, and less physical activity due to the sedentary nature of many forms of work and modes of transportation are contributing to the rise in obesity. Obesity is largely preventable, and one of the global NCD targets is to halt its rise (4) which is difficult to achieve but it would have a tremendous impact on NCD mortality.
Air pollution
Air pollution, both indoor and outdoor, is a major public health problem and one of the key underlying causes for millions of deaths due to CHD, CRD, and cancers. In 2016, air pollution caused 7 million deaths globally. Among these deaths, about 80% were caused by NCD, making air pollution a major risk factor for NCD, comparable to current tobacco smoking. About 29% of adult deaths from lung cancer, 24% from stroke, and 25% from heart disease were attributable to air pollution (1). Ambient air pollution is caused mainly by inefficient energy production, industry, the domestic/residential sector, waste management and transportation, and is measured as the mean air pollution level a person is exposed to during the year as measured outdoors. In 2016, 91% of the world’s population lived in places where the air was unsafe to breathe, according to the WHO Air quality guidelines. Household air pollution is largely generated by inefficient household fuel combustion for cooking, heating and lighting purposes, leading to air pollution in and around the home. Household air pollution “leaking” outdoors is also an important source of ambient air pollution. Billions of people still rely on simple stoves, or open fires, burning solid fuels and kerosene for cooking. These polluting cooking practices produce harmful smoke in the home. While the percentage of the population with access to clean fuels and technologies is increasing in most parts of the world, the rate of increase in access is not commensurate with population growth, particularly in sub-Saharan Africa (54).
The evidence of an increased risk of asthma due to indoor air pollutants (e.g., cooking on an indoor open fire) or outdoor air pollutants (e.g., suspension particles or sulphur dioxide) is less clear and consistent than for tobacco smoke (24). Occupational exposures, including organic and inorganic dusts, chemical agents and fumes, remain an under-appreciated risk factor for COPD (55,56). There is growing evidence that indoor biomass exposure to modern and traditional fuels used during cooking may predispose women to develop COPD in many developing countries (57,58). High levels of urban air pollution are harmful to individuals with existing heart or lung disease. The role of outdoor air pollution as a risk factor for COPD is unclear, but its role appears to be relatively small in adults compared to the role of cigarette smoking (55). There is no doubt that air pollution (both indoor and outdoor) is a CRD risk factor however in view of its association with asthma and COPD more success for CRD prevention is expected from the household air control than from the outdoor measures.
Summary
Coming back to the WHO Independent High-level Commission on NCD, we can say that significant reduction in CRD mortality has been achieved from the year 2000. This effect is more visible in MIC with higher initial mortality rate. The mortality decline is associated with promotion of multiple global CRD evidence-based management initiatives initiated by WHO during last 15–20 years and taken by many countries for development and implementation of national treatment guidelines. Comprehensive tobacco control remains major, experienced (WHO FCTC was adopted in 2003 and came into force in 2005) and most successful life-style modification measure. Other “best buy” life-style modifications have a shorter exposition period and their link with CRD is less strong than tobacco. Thus we need more exposition time of these “best buy” and their cumulative effect will definitely bring about substantial decline in CRD mortality along with other major NCD provided jointly with ministries of health many other sectors, including finance, trade, agriculture, education and environment, will have an impact on risk factors for NCD. Governments need to accept primary responsibility for taking action, along with other actors, to create an enabling environment and to promote equitable coverage of interventions to reduce unhealthy diets (high in sugars, fats, and sodium) and physical inactivity to all age groups, including integration within UHC (1,43). There is increasing evidence about the role of indoor and outdoor air pollution, with its links to urbanization, in the development of NCD. Poor air quality is widespread, and in many cities, vehicles are responsible for a high proportion of pollution. Poorly designed streets and heavy traffic also discourage walking and cycling, contributing to decreased physical activity and increased levels of obesity.
Governments and communities can tackle these, and therefore must be involved and coordinated for effective action. The political choice to ensure that the national UHC public benefit package includes NCD and mental health services requires political leadership and responsibility at all levels.
Without significant investments for NCD prevention and control now, 15 million people will continue to die each year from NCD in the prime of their lives, between the ages of 30 and 70. Most of these deaths tomorrow can be avoided by Heads of State and Government making smart political choices today.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Noncommunicable Diseases Country Profiles 2018. Geneva: World Health Organization, 2018, 223. Available online: https://www.who.int/nmh/publications/ncd-profiles-2018/en
- WHO First global ministerial conference on healthy life-styles and NCDs control. Available online: http://www.who.int
- United Nations General Assembly Resolution A/RES/66/2. Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. New York: United Nations; 2012. Available online: https://digitallibrary.un.org/record/720106/files/A_RES_66_2-EN.pdf, accessed 16 August 2018.
- Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: World Health Organization, 2013. Available online: http://www.who.int/nmh/events/ncd_action_plan/en/, accessed 16 August 2018.
- World Health Assembly Resolution WHA66.10. Follow-up to the Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. Geneva: World Health Organization, 2013. Available online: http://apps.who.int/gb/ebwha/pdf_files/WHA66/A66_R10-en.pdf?ua=1, accessed 16 August 2018).
- Transforming our world: the 2030 Agenda for Sustainable Development. New York: United Nations; 2015. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld/publication, accessed 16 August 2018.
- United Nations General Assembly Resolution A/RES/70/1. Transforming our world: the 2030 Agenda for Sustainable Development. New York: United Nations; 2015. Available online: http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E, accessed 16 August 2018.
- Thirteenth General Programme of Work, 2019–2023. Geneva: World Health Organization, 2018. Available online: http://www.who.int/about/what-we-do/gpw-thirteen-consultation/en/, accessed 16 August 2018.
- World Health Assembly Resolution WHA71.1. Thirteenth General Programme of Work, 2019–2023. Geneva: World Health Organization, 2018. Available online: http://apps.who.int/gb/ebwha/pdf_files/WHA71/A71_R1-en.pdf, accessed 16 August 2018.
- World Health Organization. Time to deliver: report of the WHO Independent high-level commission on noncommunicable diseases. World Health Organization, 2018. Available online: http://www.who.int/iris/handle/10665/272710, License: CC BY-NC-SA 3.0 IGO
- Noncommunicable Diseases Progress Monitor 2017. World Health Organization 2017. 231, Geneva, Switzerland.
- Masquelier B, Hug L, Sharrow D, et al. Global, regional, and national mortality trends in older children and young adolescents (5-14 years) from 1990 to 2016: an analysis of empirical data. The Lancet Global Health, 2018, volume 6.issue 10,PE1087-E1099, October 01. DOI: https://doi.org/ [Crossref]
- Spoon DB, Psaltis PJ, Singh M, et al. Trends in cause of death after percutaneous coronary intervention. Circulation 2014;129:1286-94. [Crossref] [PubMed]
- Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016. Geneva: World Health Organization; 2018. Available online: http://www.who.int/healthinfo/global_burden_disease/estimates/en/
- Khaltaev N. GARD, a new way to battle with chronic respiratory diseases, from disease oriented programmes to global partnership. J Thorac Dis 2017;9:4676-89. [Crossref] [PubMed]
- Global status report on noncommunicable diseases 2010. Geneva: World Health Organization, 2011.
- Tackling NCDs “Best buys” and other recommended interventions for the prevention and control of noncommunicable diseases. World Health Organization; 2017. Geneva, Switzerland. Available online: http://www.who.int/ncds/management/best-buys/en/, Accessed 16 August 2018.
- Saving lives, spending less: a strategic response to noncommunicable diseases. Geneva: World Health Organization, 2018. Available online: http://www.who.int/ncds/management/ncds-strategic-response/en/, accessed 16 August 2018.
- Global status report on alcohol and health 2018. Geneva: World Health Organization, 2018.
- Khaltaev N. WHO Dietary Recommendations and Prevention of Chronic Respiratory Diseases. J Obes Nutr Disord 2018;100025. [Crossref]
- New country classifications by income level: 2018-2019. Available online: https://blogs.worldbank.org
- Erhola M. Reconsideration of PAL-like activities. Available online: presentations. 12th GARD General Meeting, 31 August 2018. Helsinki, Finland.https://gard-breathefreely.org/ppt2018, /PowerPoint
- Global Initiative for Chronic Obstructive Lung Disease-2019 GOLD Report. Available online: https://goldcopd.org/gold-reports/
- The Global Asthma Report 2018. Auckland, New Zealand: Global Asthma Network, 2018, 88pp. Available online: www.globalasthmanetwork.org
- Pistelli R, Forastiere F, Corbo GM, et al. Respiratory symptoms and bronchial responsiveness are related to dietary salt intake and urinary potassium excretion in male children. EurRespir J 1993;6:517-22. [PubMed]
- Corbo GM, Forastiere F, De Sario M, et al. SIDRIA-2 Collaborative Group. Wheeze and asthma in children: association with body mass index, sports, television viewing, and diet. Epidemiology 2008;19:747-55. [Crossref] [PubMed]
- Ardern KD. Dietary salt reduction or exclusion for allergic asthma. Cochrane Database Syst Rev 2004.CD000436. [PubMed]
- Gotshall R, Mickleborough T, Cordain L. Dietary salt restriction improves pulmonary function in exercise - induced asthma. Med Sci Sports Exerc 2000;32:1815-9. [Crossref] [PubMed]
- Katan MB. Trans fatty acids and plasma lipoproteins. Nutrition Reviews 2000;58:188-91. [Crossref] [PubMed]
- Oomen CM, Ocké MC, Feskens EJ, et al. Association between trans fatty acid intake and 10- year risk of coronary heart disease in the Zutphen Elderly Study: a prospective population-based study. Lancet 2001;357:746-51. [Crossref] [PubMed]
- Mozaffarian D, Katan MB, Ascherio A, et al. Trans fatty acids and cardiovascular disease. NEJM 2006;354:1601-13. [Crossref] [PubMed]
- Harris WS, Pottala JV, Vasan RS, et al. Changes in erythrocyte membrane trans and marine fatty acids between 1999 and 2006 in older Americans. J Nutr 2012;142:1297-303. [Crossref] [PubMed]
- Weiland SK, Vonmutius E, Husing A, et al. Intake of trans fatty acids and prevalence of childhood asthma and allergies in Europe. Lancet 1999;353:2040-1. [Crossref] [PubMed]
- Wijga AH, Houwelingen AC, Smit HA, et al. Fatty acids in breast milk of allergic and non-allergic mothers: The PIAMA birth cohort study. Pediatr Allergy Immunol 2003;14:156-62. [Crossref] [PubMed]
- Wijga AH, Smit HA, Kerkhof M, et al. Association of consumption of products containing milk fat with reduced asthma risk in pre - school children: in PIAMA birth cohort study. Thorax 2003;58:567-72. [Crossref] [PubMed]
- Varraso R, Fung TT, Barr RG, et al. Prospective study of dietary patterns and chronic obstructive pulmonary disease among US women. Am Clin Nutr 2007;86:488-95. [Crossref] [PubMed]
- Varraso R, Fung TT, Hu FB, et al. Prospective study of dietary patterns and chronic obstructive pulmonary disease among US men. Thorax 2007;62:786-91. [Crossref] [PubMed]
- Global recommendations on physical activity for health. Geneva: World Health Organization; 2010. Available online: http://www.who.int/dietphysicalactivity/publications/9789241599979/en/, accessed 16 August 2018.
- Global action plan on physical activity 2018–2030: more active people for a healthier world. Geneva: World Health Organization, 2018. Available online: http://www.who.int/ncds/prevention/physical-activity/global-action-plan-2018-2030/en/, accessed 16 August 2018.
- Guthold R, Stevens GA, Riley LM, et al. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health 2018;6:e1077-e1086. [Crossref] [PubMed]
- Pitta F, Troosters T, Spruit MA, et al. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2005;171:972-7. [Crossref] [PubMed]
- Mantoani LC, Rubio N, McKinstry B, et al. Interventions to modify physical activity in patients with COPD: a systematic review. Eur Respir J 2016;48:69-81. [Crossref] [PubMed]
- Obesity: preventing and managing the global epidemic. Report of a WHO Consultation, 2000. Technical Report Series 894 World Health Organization, Geneva, Switzerland.
- Ford ES. The epidemiology of obesity and asthma. J Allergy Clin Immunol 2005;115:897-909. [Crossref] [PubMed]
- Bergeron C, Boulet LP, Hamid Q. Obesity, allergy and immunology. J Allergy Clin Immunol 2005;115:1102-4. [Crossref] [PubMed]
- Hallstrand TS, Fishwe ME, Wurfel MM, et al. Genetic pleiotropy between asthma and obesity in community- based sample of twins. J Allergy Clin Immunol 2005;116:1235-41. [Crossref] [PubMed]
- Braback L, Hjern A, Rasmussen F. Body mass index, asthma and allergic rhinoconjunctivitis in Swedish conscripts - a national cohort study over three decades. Respir Med 2005;99:1010-4. [Crossref] [PubMed]
- Kim S, Camargo CA Jr. Sex - race differences in the relationship between obesity and asthma; the behavioral risk factor surveillance system, 2000. Ann Epidemiol 2003;13:666-73. [Crossref] [PubMed]
- Perez-Padilla R, Rojas R, Torres V, et al. Obesity among Children Residing in Mexico City and its impact on Lung Function: A Comparison with Mexican-Americans. Arch Med Res 2006;37:165-71. [Crossref] [PubMed]
- Wickens K, Barry D, Friezema A, et al. Fast foods- are they a risk factor for asthma? Allergy 2005;60:1537-41. [Crossref] [PubMed]
- Sin DD, Jones RL, Man SF. Obesity is a risk factor for dyspnoea but not for airflow obstruction. Arch Intern Med 2002;162:1477-81. [Crossref] [PubMed]
- Saint-Pierre P, Bourdin A, Chanez P, et al. Are overweight asthmatics more difficult to control? Allergy 2006;61:79-84. [PubMed]
- Watson L, Vonk JM, Lofdahl CG, et al. Predictors of lung function and its decline in mild to moderate COPD in association with gender: Results from the EUROSCOP study. Respir Med 2006;100:746-53. [Crossref] [PubMed]
- WHO. Air Pollution. World Health Organization 2019. Available online: https://www.who.int
- Eisner MD, Anthonisen N, Coultas D, et al. An official American Thoracic Society public policy statement: Novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2010;182:693-718. [Crossref] [PubMed]
- Paulin LM, Diette GB, Blanc PD, et al. Occupational exposures are associated with worse morbidity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2015;191:557-65. [Crossref] [PubMed]
- Gan WQ, FitzGerald JM, Carlsten C, et al. Associations of ambient air pollution with chronic obstructive pulmonary disease hospitalization and mortality. Am J Respir Crit Care Med 2013;187:721-7. [Crossref] [PubMed]
- Sana A, Somda SMA, Meda N, Bouland C. Chronic obstructive pulmonary disease associated with biomass fuel use in women: a systematic review and meta-analysis. BMJ Open Respir Res 2018;5:e000246. [Crossref] [PubMed]


