Published online Nov 26, 2018. doi: 10.12998/wjcc.v6.i14.847
Peer-review started: May 29, 2018
First decision: July 8, 2018
Revised: July 20, 2018
Accepted: October 22, 2018
Article in press: October 22, 2018
Published online: November 26, 2018
Heterotopic pancreas (HP) is a congenital anomaly defined as pancreatic tissue that has no contact with the orthotopic pancreas and its own duct system and vascular supply. The most common locations of HP are the upper gastrointestinal tract, specifically, the stomach, duodenum, and proximal jejunum. Involvement of the mesentery is rare. Here, we describe a rare case of mesenteric heterotopic pancreas (MHP) in a 12-year-old girl who presented with acute abdomen. The patient underwent emergency laparotomy, and the mass and adjacent small bowel were resected. Results of the postoperative histopathologic examination confirmed the diagnosis of MHP. Observation of the patient for 12 mo postoperatively showed no evidence of recurrence. Preoperative diagnosis of HP is difficult, even in a symptomatic patient. Increased awareness and understanding of the image characteristics of MHP will aid in correct preoperative diagnosis and appropriate patient management.
Core tip: Heterotopic pancreas (HP) is a congenital anomaly defined as pancreatic tissue that has no contact with the orthotopic pancreas and its own duct system and vascular supply. The most common locations of HP are the upper gastrointestinal tract, specifically, the stomach, duodenum, and proximal jejunum. Involvement of the mesentery is rare. Here, we describe a rare case of mesenteric heterotopic pancreas (MHP) in a 12-year-old girl who presented with acute abdomen. MHP should be considered in the differential diagnosis of a mesenteric mass, especially when its morphology and enhancement are similar to those of orthotopic pancreas.
- Citation: Tang XB, Liao MY, Wang WL, Bai YZ. Mesenteric heterotopic pancreas in a pediatric patient: A case report and review of literature. World J Clin Cases 2018; 6(14): 847-853
- URL: https://www.wjgnet.com/2307-8960/full/v6/i14/847.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i14.847
Heterotopic pancreas (HP) is most commonly found in the proximal gastrointestinal tract. Although the reported incidence of HP varies, the true incidence is difficult to determine because the patients are usually asymptomatic and the condition is usually found incidentally at autopsy or during laparotomy[1,2]. Male preponderance is seen among adults, with the incidence of disease peaking during the fourth to sixth decades of life[3,4]. The most frequent location of heterotopic pancreatic tissue is the stomach (47%), followed by the jejunum (35%), duodenum (11.7%), and ileum (5.8%)[5]. Involvement of the mesentery is rare. Until now, no more than ten cases of mesenteric heterotopic pancreas (MHP) have been described in the medical literature[6-13]. Here, we describe a case of MHP in a 12-year-old female patient.
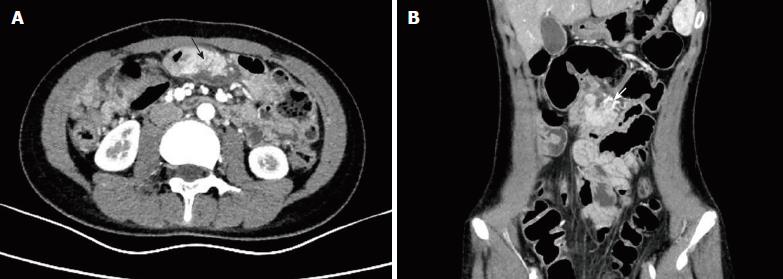
A 12-year-old girl with no significant medical history was admitted to our department with intermittent vomiting and abdominal pain for 3 d. Her growth and development were normal. On admission, she was in a good general condition. Her temperature was 36.6 °C, heart rate was 106 beats/min, and the blood pressure was 100/69 mmHg. Her physical examination showed abdominal tenderness with peritoneal irritation. The laboratory results were unremarkable. Abdominal ultrasonography revealed a well-defined, heterogeneous, medially echoic mass located at the margin of the intestinal mesentery in the abdominal cavity that measured approximately 4.9 cm × 2.6 cm. Contrast-enhanced computed tomography (CECT) of the abdomen showed an enhanced oval, soft-tissue mass (42 mm × 25 mm) in the mesentery at the level of the umbilicus (Figure 1). The clinical diagnosis of a mesenteric mass was made. The differential diagnosis included intestinal duplication cyst, inflammated Meckel’s diverticulum, and mesenteric lymphangioma.
Because of peritoneal irritation, the patient underwent emergency laparotomy 12 h after hospitalization. Laparotomy revealed a yellowish, soft-tissue mass measuring 4 cm in diameter that was located in the mesentery of the proximal jejunum and adhered to the serosal surface of the jejunum (Figure 2). The mass and the adjacent jejunum were resected, and an end-to-end anastomosis was performed.
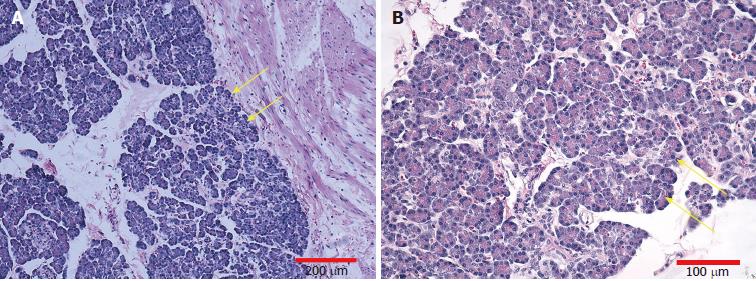
Gross pathology demonstrated a 4 cm × 3 cm mass in the jejunal mesentery that was adhered to the serosa of the jejunum. Postoperative histopathologic examination of the resected specimen revealed ectopic pancreatic tissue consisting of acini, islet cells, and pancreatic ducts, adjacent to the jejunal serosa (Figure 3). There was no evidence of malignant change in the ectopic pancreatic tissue. The pathologic diagnosis was MHP.
The patient’s postoperative course was uneventful, and she was discharged on postoperative day 8. Follow-up of the patient by abdominal ultrasonography for 12 mo postoperatively showed no evidence of relapse.
HP was first described by Jean Schultz in 1727, which is a congenital anomaly defined as pancreatic tissue that is anatomically separate from the main gland, without vascular or ductal continuity. No more than ten cases of MHP have been described in the medical literature[6-12]. Including our case, only four cases of pediatric MHP have been reported in the medical literature[6,7,9], with patients ranging in age from 12 to 15 years.
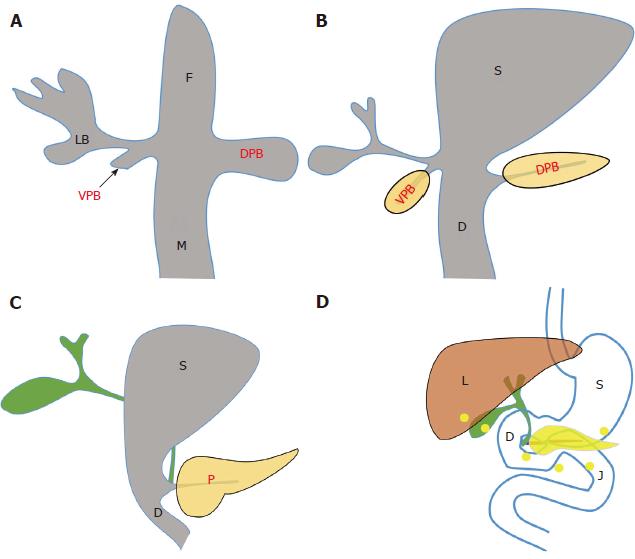
The embryologic basis of HP is controversial, but the most widely held theory is the misplacement theory (Figure 4), according to which, deposits of pancreatic tissue are “dropped” into the developing gastrointestinal system, in anatomic isolation from the main body of the pancreas[11,13]. This theory accounts for the fact that heterotopic pancreatic tissue was mostly located in the upper gastrointestinal tract near the pancreas (derivatives of the primitive foregut).
HP is well differentiated and cannot be distinguished histologically from orthotopic pancreas[1]. Gross specimens always show a firm intramural mass that has a lobular shape and a well-defined interface with surrounding tissues[14]. Most lesions (80%) are solitary and smaller than 3 cm, but they can range in size from 0.2 cm to 5.0 cm[14,15]. The first and most common histological type of heterotopic pancreatic tissue is composed of all the elements of the normal pancreas, including the acini, ducts, and islet cells[16]. However, not all three of these components were identified in a single case. The morphologic feature of MHP closely resembles that of the orthotopic pancreas and manifests as a homogeneous, well-enhanced, and elongated mass with pancreas-like clefts or lobulations[17].
Uncomplicated HP is typically asymptomatic, which is always discovered incidentally during surgery, imaging examination, or autopsy. Any complication that can occur in the orthotopic pancreas can also occur in HP. Associated complications include pancreatitis, pseudocyst formation, abnormal hormone secretion, bowel obstruction, common bile duct obstruction, gastrointestinal bleeding, intussusception, and malignant degeneration[3,4,18-20]. Depending on its location and size, and involvement of the overlying mucosa, HP can cause symptoms. The most common findings were abdominal pain, abdominal distension, nausea and vomiting, malaise, anorexia, anemia, body weight loss, jaundice, and upper gastrointestinal bleeding according to the study by Zhang et al[1].
Because of its rarity and nonspecific clinical manifestation, accurate preoperative diagnosis of HP remains difficult[5,21]. The definitive diagnosis has been always achieved after postoperative pathology. CECT and magnetic resonance imaging (MRI) may demonstrate the lesion that enhances similarly to the orthotopic pancreas[22-26]. The most common CT manifestation of HP is a small intramural and endoluminal mass with microlobulated margins[22]. On an MRI scan, HP is isointense to the orthotopic pancreas, with characteristic T1-weighted high signal intensity and early avid enhancement after the administration of intravenous contrast material[17,22], which is particularly helpful for differentiating HP from other lesions. Heterotopic pancreatic tissue has a rudimentary ductal system. The existence of a central duct along the long axis of the mass is another key finding for the diagnosis of HP[8,17,22]. Sometimes the duct can be confirmed as draining into the fourth portion of the duodenum by magnetic resonance cholangiopancreatography[8]. Knowledge of the characteristic imaging appearance of MHP is key to confirming the diagnosis preoperatively. First, as with HP in other locations, MHP has morphologic and enhancement characteristics similar to the orthotopic pancreas, named “another pancreas in the mesentery”[17,22]. Second, the mean long axis diameter/short axis diameter ratio of MHP was much greater than that of gastric HP (3.0 vs 1.4-1.5)[17]. Third, a duct-like structure paralleling the long axis of MHP is seen more frequently than HP in other locations[17].
MHP should be considered in the differential diagnosis. A gastrointestinal stromal tumor, carcinoid tumor, lymphoma, and metastasis can manifest as a homogeneous and well-enhanced soft tissue mass located in the mesentery, and the enhancement pattern is unreliable to differentiate from MHP on an enhanced CT scan[17]. Because of the potential serious complications and malignant change, local excision of MHP is the optimal treatment[2,26].
We list the cases of MHP in medical literature (Table 1) and found some characteristics of MHP. First, MHP was not seen in children younger than 10 years old. Of the eight cases of MHP, 50% (4/8) were teenagers aged from 12 to 15 years old, 50% (4/8) were adults aged from 38 to 75 years old. Second, there is a female preponderance (75%, 6/8) of MHP, which is opposite to the male preponderance of HP. Third, the majority of MHP (75%, 6/8) were located in jejunal mesentery. Fourth, CECT and MRCP were the most useful diagnostic method for MHP. These characteristics can be applied in clinical diagnosis of MHP.
| Ref. | Age (yr) | Sex | Clinical manifestation | Location | Imaging features | Operation |
| [6] | 15 | F | Right upper quadrant pain; Diffuse abdominal tenderness, most pronounced in the right upper quadrant and nonspecific guarding | Jejunal mesentery | CECT: A 3.3 cm × 2.3 cm soft tissue mass in the mesentery, with morphology and homogeneous enhancement characteristics similar to the pancreas | A 3 cm mass in the jejunal mesentery, adjacent to the transverse colon and omentum |
| The mass and the adjacent small bowel were resected | ||||||
| [7] | 12 | M | Periumbilical abdominal pain, nausea and vomiting; Temperature of 100 °F | Jejunal mesentery | No imaging examination | A purulent node (1.5 cm × 1 cm × 0.7 cm) with fibrinous exudate at the base of the midjejunal mesentary |
| A rigid abdomen with absence of bowel sounds | This node was excised | |||||
| [8] | 57 | F | Pain in the right side of the back, nausea, a similar episode of pain approximately 1 mo before Mild, generalized abdominal tenderness and nonspecific guarding | Small bowel mesentery | CECT: A 3.7 cm × 1.7 cm soft tissue mass in the mesentery, enhancement similar to the pancreas | Treated conservatively |
| MRCP: A duct within the mesenteric mass, draining into the fourth portion of the duodenum | ||||||
| [9] | 15 | F | Abdominal pain of recent onset and abdominal distention of several years of duration | Mesocolon | CT: A hypodense, intraperitoneal, circumscribed mass dislocating the spleen and left kidney | A spherical, encapsulated tumor mass (210 mm in the largest diameter) in the mesocolon Resection of the mass with a segment of transverse colon |
| A large tumor filling the left hypochondrium | ||||||
| [10] | 75 | F | Acute periumbilical pain, nausea and vomiting | Jejunal mesentery | US: Cholelithiasis and gallbladder wall thickening | An inflammatory mass in the mesentery, 15 cm × 8 cm × 5 cm |
| Acute abdomen with peritoneal irritation findings | US before the surgery: An abdominal tumoral mass, pseudokidney image, originating from the intestine or mesentery | A great portion of the inflammatory mass was excised, and cholecystectomy | ||||
| [11] | 38 | M | One episode of syncope, 2-d history of melena | Jejunal mesentery | CECT: An elongated soft tissue mass in the jejunal mesentery, attenuation similar to orthotopic pancreas and extended to the periduodenal fat plane | A soft-tissue mass 20 cm in diameter in the jejunal mesentery, infiltrating the adjacent jejunal wall |
| The heart rate was 96 beats/min; no abdominal tenderness | The lesion was excised with part of the adjacent jejunum | |||||
| [12] | 67 | F | Postprandial epigastric stabbing pain, nausea and vomiting. Similar episodes had recurred over the past 30 yr | Jejunal mesentery | CECT: A mass in the mesentery. A small ductal structure in the mass, communicating with the adjacent jejunal loop MRCP: A mass in the mesentery isointense to the native pancreas, with a small duct draining into a proximal jejunal loop | A mass (6.5 cm × 2.5 cm × 1.6 cm indurated teardrop-shaped) mass in the jejunal mesentery |
| Past medical history: A laparoscopic cholecystectomy; Tenderness of epigastrium | The mass with the overlying adherent jejunum was resected | |||||
| This study | 12 | F | Intermittent vomiting and abdominal pain | Jejunal mesentery | US: A well-defined, heterogeneous, medially echoic, 4.9 cm × 2.6 cm mass at the margin of the mesentery | A yellowish, soft-tissue mass 4 cm in diameter in the mesentery, adhered to the serosa of the jejunum |
| Abdominal tenderness with peritoneal irritation | ||||||
| CECT: An enhanced oval, soft tissue mass (42 cm × 25 mm) in the mesentery | The mass and the adjacent small bowel were resected |
In conclusion, MHP is very rare and an unusual cause of acute abdomen in patients older than 12 years. Preoperative diagnosis of MHP is difficult, even in a symptomatic patient. When a mesenteric mass has morphology and enhancement similar to the orthotopic pancreas, MHP should be considered in the differential diagnosis. Increased awareness and understanding of the imaging characteristics of MHP will aid in correct preoperative diagnosis and appropriate patient management.
A 12-year-old girl with intermittent vomiting and abdominal pain for 3 d.
Mesenteric mass.
Intestinal duplication cyst, inflammated Meckel’s diverticulum, and mesenteric lymphangioma were considered.
The laboratory results were unremarkable.
Contrast-enhanced computed tomography (CECT) of the abdomen showed an enhanced oval, soft-tissue mass (42 mm × 25 mm) in the mesentery at the level of the umbilicus.
Mesenteric heterotopic pancreas (MHP).
Resection of the mass and adjacent small bowel.
Two cases of pediatric MHP have been reported in the medical literature from the University of Chicago Medical Center and Boston City Hospital.
Heterotopic pancreas of the mesentery.
This case will contribute to increasing clinicians’ awareness and understanding of the imaging features of MHP in order to help in making correct preoperative diagnosis and giving appropriate treatment.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Amornyotin S, Nobile S, Pandey A, Sergi CM, Shaaban OM, Uwaezuoke SN S- Editor: Ji FF L- Editor: Wang TQ E- Editor: Song H
| 1. | Zhang Y, Sun X, Gold JS, Sun Q, Lv Y, Li Q, Huang Q. Heterotopic pancreas: a clinicopathological study of 184 cases from a single high-volume medical center in China. Hum Pathol. 2016;55:135-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Lai EC, Tompkins RK. Heterotopic pancreas. Review of a 26 year experience. Am J Surg. 1986;151:697-700. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 140] [Cited by in F6Publishing: 123] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Tanaka K, Tsunoda T, Eto T, Yamada M, Tajima Y, Shimogama H, Yamaguchi T, Matsuo S, Izawa K. Diagnosis and management of heterotopic pancreas. Int Surg. 1993;78:32-35. [PubMed] [Cited in This Article: ] |
| 4. | Pang LC. Pancreatic heterotopia: a reappraisal and clinicopathologic analysis of 32 cases. South Med J. 1988;81:1264-1275. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 67] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Hsia CY, Wu CW, Lui WY. Heterotopic pancreas: a difficult diagnosis. J Clin Gastroenterol. 1999;28:144-147. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 86] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Ginsburg M, Ahmed O, Rana KA, Boumendjel R, Dachman AH, Zaritzky M. Ectopic pancreas presenting with pancreatitis and a mesenteric mass. J Pediatr Surg. 2013;48:e29-e32. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Fam S, O’Briain DS, Borger JA. Ectopic pancreas with acute inflammation. J Pediatr Surg. 1982;17:86-87. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Silva AC, Charles JC, Kimery BD, Wood JP, Liu PT. MR Cholangiopancreatography in the detection of symptomatic ectopic pancreatitis in the small-bowel mesentery. AJR Am J Roentgenol. 2006;187:W195-W197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Tornóczky T, Kálmán E, Jáksó P, Méhes G, Pajor L, Kajtár GG, Battyány I, Davidovics S, Sohail M, Krausz T. Solid and papillary epithelial neoplasm arising in heterotopic pancreatic tissue of the mesocolon. J Clin Pathol. 2001;54:241-245. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 46] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Canbaz H, Colak T, Düşmez Apa D, Sezgin O, Aydin S. An unusual cause of acute abdomen: mesenteric heterotopic pancreatitis causing confusion in clinical diagnosis. Turk J Gastroenterol. 2009;20:142-145. [PubMed] [Cited in This Article: ] |
| 11. | Shin SS, Jeong YY, Kang HK. Giant heterotopic pancreas in the jejunal mesentery. AJR Am J Roentgenol. 2007;189:W262-W263. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Wong JC, Robinson C, Jones EC, Harris A, Zwirewich C, Wakefield R, Simons RK, Yoshida EM. Recurrent ectopic pancreatitis of the jejunum and mesentery over a 30-year period. Hepatobiliary Pancreat Dis Int. 2011;10:218-220. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Kim DW, Kim JH, Park SH, Lee JS, Hong SM, Kim M, Ha HK. Heterotopic pancreas of the jejunum: associations between CT and pathology features. Abdom Imaging. 2015;40:38-45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Park SH, Han JK, Choi BI, Kim M, Kim YI, Yeon KM, Han MC. Heterotopic pancreas of the stomach: CT findings correlated with pathologic findings in six patients. Abdom Imaging. 2000;25:119-123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Mortelé KJ, Rocha TC, Streeter JL, Taylor AJ. Multimodality imaging of pancreatic and biliary congenital anomalies. Radiographics. 2006;26:715-731. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 206] [Cited by in F6Publishing: 225] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 16. | Trifan A, Târcoveanu E, Danciu M, Huţanaşu C, Cojocariu C, Stanciu C. Gastric heterotopic pancreas: an unusual case and review of the literature. J Gastrointestin Liver Dis. 2012;21:209-212. [PubMed] [Cited in This Article: ] |
| 17. | Seo N, Kim JH. Characteristic CT features of heterotopic pancreas of the mesentery: “another pancreas” in the mesentery. Clin Imaging. 2014;38:27-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Makhlouf HR, Almeida JL, Sobin LH. Carcinoma in jejunal pancreatic heterotopia. Arch Pathol Lab Med. 1999;123:707-711. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 19. | Halkic N, Nordback P. Soft-tissue images. Malignant degeneration of heterotopic pancreas. Can J Surg. 2001;44:407. [PubMed] [Cited in This Article: ] |
| 20. | Riccardo G, Valeria B, Giulia C, Alessia C, Luisa F, Elisabetta T, Alessandro M, Isabella M, Jürgen S. Heterotopic pancreas in Meckel’s diverticulum in a 7-year-old child with intussusception and recurrent gastrointestinal bleeding: case report and literature review focusing on diagnostic controversies. Afr J Paediatr Surg. 2014;11:354-358. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Ogata H, Oshio T, Ishibashi H, Takano S, Yagi M. Heterotopic pancreas in children: review of the literature and report of 12 cases. Pediatr Surg Int. 2008;24:271-275. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Rezvani M, Menias C, Sandrasegaran K, Olpin JD, Elsayes KM, Shaaban AM. Heterotopic Pancreas: Histopathologic Features, Imaging Findings, and Complications. Radiographics. 2017;37:484-499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 87] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 23. | Cho JS, Shin KS, Kwon ST, Kim JW, Song CJ, Noh SM, Kang DY, Kim HY, Kang HK. Heterotopic pancreas in the stomach: CT findings. Radiology. 2000;217:139-144. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 78] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 24. | Megibow AJ, Balthazar EJ, Cho KC, Medwid SW, Birnbaum BA, Noz ME. Bowel obstruction: evaluation with CT. Radiology. 1991;180:313-318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 191] [Cited by in F6Publishing: 161] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 25. | Wang C, Kuo Y, Yeung K, Wu C, Liu G. CT appearance of ectopic pancreas: a case report. Abdom Imaging. 1998;23:332-333. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |