Abstract
Background
The impact of primary tumor location on overall survival (OS), recurrence-free survival (RFS), and long-term outcomes has not been well established in patients undergoing potentially curative resection of colorectal liver metastases (CRLM).
Methods
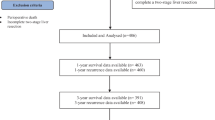
A single-institution database was queried for initial resections for CRLM 1992–2004. Primary tumor location determined by chart review (right = cecum to transverse; left = splenic flexure to sigmoid). Rectal cancer (distal 16 cm), multiple primaries, and unknown location were excluded. Kaplan–Meier and Cox regression methods were used. Cure was defined as actual 10-year survival with either no recurrence or resected recurrence with at least 3 years of disease-free follow-up.
Results
A total of 907 patients were included with a median follow-up of 11 years; 578 patients (64%) had left-sided and 329 (36%) right-sided primaries. Median OS for patients with a left-sided primary was 5.2 years (95% confidence interval [CI] 4.6–6.0) versus 3.6 years (95% CI 3.2–4.2) for right-sided (p = 0.004). On multivariable analysis, the hazard ratio for right-sided tumors was 1.22 (95% CI 1.02–1.45, p = 0.028) after adjusting for common clinicopathologic factors. Median RFS was marginally different stratified by primary location (1.3 vs. 1.7 years; p = 0.065). On multivariable analysis, location of primary was not significantly associated with RFS (p = 0.105). Observed cure rates were 22% for left-sided and 20% for right-sided tumors.
Conclusions
Among patients undergoing resection of CRLM, left-sided primary tumors were associated with improved median OS. However, long-term survival and recurrence-free survival were not significantly different stratified by primary location. Patients with left-sided primary tumors displayed a prolonged clinical course suggestive of more indolent biology.


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29.
Benedix F, Kube R, Meyer F, et al. Comparison of 17,641 patients with right- and left-sided colon cancer: differences in epidemiology, perioperative course, histology, and survival. Dis Colon Rectum. 2010;53:57–64.
Weiss JM, Pfau PR, O’Connor ES, et al. Mortality by stage for right- versus left-sided colon cancer: analysis of surveillance, epidemiology, and end results–Medicare data. J Clin Oncol. 2011;29:4401–9.
Yahagi M, Okabayashi K, Hasegawa H, et al. The worse prognosis of right-sided compared with left-sided colon cancers: a systematic review and meta-analysis. J Gastrointest Surg. 2016;20:648–55.
Gervaz P, Bucher P, Morel P. Two colons-two cancers: paradigm shift and clinical implications. J Surg Oncol. 2004;88:261–6.
Benedix F, Meyer F, Kube R, et al. Influence of anatomical subsite on the incidence of microsatellite instability, and KRAS and BRAF mutation rates in patients with colon carcinoma. Pathol Res Pract. 2012;208:592–7.
Bufill JA. Colorectal cancer: evidence for distinct genetic categories based on proximal or distal tumor location. Ann Intern Med. 1990;113:779–88.
Price TJ, Beeke C, Ullah S, et al. Does the primary site of colorectal cancer impact outcomes for patients with metastatic disease? Cancer. 2015;121:830–5.
Tejpar S, Stintzing S, Ciardiello F, et al. Prognostic and predictive relevance of primary tumor location in patients with RAS wild-type metastatic colorectal cancer: retrospective analyses of the CRYSTAL and FIRE-3 Trials. JAMA Oncol. 2016;3:194–201.
Venook A, Niedzwiecki D, Innocenti F, et al. Impact of primary (1º) tumor location on overall survival (OS) and progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC): analysis of CALGB/SWOG 80405 (Alliance). J Clin Oncol. 2016;34:3504.
Holch JW, Ricard I, Stintzing S, et al. The relevance of primary tumour location in patients with metastatic colorectal cancer: a meta-analysis of first-line clinical trials. Eur J Cancer. 2016;70:87–98.
Tomlinson JS, Jarnagin WR, DeMatteo RP, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol. 2007;25:4575–80.
Pulitano C, Castillo F, Aldrighetti L, et al. What defines ‘cure’ after liver resection for colorectal metastases? Results after 10 years of follow-up. HPB (Oxford). 2010;12:244–9.
Vigano L, Ferrero A, Lo Tesoriere R, et al. Liver surgery for colorectal metastases: results after 10 years of follow-up. Long-term survivors, late recurrences, and prognostic role of morbidity. Ann Surg Oncol. 2008;15:2458–64.
Fong Y, Fortner J, Sun RL, et al. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230:309–18; discussion 318–21.
Zakaria S, Donohue JH, Que FG, et al. Hepatic resection for colorectal metastases: value for risk scoring systems? Ann Surg. 2007;246:183–91.
Nordlinger B, Guiguet M, Vaillant JC, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996;77:1254–62.
Cardona K, Mastrodomenico P, D’Amico F, et al. Detailed pathologic characteristics of the primary colorectal tumor independently predict outcome after hepatectomy for metastases. Ann Surg Oncol. 2013;20:148–54.
Sasaki K, Andreatos N, Margonis GA, et al. The prognostic implications of primary colorectal tumor location on recurrence and overall survival in patients undergoing resection for colorectal liver metastasis. J Surg Oncol. 2016;114:803–9.
Yamashita S, Brudvik KW, Kopetz SE, et al. Embryonic origin of primary colon cancer predicts pathologic response and survival in patients undergoing resection for colon cancer liver metastases. Ann Surg. 2016. https://doi.org/10.1097/SLA.0000000000002087.
Sadot E, Groot Koerkamp B, Leal JN, et al. Resection margin and survival in 2368 patients undergoing hepatic resection for metastatic colorectal cancer: surgical technique or biologic surrogate? Ann Surg. 2015;262:476–85; discussion 483–5.
Carpizo DR, Are C, Jarnagin W, et al. Liver resection for metastatic colorectal cancer in patients with concurrent extrahepatic disease: results in 127 patients treated at a single center. Ann Surg Oncol. 2009;16:2138–46.
Missiaglia E, Jacobs B, D’Ario G, et al. Distal and proximal colon cancers differ in terms of molecular, pathological, and clinical features. Ann Oncol. 2014;25:1995–2001.
Schirripa M, Bergamo F, Cremolini C, et al. BRAF and RAS mutations as prognostic factors in metastatic colorectal cancer patients undergoing liver resection. Br J Cancer. 2015;112:1921–8.
Karagkounis G, Torbenson MS, Daniel HD, et al. Incidence and prognostic impact of KRAS and BRAF mutation in patients undergoing liver surgery for colorectal metastases. Cancer. 2013;119:4137–44.
Nash GM, Gimbel M, Cohen AM, et al. KRAS mutation and microsatellite instability: two genetic markers of early tumor development that influence the prognosis of colorectal cancer. Ann Surg Oncol. 2010;17:416–24.
Kemeny N, Huang Y, Cohen AM, et al. Hepatic arterial infusion of chemotherapy after resection of hepatic metastases from colorectal cancer. N Engl J Med. 1999;341:2039–48.
Acknowledgement
Supported in part by the Biostatistics Core and NIH/NCI P30 CA008748 Cancer Center Support Grant.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Creasy, J.M., Sadot, E., Koerkamp, B.G. et al. The Impact of Primary Tumor Location on Long-Term Survival in Patients Undergoing Hepatic Resection for Metastatic Colon Cancer. Ann Surg Oncol 25, 431–438 (2018). https://doi.org/10.1245/s10434-017-6264-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6264-x