Abstract
Purpose
The type of surgery and the extent of lymphadenectomy depend on the tumor location and should be based on the extent of lymphatic spread and the oncologic outcome. The aim was to analyze patterns of lymph node metastasis in patients with right-sided colon cancer.
Methods
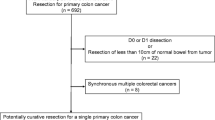
Between 1996 and 2007, a total of 419 patients underwent curative resection for right-sided colon cancer. Lymph nodes were grouped immediately after surgery on the basis of the location of the tumor.
Results
There were 75, 208, 78, and 58 tumors in the cecum, ascending colon, at the hepatic flexure, and in the transverse colon, respectively. Of the 58 patients with transverse colon tumors, 43, 11, 3, and 1 underwent right hemicolectomies, transverse colectomies, left hemicolectomies, and a subtotal colectomy, respectively. Patients with cecal and ascending colon cancers most frequently had metastases in the ileocolic lymph nodes. Metastasis to the lymph nodes along the right branch of the middle colic artery occurred in 6.1% of patients with cecal cancer. In patients with hepatic flexure cancers, the epicolic lymph nodes along the right and middle colic arteries were most commonly metastatic lymph nodes. In transverse colon cancer, the middle colic node was the most commonly involved lymph node. Approximately 10% of patients had metastases to the right colic nodes.
Conclusions
Metastasis to lymph nodes along the right colic artery occurred in approximately 10% of the patients with transverse cancer, indicating the need for great care in deciding the extent of segmental resection for these patients.




Similar content being viewed by others
References
Corman ML. Colon and Rectal Surgery. 5th ed. Philadelphia: Lippincott Williams and Wilkins, 2005.
Lee YS, Lee IK, Kang WK, et al. Surgical and pathological outcomes of laparoscopic surgery for transverse colon cancer. Int J Colorectal Dis. 2008;23:669–73.
Schlachta CM, Mamazza J, Poulin EC. Are transverse colon cancers suitable for laparoscopic resection? Surg Endosc. 2007;21:396–9.
Lee YS, Lee IK, Kim HJ, et al. Short-term clinico-pathological outcomes of laparoscopic transverse colectomy for transverse colon cancer. J Korean Soc Coloproctol. 2008;24:107–12.
Japanese Society for Cancer of the Colon and Rectum. Japanese Classification of Colorectal Carcinoma. Tokyo: Kanehara, 1999.
Choi GS, Jun SH. Laparoscopic assisted right hemicolectomy: based on vascular. J Korean Soc Coloproctol. 1997;13:565–72.
Yada H, Sawai K, Taniguchi H, et al. Analysis of vascular anatomy and lymph node metastases warrants radical segmental bowel resection for colon cancer. World J Surg. 1997;21:109–15.
Wood TE, Spirt M, Rangel D, et al. Lymphatic mapping improves staging during laparoscopic colectomy for cancer. Surg Endosc. 2005;15:715–9.
Morton DL, Wen DR, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg. 1992;127: 392–9.
Wood TF, Tsioulias GJ, Morton DL, et al. Focused examination of sentinel lymph nodes upstages early colorectal carcinoma. Am Surg. 2000;66:998–1003.
Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050–9.
Chew SSB, Adams WJ. Laparoscopic hand-assisted extended right hemicolectomy for cancer management. Surg Endosc. 2007;21:1654–6.
International Union Against Cancer (UICC). Colon and rectum. In: Sobin LH, Wittekind CH, eds. TNM Classification of Malignant Tumours. 6th ed. New York: Wiley, 2002.
American Joint Committee on Cancer. AJCC Cancer Staging Manual. 6th ed. Philadelphia: Lippincott-Raven, 2001.
Suzuki O, Sekishita Y, Shiono T, et al. Number of lymph node metastases is better predictor of prognosis than level of lymph node metastasis in patients with node-positive colon cancer. J Am Coll Surg. 2006;2025:732–6.
Kobayashi H, Ueno H, Hashiguchi Y, Mochizuki H. Distribution of lymph node metastasis is a prognostic index in patients with stage III colon cancer. Surgery 2006;139:516–22.
Berger AC, Sigurdson ER, LeVoyer T, et al. Colon cancer survival is associated with decreasing ratio of metastatic examined lymph nodes. J Clin Oncol. 2005;23:8706–12.
Lee HY, Choi HJ, Park KJ, et al. Prognostic significance of metastatic lymph node ratio in node-positive colon carcinoma. Ann Surg Oncol. 2007;14:1712–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, I.J., Choi, GS., Kang, B.M. et al. Lymph Node Metastasis Patterns in Right-Sided Colon Cancers: Is Segmental Resection of These Tumors Oncologically Safe?. Ann Surg Oncol 16, 1501–1506 (2009). https://doi.org/10.1245/s10434-009-0368-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-009-0368-x