Abstract
Background
Few data exist regarding outcomes after resection versus embolic treatment of symptomatic metastatic carcinoid and neuroendocrine tumors. The purpose of this study was to determine whether cytoreduction provides any benefit over embolic management of diffuse neuroendocrine tumors.
Methods
A prospective database of 734 patients treated at our institution was retrospectively queried for symptomatic metastatic tumors treated with embolization or cytoreduction. Patients were compared with regard to pretreatment performance status, relief of symptoms, and survival.
Results
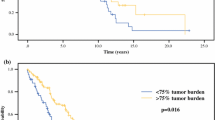
A total of 120 patients were identified: 59 undergoing embolization and 61 undergoing cytoreduction. Twenty-three patients had palliative cytoreduction (gross residual disease). Pretreatment performance status (Eastern Cooperative Oncology Group) was similar for both groups: .7 ± .70 (embolization) versus .8 ± .72 (cytoreduction; P = .27). Complete symptomatic relief was observed in 59% and partial relief in 32% of patients who underwent embolization, with a mean symptom-free interval of 22 ± 13.6 months. A total of 69% of patients who underwent cytoreduction had complete symptomatic relief, and 23% had partial relief (P = .08 vs. embolization). The mean duration of relief was 35 ± 22.0 months (P < .001 vs. embolization). The mean survival for the patients who underwent embolization was 24 ± 15.8 months versus 43 ± 26.1 months for those who underwent cytoreduction (P < .001). Survival in patients who underwent palliative cytoreduction was 32 ± 18.9 months (P < .001 vs. embolization), whereas it was 50 ± 27.6 months in patients who underwent curative resection (P < .001 vs. embolization; P < .001 vs. palliative).
Conclusions
Cytoreduction for metastatic neuroendocrine tumors resulted in improved symptomatic relief and survival when compared with embolic therapy in this nonrandomized study. Cytoreduction should be pursued whenever possible even if complete resection may not be achievable.



Similar content being viewed by others
References
Modlin I, Sandor A. An analysis of 8305 cases of carcinoid tumors. Cancer 1997;79:813–29
Newton J, Swerdlow A, dos Santos Silva I, et al. The epidemiology of carcinoid tumours in England and Scotland. Br J Cancer 1994;70:939–42
Moertel C. Karnofsky memorial lecture. An odyssey in the land of small tumors. J Clin Oncol 1987;5:1502–22
Berge T, Linell F. Carcinoid tumours. Frequency in a defined population during a 12-year period. Acta Pathol Microbiol Scand [A] 1976;84:322–30
Chamberlain R, Canes D, Brown K, et al. Hepatic neuroendocrine metastases: does intervention alter outcomes? J Am Coll Surg 2000;190:432–45
Que F, Nagorney DM, Batts KP, et al. Hepatic resection for metastatic neuroendocrine carcinomas. Am J Surg 1995;169:36–42; discussion 42–3
Crocetti E. Gastrointestinal carcinoid tumours. A population-based study. Ital J Gastroenterol Hepatol 1997;29:135–7
Phan G, Yeo GQ, Hruban RH, et al. Surgical experience with pancreatic and peripancreatic neuroendocrine tumors: review of 125 patients. J Gastrointest Surg 1998;2:472–82
Saltz L, Trochanowski B, Buckely M, et al. Octreotide as an antineoplastic agent in the treatment of functional and nonfunctional neuroendocrine tumors. Cancer 1993;72:244–8
Ruszniewski P, Malka D. Hepatic arterial chemoembolization in the management of advanced digestive endocrine tumors. Digestion 2000;62(Suppl 1):79–83
Fraker D, Soulen M. Regional therapy of hepatic metastases. Hematol Oncol Clin North Am 2002;16:947–67
Sutcliffe R, Maguire D, Ramage J, et al. Management of neuroendocrine liver metastases. Am J Surg 2004;187:39–46
Stephen J, Grahame-Smith DG. Treatment of the carcinoid syndrome by local removal of hepatic metastases. Proc R Soc Med 1972;65:444–5
Strodel W, Talpos G, Eckhauser F, et al. Surgical therapy for small-bowel carcinoid tumors. Arch Surg 1983;118:391–7
Norton J, Sugarbaker PH, Doppman JL, et al. Aggressive resection of metastatic disease in selected patients with malignant gastrinoma. Ann Surg 1986;203:352–9
McEntee G, Nagorney DM, Kvols LK, et al. Cytoreductive hepatic surgery for neuroendocrine tumors. Surgery 1990;108:1091–6
Makridis C, Oberg K, Juhlin C, et al. Surgical treatment of mid-gut carcinoid tumors. World J Surg 1990;14:377–83; discussion 384–5
Soreide O, Berstad T, Bakka A, et al. Surgical treatment as a principle in patients with advanced abdominal carcinoid tumors. Surgery 1992;111:48–54
Grama D, Eriksson B, Martensson H, et al. Clinical characteristics, treatment and survival in patients with pancreatic tumors causing hormonal syndromes. World J Surg 1992;16:632–9
Chen H, Hardacre JM, Uzar A, et al. Isolated liver metastases from neuroendocrine tumors: does resection prolong survival? J Am Coll Surg 1998;187:88–92; discussion 92–3
Thompson GB, Tompkins RK, Longmire WP, et al. Islet cell carcinomas of the pancreas: a twenty-year experience. Surgery 1988;104:1011–7
Ahlman H, Wangberg B, Jansson S, et al. Management of disseminated midgut carcinoid tumours. Digestion 1991;49:78–96
Goto H, Yamaji Y, Konno T, et al. A glucagon-secreting alpha-cell carcinoma of the pancreas. World J Surg 1982;6:107–9
Nagorney DM, Blooms SR, Polak JM, et al. Resolution of recurrent Verner-Morrison syndrome by resection of metastatic vipoma. Surgery 1983;93:348–53
Travis WD, Linnoila RI, Tsokos MG, et al. Neuroendocrine tumors of the lung with proposed criteria for large-cell neuroendocrine carcinoma. An ultrastructural, immunohistochemical, and flow cytometric study of 35 cases. Am J Surg Pathol 1991;15:529–53
Sarmiento JM, Heywood G, Rubin J, et al. Surgical treatment of neuroendocrine metastases to the liver: a plea for resection to increase survival. J Am Coll Surg 2003;197:29–37
Foster JH. Survival after liver resection for cancer. Cancer 1970;26:493-502
Iwatsuki S, Shaw BW, Starzl TE. Experience with 150 liver resections. Ann Surg 1983;197:247–53
Thompson HH, Tompkins RK, Longmire WP. Major hepatic resection. A 25-year experience. Ann Surg 1983;197:375–88
Wolf RF, Goodnight JE, Krag DE, et al. Results of resection and proposed guidelines for patient selection in instances of non-colorectal hepatic metastases. Surg Gynecol Obstet 1991;173:454–60
Ahlman H, Wangberg B, Jansson S, et al. Interventional treatment of gastrointestinal neuroendocrine tumours. Digestion 2000;62(Suppl 1):59–68
Eriksson BK, Larsson EG, Skogseid BM, et al. Liver embolizations of patients with malignant neuroendocrine gastrointestinal tumors. Cancer 1998;83:2293–301
Brown KT, Koh BY, Brody LA, et al. Particle embolization of hepatic neuroendocrine metastases for control of pain and hormonal symptoms. J Vasc Interv Radiol 1999;10:397–403
Lehnert T. Liver transplantation for metastatic neuroendocrine carcinoma: an analysis of 103 patients. Transplantation 1998;66:1307–12
Zimmer T, Stozel U, Bader M, et al. Endoscopic ultrasonography and somatostatin receptor scintigraphy in the preoperative localisation of insulinomas and gastrinomas. Gut 1996;39:562–8
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article is available at http://dx.doi.org/10.1245/ASO.2006.03.902.
Rights and permissions
About this article
Cite this article
Osborne, D.A., Zervos, E.E., Strosberg, J. et al. Improved Outcome With Cytoreduction Versus Embolization for Symptomatic Hepatic Metastases of Carcinoid and Neuroendocrine Tumors. Ann Surg Oncol 13, 572–581 (2006). https://doi.org/10.1245/ASO.2006.03.071
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/ASO.2006.03.071