-
PDF
- Split View
-
Views
-
Cite
Cite
G. Coakley, C. Mathews, M. Field, A. Jones, G. Kingsley, D. Walker, M. Phillips, C. Bradish, A. McLachlan, R. Mohammed, V. Weston, on behalf of the British Society for Rheumatology Standards, Guidelines and Audit Working Group, BSR & BHPR, BOA, RCGP and BSAC guidelines for management of the hot swollen joint in adults, Rheumatology, Volume 45, Issue 8, August 2006, Pages 1039–1041, https://doi.org/10.1093/rheumatology/kel163a
Close - Share Icon Share
Scope and purpose of the guidelines
The clinical presentation of a hot swollen joint is common and has wide differential diagnosis. The most serious is septic arthritis, with a case fatality of 11%. Delayed or inadequate treatment leads to joint damage. These guidelines focus on the diagnosis and management of septic arthritis. Hot swollen joints commonly have other underlying diagnoses, including crystal arthritis, reactive arthritis and a monoarticular presentation of polyarthritis.
Guidelines for managing the hot swollen joint in adults
The guidelines have been developed for use with adults who develop a hot swollen native joint acutely (typically with a history of two weeks or less) affecting any joint except the axial skeleton. This is an abridged version, which is available in full as supplementary material on the journal website.
Symptoms and signs suggestive of septic arthritis
Patients with a short history of a hot, swollen and tender joint (or joints) with restriction of movement should be regarded as having septic arthritis until proven otherwise (B).
If clinical suspicion is high, then it is imperative to treat as septic arthritis even in the absence of fever (B).
Investigation of synovial fluid
The synovial fluid must be aspirated, Gram-stained and cultured prior to starting antibiotics (B). Warfarin does not contraindicate needle aspiration (C).
A possibly infected prosthetic joint should always be referred to an orthopaedic surgeon (C).
Neither the absence of organisms on Gram stain nor a negative subsequent synovial fluid culture excludes the diagnosis of septic arthritis (B).
Specimens must be sent fresh to the laboratory and obtained prior to starting antibiotics (C).
Polarising microscopy should always be carried out (B).
Other laboratory investigations
Blood cultures should always be taken (B).
The white cell count, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) should be measured (B). Inflammatory markers are useful for monitoring response to treatment (B).
The serum urate level is of no diagnostic value in acute gout or sepsis (B).
Electrolytes and liver function should be measured to detect end organ damage because renal function may influence antibiotic choice (B).
If the history suggests non-articular infection, then appropriate cultures and swabs should be taken prior to starting antibiotics (B).
Imaging
Plain radiographs of the affected joint are of no benefit in diagnosing septic arthritis but may show chondrocalcinosis. They should be performed as a baseline investigation (C).
Magnetic resonance imaging is the most appropriate imaging where required, since it is sensitive in detecting osteomyelitis that may require a surgical approach (B).
In suspected hip sepsis, diagnostic aspiration will usually require the use of ultrasound or an image intensifier (C).
Antibiotic treatment of septic arthritis
There is no evidence on which to advise the optimal duration of i.v. or oral antibiotics. Conventionally, they are given intravenously for up to 2 weeks or until signs improve, then orally for 4 weeks. Symptoms, signs and acute phase responses are all helpful in guiding the decision to stop antibiotics. Expert review may be required if the expected resolution does not occur (C).
Summary of recommendations for initial empirical antibiotic choice in suspected septic arthritis
| Patient group . | Antibiotic choice . |
|---|---|
| No risk factors for atypical organisms | Flucloxacillin 2 g qds i.v. Local policy may be to add gentamicin i.v. |
| If penicillin allergic, clindamycin 450–600 mg qds i.v. or 2nd or 3rd generation cephalosporin i.v. | |
| High risk of Gram-negative sepsis (elderly, frail, recurrent UTI, and recent abdominal surgery) | 2nd or 3rd generation cephalosporin eg cefuroxime 1.5 g tds i.v. Local policy may be to add flucloxacillin i.v. to 3rd generation cephalosporin. Discuss allergic patients with microbiology—Gram stain may influence antibiotic choice |
| MRSA risk (known MRSA, recent inpatient, nursing home resident, leg ulcers or catheters, or other risk factors determined locally) | Vancomycin i.v. plus 2nd or 3rd generation cephalosporin i.v. |
| Suspected gonococcus or meningococcus | Ceftriaxone i.v. or similar dependent on local policy or resistance |
| i.v. drug users | Discuss with microbiologist |
| ITU patients, known colonisation of other organs (e.g. cystic fibrosis) | Discuss with microbiologist |
| Patient group . | Antibiotic choice . |
|---|---|
| No risk factors for atypical organisms | Flucloxacillin 2 g qds i.v. Local policy may be to add gentamicin i.v. |
| If penicillin allergic, clindamycin 450–600 mg qds i.v. or 2nd or 3rd generation cephalosporin i.v. | |
| High risk of Gram-negative sepsis (elderly, frail, recurrent UTI, and recent abdominal surgery) | 2nd or 3rd generation cephalosporin eg cefuroxime 1.5 g tds i.v. Local policy may be to add flucloxacillin i.v. to 3rd generation cephalosporin. Discuss allergic patients with microbiology—Gram stain may influence antibiotic choice |
| MRSA risk (known MRSA, recent inpatient, nursing home resident, leg ulcers or catheters, or other risk factors determined locally) | Vancomycin i.v. plus 2nd or 3rd generation cephalosporin i.v. |
| Suspected gonococcus or meningococcus | Ceftriaxone i.v. or similar dependent on local policy or resistance |
| i.v. drug users | Discuss with microbiologist |
| ITU patients, known colonisation of other organs (e.g. cystic fibrosis) | Discuss with microbiologist |
Note: antibiotic choice will need to be modified in light of results of Gram stain and culture. This table is based on expert opinion and should be reviewed locally by microbiology departments. UTI, urinary tract infection; MRSA, methicillin-resistant Staphylococcus aureus; ITU, intensive therapy unit.
| Patient group . | Antibiotic choice . |
|---|---|
| No risk factors for atypical organisms | Flucloxacillin 2 g qds i.v. Local policy may be to add gentamicin i.v. |
| If penicillin allergic, clindamycin 450–600 mg qds i.v. or 2nd or 3rd generation cephalosporin i.v. | |
| High risk of Gram-negative sepsis (elderly, frail, recurrent UTI, and recent abdominal surgery) | 2nd or 3rd generation cephalosporin eg cefuroxime 1.5 g tds i.v. Local policy may be to add flucloxacillin i.v. to 3rd generation cephalosporin. Discuss allergic patients with microbiology—Gram stain may influence antibiotic choice |
| MRSA risk (known MRSA, recent inpatient, nursing home resident, leg ulcers or catheters, or other risk factors determined locally) | Vancomycin i.v. plus 2nd or 3rd generation cephalosporin i.v. |
| Suspected gonococcus or meningococcus | Ceftriaxone i.v. or similar dependent on local policy or resistance |
| i.v. drug users | Discuss with microbiologist |
| ITU patients, known colonisation of other organs (e.g. cystic fibrosis) | Discuss with microbiologist |
| Patient group . | Antibiotic choice . |
|---|---|
| No risk factors for atypical organisms | Flucloxacillin 2 g qds i.v. Local policy may be to add gentamicin i.v. |
| If penicillin allergic, clindamycin 450–600 mg qds i.v. or 2nd or 3rd generation cephalosporin i.v. | |
| High risk of Gram-negative sepsis (elderly, frail, recurrent UTI, and recent abdominal surgery) | 2nd or 3rd generation cephalosporin eg cefuroxime 1.5 g tds i.v. Local policy may be to add flucloxacillin i.v. to 3rd generation cephalosporin. Discuss allergic patients with microbiology—Gram stain may influence antibiotic choice |
| MRSA risk (known MRSA, recent inpatient, nursing home resident, leg ulcers or catheters, or other risk factors determined locally) | Vancomycin i.v. plus 2nd or 3rd generation cephalosporin i.v. |
| Suspected gonococcus or meningococcus | Ceftriaxone i.v. or similar dependent on local policy or resistance |
| i.v. drug users | Discuss with microbiologist |
| ITU patients, known colonisation of other organs (e.g. cystic fibrosis) | Discuss with microbiologist |
Note: antibiotic choice will need to be modified in light of results of Gram stain and culture. This table is based on expert opinion and should be reviewed locally by microbiology departments. UTI, urinary tract infection; MRSA, methicillin-resistant Staphylococcus aureus; ITU, intensive therapy unit.
Joint drainage and surgical options
Septic joints should be aspirated to dryness as often as required (C).
This can be done either through a closed-needle approach or arthroscopically according to local preferences (C).
If the response is not satisfactory with a closed-needle approach, arthroscopic aspiration should be used (C).
In suspected hip sepsis, arrange early referral for an orthopaedic opinion. Urgent open debridement is often necessary (C).
Recommendations specific to primary care and the Emergency Department (ED)
The commonest hot joint to present in primary care is the great toe metatarsophalangeal joint. This is almost always due to gout and can be diagnosed on clinical grounds (B).
Some general practitioners (GPs) regularly aspirate and inject joints. If they aspirate unexpected cloudy fluid from a joint, they should send the sample with the patient to the ED and not inject corticosteroid (C).
GPs and ED doctors should refer patients with suspected septic arthritis to a specialist within the hospital who has the expertise to aspirate the joint (C).
Patients should be admitted to hospital if sepsis is suspected (C).
If there is doubt about whether sepsis might be present, intra-articular steroids should not be used (C).
The skills necessary to aspirate a joint in hospitals will commonly be held by specialists and trainees in ED, orthopaedics and rheumatology (C).
Mechanism for audit of the guidelines
In cases of proven septic arthritis:
Was the joint aspirated at presentation prior to antibiotics? If not, what was the reason?
Was there a delay in treatment and, if so, why?
Was ESR and CRP measured at diagnosis and serially?
Were appropriate cultures taken?
Was the initial antibiotic choice in keeping with the guidelines?
Was prosthetic joint sepsis managed by orthopaedic surgeons?
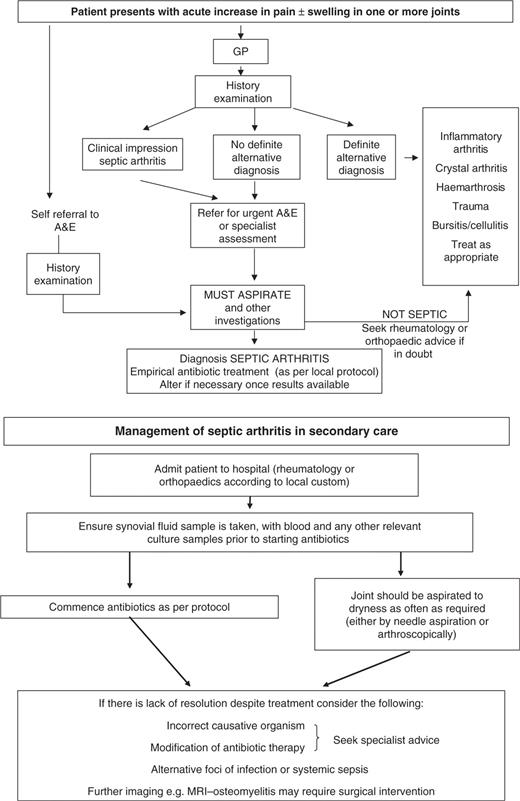
Algorithm of guidelines
The authors have declared no conflicts of interest.
Author notes
1Queen Elizabeth Hospital, Woolwich, London, 2Centre for Rheumatic Diseases, Royal Infirmary, Glasgow, 3City Hospital, Nottingham, 4University Hospital Lewisham, London, 5Freeman Hospital, Newcastle, 6King's College Hospital, London, 7Royal Orthopaedic Hospital, Birmingham (representing the British Orthopaedic Association), 8Hetherington Group Practice, London SW4, 9Arthritis Care and 10University Hospital NHS Trust, Nottingham (representing the British Society for Antimicrobial Chemotherapy), UK



Comments