Abstract
Purpose
To examine the prevalence of refractive error and distribution of ocular biometric parameters among major ethnic groups in a population-based sample of 11–15-year-old Australian children.
Methods
The Sydney Myopia Study examined 2353 students (75.3% response) from a random cluster-sample of 21 secondary schools across Sydney. Examinations included cycloplegic autorefraction, and measures of corneal radius of curvature, anterior chamber depth, and axial length.
Results
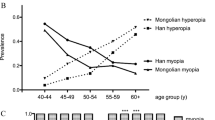
Participants mean age was 12.7 years (range 11.1–14.4); 49.4% were female. Overall, 60.0% of children had European Caucasian ethnicity, 15.0% East Asian, 7.1% Middle Eastern, and 5.5% South Asian. The most frequent refractive error was mild hyperopia (59.4%, 95% confidence interval (CI), 53.2–65.6), defined as spherical equivalent (SE) +0.50 to +1.99 D. Myopia (SE−0.50 D or less) was found in 11.9%, 95% (CI 6.6–17.2), and moderate hyperopia (SE⩾+2.00 D) in 3.5%, 95% (CI 2.8–4.1). Myopia prevalence was lower among European Caucasian children (4.6%, 95% CI 3.1–6.1) and Middle Eastern children (6.1%, 95% CI 1.3–11.0) than among East Asian (39.5%, 95%, CI 25.6–53.5) and South Asian (31.5%, 95%, CI 21.6–41.4) children. European Caucasian children had the most hyperopic mean SE (+0.82 D) and shortest mean axial length (23.23 mm). East Asian children had the most myopic mean SE (−0.69 D) and greatest mean axial length (23.86 mm).
Conclusion
The overall myopia prevalence in this sample was lower than in recent similar-aged European Caucasian population samples. East Asian children in our sample had both a higher prevalence of myopia and longer mean axial length.
Similar content being viewed by others
Introduction
Uncorrected refractive errors are a major cause of visual impairment in children worldwide, and are a priority area targeted by the World Health Organisation in the global initiative to eliminate avoidable blindness by the year 2020.1 The recent population-based Refractive Error Study in Children surveys collected data from six countries2, 3, 4, 5, 6, 7, 8, 9 and reported high myopia prevalence rates in East Asian countries and in urban areas. Among children aged 12 years, the prevalence of myopia is higher in China (18–49.7%)2, 3 and Malaysia (24.8%),4 than in Nepal (2%),5 South Africa (4%),6 India (10–10.6%),7, 8 and Chile (10%).9 In other studies, the prevalence of myopia among school children in Taiwan, Hong Kong, and Singapore ranges from 26 to 55%.10, 11, 12 Recent population-based studies of refractive error among European Caucasian children are scant.13, 14, 15 In one study among children aged 12–13 years in Sweden, the prevalence of myopia was high (49.7%).13 In the US, two studies have reported on the prevalence of myopia in children, although these rates have varied (9.2 and 28%).14, 15
Given the high prevalence of myopia in East Asian countries and the observation that myopic eyes generally have greater axial length than non-myopic eyes,12, 16 it could be postulated that ocular dimensions may differ between ethnic groups. Studies comparing ocular components by ethnicity are few,17, 18 despite recent large ocular biometry data sets published for children in Singapore, Taiwan, Malaysia, Vanuatu, and the US.10, 17, 18, 19, 20 Although the IOLMaster, a commercial biometry instrument using partial coherence interferometry is more precise than clinical ultrasound in measurement of axial length,21 few studies of ocular biometry in children, however, have utilised this tool to date.22, 23
In this paper, we aimed to (1) report the prevalence of refractive errors; and (2) use the IOLMaster to examine ocular biometric components in children from ethnic groups found in a large sample of Year 7 school children (predominantly aged 12 years) residing in Sydney, Australia.
Materials and methods
The Sydney Myopia Study is a population-based survey of eye health in school children resident in Sydney, Australia, and forms part of the Sydney Childhood Eye Study. Findings for 6-year-old children have been reported previously.23 Approval for the study was obtained from the Human Research Ethics Committee of the University of Sydney, the New South Wales Department of Education and the Catholic Education Office. The study adhered to the tenets of the Declaration of Helsinki.
Secondary schools across the Sydney metropolitan region were stratified by socio-economic status and 21 schools, including a proportional mix of public and private/religious schools, were selected to provide a representative sample of Sydney children.24 All children in Year 7 were invited to participate. After informed written consent from their parents, children underwent a detailed eye examination, which included cycloplegic autorefraction (RK-F1 autorefractor, Canon, Tokyo, Japan) and ocular biometry (IOLMaster,TM Carl Zeiss-Meditec, Jena, Germany).
Five reliable readings of refraction were generated by the autorefractor for each eye; the mean reading was used for analysis. Ocular biometry measurement included corneal radius of curvature (measured along the flattest and steepest meridians and axial length), anterior chamber depth (measured as the distance from the anterior corneal surface to the anterior lens surface), and axial length (measured as the distance from the anterior corneal vertex to the retinal pigment epithelium along the fixation line). Lens power was calculated using Bennett's formula.25
Amethocaine 0.5% (Minims™, Chauvin Pharmaceuticals, England) was used for corneal anaesthesia at 0 min, followed by cyclopentolate 1% (one drop) at 2 min for cycloplegia. Tropicamide 1% (one drop) at 3 min and phenylephrine 2.5% (one drop) at around 10 min were also used in some children to obtain adequate mydriasis. A minimum pupillary diameter of 6 mm was achieved in all children before refraction. Tropicamide was used in 53.0% and phenylephrine was used in 10.6% of students. Dilating eye drops were refused by 11 children (0.5%) who consented to non-cycloplegic autorefraction and completed all other examinations. Autorefraction was performed approximately 25 min after the last drop.
Socio-demographic information including ethnicity, highest level of parental education, and occupation were collected in questionnaires completed by parents. Ethnicity of the child was determined only if both parents shared that ethnic origin. Otherwise, children were placed in the mixed ethnicity category. Ethnicity was classified on the basis of self-identification by the parents, combined with information about the place of birth of the child. Ethnic categories (European Caucasian, East Asian, South Asian, Middle Eastern, Pacific Islander, Indigenous Australian, African, South American) were consistent with the Australian Standard Classification of Cultural and Ethnic groups (available at www.abs.gov.au, document number 1249.0), which takes into consideration the similarity in the cultural and social characteristics to determine ethnic groupings. The term East Asian covers people originating from China, Malaysia, Singapore, Indonesia, Philippines, Japan, Korea, Myanmar, Thailand, Laos, Cambodia, and Vietnam. The broad classification of East Asian was used rather than separate Northeast Asian and Southeast Asian categories because of the difficulty in classifying people derived from both of these branches. South Asian included people originating from India, Pakistan, and Nepal.
Myopia was defined as spherical equivalent (SE) refraction (sphere +½cylinder) −0.50 D or less, emmetropia as SE –0.49 to +0.49 D, mild hyperopia as SE +0.50 to +1.99 D, and moderate hyperopia as SE +2.00 D or greater.
Data were analysed using Statistical Analysis System software (SAS Institute, Cary, NC, USA). Overall distributions of refraction and ocular biometric parameters were described in terms of central tendency and spread (mean and SD). Mixed models and generalised estimating equations were used to examine associations and subgroup differences, adjusting for the effects of cluster sampling. Where cluster effects were not significant, t-tests and χ2 tests were used. All confidence intervals (CIs) are 95%. Average corneal radius of curvature was the average of the steepest and flattest meridians. Axial length/corneal radius (AL/CR) ratio was defined using the average corneal radius of curvature.
Results
Population characteristics
Overall, 2353 children were examined (75.3% response); participants and non-participants were similar in gender and ethnic background (Table 1). The mean age of participants was 12.7 years, ranging from 11.1 to 14.4 years, with 49.4% girls. Among participants, most were of European Caucasian ethnicity (60.0%), other ethnicities included East Asian (15.0%), Middle Eastern (7.1%), South Asian (5.5%), and Oceanian (3.3%). Mixed ethnicity accounted for 7.6%, and other ethnicities (African, indigenous, South American) each comprised less than 1%.
Refractive error and refraction
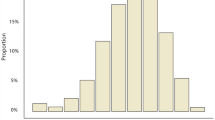
Overall, the vast majority of children had mild hyperopia (59.4%, Table 2), which was followed by emmetropia (25.3%) and myopia (11.9%), including 8.0% who had myopia of SE less than −1.00 D. Moderate hyperopia was found in 3.5%. The mean SE for the whole group was emmetropic (+0.49 D; Table 3).
Children in the European Caucasian and Middle Eastern subgroups had lower prevalence rates of myopia (4.6 and 6.1%, respectively) than children of East Asian and South Asian ethnicity (39.5 and 31.5%, respectively). Mean SE was more myopic among the East Asian (−0.69 D) and South Asian groups (−0.35 D) compared to the European Caucasian (+0.82 D) and Middle Eastern groups (+0.71 D, Table 3). Children of European Caucasian ethnicity had significantly more hyperopic SE (+0.82 D) than children from other ethnic backgrounds combined (+0.04 D, P<0.0001) after adjusting for age, gender, and height. Girls had a significantly higher prevalence of myopia than boys (14.1 vs 9.7%), with less hyperopic mean SE (+0.39 D vs +0.58 D).
Corneal radius of curvature and axial length
Mean corneal radius was steeper in children of European Caucasian ethnicity and South Asian ethnicity than in children of other ethnic groups (Table 3). Mean axial length was shorter in the European Caucasian and the Middle Eastern subgroups (Table 3). Boys had slightly flatter corneas (7.84 vs 7.73 mm, P<0.0001) and longer eyes (23.72 vs 23.30 mm, P<0.0001) than girls.
Anterior chamber depth and lens power
Mean anterior chamber for the whole group was 3.67 mm, and was deeper in European Caucasian children compared to East Asian children (3.67 vs 3.62 mm, P=0.047), adjusting for age, gender, and height. However, anterior chamber depth in European Caucasian children was similar to that in South Asian children and Middle Eastern children (both P>0.05). Boys had deeper chambers than girls (3.73 vs 3.61 mm, P<0.0001).
Calculated lens power was 22.15 D for the whole group, and was weaker in children of East Asian ethnicity than in children of European Caucasian ethnicity (22.03 vs 22.18 D, P=0.02). Lens power in the European Caucasian group was similar to that in South Asian children and in Middle Eastern children (both P>0.05). Boys had weaker lens power than girls (21.67 vs 22.65 D, P<0.0001).
Axial length in emmetropia and myopia, differences in two major ethnic groups
The distribution of axial length among emmetropic children was similar between European Caucasian and East Asian children, with similar mean axial length (23.49 mm for European Caucasian and 23.45 mm for East Asian children, respectively, shown in Figure 1). Among myopic children, there was a wide distribution and overlap of axial length in both European Caucasian and East Asian subgroups; differences between these two ethnic groups included a higher proportion of children with greater axial lengths and a tendency towards longer axial length among the East Asian subgroup. In children with myopia, mean axial length was slightly longer in the East Asian subgroup (24.66 mm) than in the European Caucasian subgroup (23.99 mm). Considerable overlap in the distribution of axial length was noted between emmetropic and myopic children.
Discussion
Prevalence of SE errors
In this large population-based sample of Sydney children with a mean age of 12.7 years, the prevalence of myopia was 11.9%, whereas the prevalence of moderate hyperopia was 3.5%. The mean SE (+0.49 D) was just within the emmetropic range.
Comparison of refractive error prevalence rates with other studies is difficult due to the use of different definitions, instrumentation, variable use of cycloplegia, plus differences in other population characteristics such as ethnicity, gender, and age distribution. In studies of predominantly European Caucasian children, the reported prevalence for myopia ranges from 11.6 to 49.7%.13, 14, 15, 26 Junghans and Crewther26 reported only a slightly higher prevalence of myopia (14.7%) in urban Australian children, using non-cycloplegic retinoscopy. This method, however, increases measurement variability and is likely to underestimate hyperopia,2 emphasising the importance of cycloplegia. In studies among predominantly European Caucasian children in the US, Zadnik15 reported a prevalence of myopia of around 20% for children aged 12 years and Kleinstein et al14 reported a prevalence of 11.6% for children aged 5–17 years in the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error. Among 12–13-year-old children in Sweden, Villarreal et al13 reported a myopia prevalence of 49%. These values are consistently higher than the low prevalence of myopia in 12-year-old European Caucasian children reported in this study (4.6%).
The overall prevalence of myopia in the current study was very substantially lower than that reported for similarly aged East Asian children (36.7–78.4%),2, 3, 11, 27 using the same definition for myopia (SE −0.50 D or less). The overall prevalence of myopia in this study was, however, higher than that reported for children in Chile, Nepal, India, and South Africa (Table 4).5, 6, 7, 8, 9
Ethnic differences in the prevalence of myopia
In this study, children of European Caucasian ethnicity had both a lower prevalence of myopia and a more hyperopic SE than children of East Asian ethnicity. A new finding was that children of South Asian ethnicity had a similar myopia prevalence and myopic SE as children of East Asian ethnicity. Ethnic differences in myopia have also been reported in other studies among children in school-based settings.12, 14 Kleinstein et al14 reported a higher prevalence of myopia among Asian children (18.5%) than White children (4.4%), aged 5−17 years. Each ethnic sample (African American, Asian, Hispanic, and White) was predominantly drawn from relatively different environments; therefore, these differences in myopia prevalence cannot be attributed to ethnicity alone. A study of children aged 7−9 years from two schools in Singapore12 showed that the prevalence of myopia among Chinese children (37.0%) was higher than among non-Chinese children (19.9%). Ethnic associations with myopia may not necessarily indicate a purely genetic influence, but could reflect enduring patterns of behaviour and cultural attitudes that may result in a more myopigenic environment, such as higher levels of more intense near-work and lower levels of outdoor activity.
The prevalence of myopia in East Asian children in the current study is lower than that in other studies among East Asian children in urban areas, where the prevalence of myopia ranges from 48.2 to 60.0% (Table 4). These differences in myopia prevalence among children of East Asian ethnicity suggest that a high prevalence of myopia is not inherently universal. The association of an urbanised environment with myopia development could be mediated by factors such as higher educational attainment and greater levels of near-work, with possible differences in duration and intensity of study between children of urban and rural areas.
Gender differences in myopia
The higher prevalence of myopia in girls reported in the current study was also described in our 6-year-old cohort,23and is consistent with a number of studies among Asian,2, 4, 10, 11 rural Indian,8 and Caucasian childhood populations.20 No gender differences, however, were found in studies of children in urban India,7 South Africa,6 Nepal,5 and Chile.9
The higher rate of myopia and lower rate of moderate hyperopia in girls in our study is consistent with their lower mean SE; however, the reasons for these findings are unclear. One possible explanation is that girls may perform more near-work than boys; however, recent papers have raised some doubt over the relative importance of near-work as a risk factor for myopia.28 Another suggestion is that earlier pubertal changes in girls are responsible; however, in our findings we have shown that mean axial length was shorter in girls than boys, making a hormonal cause for myopia less likely.
Hyperopia
Hyperopia is an important condition because of its association with amblyopia, strabismus, and anisometropia in children.29 Although the prevalence of moderate hyperopia varies among different countries (Table 4), these differences are typically less dramatic than the differences in myopia prevalence. The prevalence of moderate hyperopia in our sample was comparable to that in urban India,7 but was higher than rates reported for East Asian countries,2, 3, 4, 11, 27 rural India,8 and South Africa.6
Populations with a high prevalence of myopia generally have a relatively low prevalence of hyperopia (Table 4). This suggests that the decrease in prevalence of moderate hyperopia with age may be due to an overall myopic shift in the population, which, in turn, are associated with age-related physiological changes in ocular biometry. However, in locations such as Nepal, rural India, and South Africa, where the prevalence of myopia is very low, factors other than age-related myopic shift may also contribute to a low prevalence of hyperopia.
Ocular biometry
Age-specific ocular biometric data for children have been published for older children in the US17, 20 and Taiwan.10 These reports used ultrasound measurements and provided gender-stratified data but not overall data for each age year, making comparison with our ethnic subgroups difficult. The mean axial length in boys (23.58 mm) and girls (23.18 mm) obtained by IOLMaster in our study were actually comparable to those reported by Zadnik et al20 for similarly aged children (23.55 and 23.27 mm in boys and girls, respectively). Lin et al10 reported similar findings for Taiwanese girls (23.6 mm) but slightly longer mean axial length (24.1 mm) in Taiwanese boys, both aged 12 years. Mean axial length for children of East Asian ethnicity in our study was 23.86 mm.
Among studies of children with myopia, mean axial length was generally longer. In the Correction of Myopia Evaluation Trial study,17 which only included children with myopia, axial length in those aged 11 years was 24.62 mm in boys and 24.23 mm in girls. In younger Singaporean children (ages 7−9 years), axial length measurements obtained using ultrasound for those with low myopia (23.76 mm) or high myopia (24.81 mm) were greater than that found in 12-year-old children (23.38 mm) in the current study.
Our finding that boys generally had a more hyperopic refraction and longer eyes with deeper anterior chambers than girls is consistent with previous studies using ultrasound measurements.10, 17 Some studies have also reported weaker lens power20 and thinner lens10 among boys. Although there were highly statistically significant gender differences in mean corneal radius and axial length, the actual differences were quite small (0.1 and 0.4 mm, respectively) and translated into only a small difference in SE (0.19 D) between boys and girls. Therefore, in clinical terms, the differences of ocular biometry between boys and girls may be considered relatively inconsequential.
Strengths and limitations
We used random cluster sampling to obtain a large representative sample of children in the Sydney metropolitan region. Both satisfactory response rate, and the use of cycloplegic refraction and standardised measurement protocols contributed to the strengths of this study. By examining a large sample of children within one school year, we are able to control the influences of schooling to a certain extent and make valid comparisons of ocular dimensions between boys and girls, and between ethnic groups. We assigned ethnicity for the child by using data from both parents to increase accuracy and excluded children of mixed race from ethnic comparisons. Ocular biometry measurements were obtained by the IOLMaster, which are considered to be more precise and repeatable than those obtained using ultrasound.21 As previous reports have shown that axial length measurement by non-immersion ultrasound are shorter,30 IOLMaster measurements were internally adjusted for comparison.
A limitation of this study was the use of calculated lens power. This was based on the Gullstrand–Emsley schematic eye, and assumed a theoretical relationship between ocular components in the adult eye. Measurement of vitreous chamber depth was not performed with the IOLMaster. With a cross-sectional design, data on development and progression of myopia are outside the scope of this study. Comparing the current findings in 12-year-old children with our previously published data for 6-year-old children, however,23 the older children had a higher prevalence of myopia, longer axial length, longer anterior chamber depth, weaker lens power, and a more myopic SE than the younger children. There was no apparent change in the corneal radius between the two samples.
In summary, in this study of 12-year-old children, we report a relatively low prevalence of myopia by international standards in age-matched cohorts. There were substantial ethnic differences in the prevalence of different refractive errors and in ocular dimensions within this sample of children from diverse ethnic backgrounds. Among the four major ethnic groups, myopia prevalence ranged from European Caucasian (lowest), Middle Eastern, South Asian, and East Asian (highest) with corresponding range of increasing axial length.
References
Pizzarello L, Abiose A, Ffytche T, Duerksen R, Thulasiraj R, Taylor H et al. Vision 2020: the right to sight. A global initiative to eliminate avoidable blindness. Arch Ophthal 2004; 122: 615–620.
Zhao J, Pan X, Sui R, Munoz SR, Sperduto RD, Ellwein LB . Refractive error study in children: results from Shunyi district, China. Am J Ophthalmol 2000; 129: 427–435.
He M, Zeng J, Liu Y, Xu J, Pokharel GP, Ellwein LB . Refractive error and visual impairment in urban children in southern china. Invest Ophthalmol Vis Sci 2004; 45: 793–799.
Goh PP, Abqariyah Y, Pokharel GP, Ellwein LB . Refractive error and visual impairment in school-age children in Gombak district, Malaysia. Ophthalmology 2005; 112: 678–685.
Pokharel GP, Negrel AD, Munoz SR, Ellwein LB . Refractive error study in children: results from Mechi Zone, Nepal. Am J Ophthalmol 2000; 129: 436–444.
Naidoo KS, Raghunandan A, Mashige KP, Govender P, Holden BA, Pokharel GP et al. Refractive error and visual impairment in African children in South Africa. Invest Ophthalmol Vis Sci 2003; 44: 3764–3770.
Murthy GV, Gupta SK, Ellwein LB, Munoz SR, Pokharel GP, Sanga L et al. Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci 2002; 43: 623–631.
Dandona R, Dandona L, Srinivas M, Sahare P, Narsaiah S, Munoz SR et al. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci 2002; 43: 615–622.
Maul E, Barroso S, Munoz SR, Sperduto RD, Ellwein LB . Refractive error study in children: results from La Florida, Chile. Am J Ophthalmol 2000; 129: 445–454.
Lin LL, Shih YF, Tsai CB, Chen CJ, Lee LA, Hung PT et al. Epidemiologic study of ocular refraction among schoolchildren in Taiwan in 1995. Optom Vis Sci 1999; 76: 275–281.
Fan DS, Lam DS, Lam RF, Lau JT, Chong KS, Cheung EY et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci 2004; 45: 1071–1075.
Saw SM, Chua WH, Hong CY, Wu HM, Chan WY, Chia KS et al. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci 2002; 43: 332–339.
Villarreal MG, Ohlsson J, Abrahamsson M, Sjostrom A, Sjostrand J . Myopisation: the refractive tendency in teenagers. Prevalence of myopia among young teenagers in Sweden. Acta Ophthalmol Scand 2000; 78: 177–181.
Kleinstein RN, Jones LA, Hullett S, Kwon S, Lee RJ, Friedman NE et al. Refractive error and ethnicity in children. Arch Ophthalmol 2003; 121: 1141–1147.
Zadnik K . The Glenn A. Fry Award Lecture (1995). Myopia development in childhood. Optom Vis Sci 1997; 74: 603–608.
Goss DA, Cox VD, Herrin-Lawson GA, Nielsen ED, Dolton WA . Refractive error, axial length, and height as a function of age in young myopes. Optom Vis Sci 1990; 67: 332–338.
Gwiazda J, Marsh-Tootle WL, Hyman L, Hussein M, Norton TT . Baseline refractive and ocular component measures of children enrolled in the correction of myopia evaluation trial (COMET). Invest Ophthalmol Vis Sci 2002; 43: 314–321.
Garner LF, Meng CK, Grosvenor TP, Mohidin N . Ocular dimensions and refractive power in Malay and Melanesian children. Ophthalmic Physiol Opt 1990; 10: 234–238.
Luo HD, Gazzard G, Fong A, Aung T, Hoh SK, Loon SC et al. Myopia, axial length, and OCT characteristics of the macula in Singaporean children. Invest Ophthalmol Vis Sci 2006; 47: 2773–2781.
Zadnik K, Manny RE, Yu JA, Mitchell GL, Cotter SA, Quiralte JC et al. Ocular component data in schoolchildren as a function of age and gender. Optom Vis Sci 2003; 80: 226–236.
Lam AK, Chan R, Pang PC . The repeatability and accuracy of axial length and anterior chamber depth measurements from the IOLMaster. Ophthalmic Physiol Opt 2001; 21: 477–483.
Huynh SC, Kifley A, Rose KA, Morgan I, Heller GZ, Mitchell P . Astigmatism and its components in 6-year old children. Invest Ophthalmol Vis Sci 2006; 47: 55–64.
Ojaimi E, Rose KA, Morgan IG, Smith W, Martin FJ, Kifley A et al. Distribution of ocular parameters and refraction in a population-based study of Australian children. Invest Ophthalmol Vis Sci 2005; 46: 2748–2754.
Ojaimi E, Rose KA, Smith W, Morgan IG, Martin FJ, Mitchell P . Methods for a population-based study of myopia and other eye conditions in school children: the Sydney Myopia Study. Ophthalmic Epidemiol 2005; 12: 59–69.
Bennett AG, Rabbetts RB Clinical Visual Optics. Butterworth-Heinemann Ltd: Oxford, 1989.
Junghans BM, Crewther SG . Little evidence for an epidemic of myopia in Australian primary school children over the last 30 years. BMC Ophthalmol 2005; 5: 1.
Lin LL, Shih YF, Hsiao CK, Chen CJ . Prevalence of myopia in Taiwanese schoolchildren: 1983–2000. Ann Acad Med Singapore 2004; 33: 27–33.
Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K . Parental myopia, near work, school achievement, and children's refractive error. Invest Ophthalmol Vis Sci 2002; 43: 3633–3640.
Committee for the Classification of Eye Movement Abnormalities and Strabismus. A classification of eye movement abnormalities and strabismus (CEMAS). 2001 pp 1–56 National Eye Institute http://www.nei.nih.gov/news/statements/cemas.pdf. Accessed January 2007.
Carkeet A, Saw SM, Gazzard G, Tang W, Tan DTH . Repeatability of IOLMaster biometry in children. Optom Vis Sci 2004; 81: 829–834.
Acknowledgements
The Sydney Myopia Study is supported by the Australian National Health & Medical Research Council (Grant No. 253732); the Westmead Millennium Institute, University of Sydney; and the Vision Co-operative Research Centre, University of New South Wales, Sydney, Australia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary Interest: None
Rights and permissions
About this article
Cite this article
Ip, J., Huynh, S., Robaei, D. et al. Ethnic differences in refraction and ocular biometry in a population-based sample of 11–15-year-old Australian children. Eye 22, 649–656 (2008). https://doi.org/10.1038/sj.eye.6702701
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702701
Keywords
This article is cited by
-
Investigation of ocular biometry in 4– to 9-year-old Chinese children
BMC Ophthalmology (2023)
-
Clinically Significant Axial Shortening in Myopic Children After Repeated Low-Level Red Light Therapy: A Retrospective Multicenter Analysis
Ophthalmology and Therapy (2023)
-
Myopia prevalence and ocular biometry: a cross-sectional study among minority versus Han schoolchildren in Xinjiang Uygur autonomous region, China
Eye (2022)
-
A review on the epidemiology of myopia in school children worldwide
BMC Ophthalmology (2020)
-
Myopia
Nature Reviews Disease Primers (2020)