Abstract
Purpose To evaluate the long-term results of combined treatment with excision and cryosurgery for malignant epithelial tumours of the conjunctiva.
Methods We retrospectively reviewed the medical records of patients diagnosed with conjunctival malignant epithelial tumours and treated with excision and cryosurgery between 1980 and 1998. The demographic features of the patients, characteristics of the tumours, and the peculiarities of the recurrences were recorded. The SPSS V 9.05 computed program was used for the statistical analysis of the results. Kaplan–Meier plots were used to determine the recurrence-free survival, and the logrank test was used to compare the recurrences according to histological classification.
Results A total of 55 subjects (57 eyes), 19 female and 36 male, were included in the study. Their ages ranged between 15 and 82 years (mean 55±14 years). Histological diagnosis was conjunctival intraepithelial neoplasia (CIN) in 26 (46%) and invasive squamous cell carcinoma (SCC) of the conjunctiva in 31 eyes (54%). All eyes were treated with excision and cryosurgery with nitrous oxide probe. During the follow-up period of 6 months to 15 years, seven (12.3%) recurrences were observed. The success rate for patients with CIN and invasive SCC was 88.5 and 87.1%, respectively. There was no difference for recurrence rates between CIN and invasive SCC groups according to logrank test (P=0.68).
Conclusions Over the long-term follow-up, cryosurgery following excision is a successful method in the treatment of conjunctival intraepithelial tumours and invasive squamous cell carcinoma of conjunctiva with favourable outcome and minimal complications.
Similar content being viewed by others
Introduction
Conjunctival malignant epithelial tumours are seen rarely in everyday practice, but they are the most common malignant lesions of the conjunctiva.1 These tumours usually originate near the limbus, frequently involve the bulbar conjunctiva and the cornea, and sometimes spread towards the fornices.1 They are usually located within the palpebral opening and require active treatment to prevent visual and ocular loss.2 The tumours are more prevalent in men than women, and typically occur in middle-aged to elderly people with a history of high ultraviolet exposure.1 Association with cigarette smoking, petroleum derivative exposure, AIDS and chronic papilloma-virus infection history has been described.2,3
Clinically it can be hard to differentiate conjunctival intraepithelial neoplasia (CIN) and early invasive squamous cell carcinoma (SCC). Owing to the superficial arrangement of the lesion, the conjunctiva moves freely over the underlying episcleral tissue in both these conditions.1 In CIN, the subepithelial basement membrane is intact and the tumour is confined to the epithelium.4 In invasive SCC, the malignant cells extend beyond the epithelial basement membrane into the stroma or substantia propria and the tumour may fixate to the underlying tissues. The tumour rarely extends deeper into the eye or orbit.2,4
The most common treatment for CIN and invasive SCC has been surgical excision. This method has a recurrence rate of 30–40%.5,6,7,8 This high recurrence rate can be explained by the inadequate surgical margins and small tumour remnants, which might remain after excision.7 Thus, the positive excision margin at the time of surgery was suggested as the most important factor in predicting recurrence.8 In order to reduce the recurrence rates, supplemental treatment methods have been used after complete excision of the tumour. Cryosurgery,1,4,9 radiation therapy,10,11,12 topical retinoic acid,13 and alpha 2 interferon14,15 were reported as adjunctive treatment forms. There have also been reports of favourable treatment with topical mitomycin C.16,17 Enucleation or exenteration may be necessary in advanced cases. However, surgical excision of the tumour followed by cryosurgery is the most commonly chosen treatment method. In this study the long-term results of cryosurgery following complete excision of the malignant epithelial tumours of the conjunctiva were evaluated.
Materials and methods
We retrospectively reviewed the medical records of 104 consecutive patients with the diagnosis of malignant epithelial tumour of the conjunctiva, who were seen at our Ophthalmic Oncology Service between 1980 and 1998. The patients who were lost to follow-up in less than 6 months or who received other treatment modalities were excluded from the study. A total of 55 patients were treated with cryo-application in conjunction to the excision of the tumour.
The demographic features of the patients, the location and size of the tumour, histological classification, complication rates, follow-up time, and postoperative outcome were recorded. The cases with recurrence were evaluated in detail.
Surgery was performed by the same surgeon (GP) with excision combined with double freeze–thaw cryosurgery. The surgical technique was as follows: local anaesthesia was accomplished by subconjunctival injection of 20 mg lidocaine hydrochloride in 1.25% epinephrine. Before the excision, cryosurgery was applied to the margins and beyond the tumour with a nitrous oxide cryo-unit (Elbe, Germany), 2.5 mm retinal cryoprobe tip. Cryosurgery was performed until an ice-ball around the probe was formed as 2 mm for the conjunctiva, 1 mm for episcleral tissues and corneoscleral limbus, and 0.5 mm for the cornea. The ice-ball was then allowed to slowly thaw and was refrozen in the same location. This was repeated at the next location (usually 3 mm apart). The tumour was excised with the surrounding 2 mm healthy appearing conjunctiva down to bare scleral base. A superficial sclerectomy was performed only where the conjunctiva was adherent to the episcleral area. With at least 1 mm normal epithelium, the tumour was scraped from the cornea using a no. 64 Beaver blade sparing the Bowman membrane, which may be a natural barrier to penetration. The wound was closed with end-to-end closure of the Tenon capsule and the conjunctiva with interrupted 6/0 absorbable sutures. After the excision, cryosurgery was repeated at the locations where the tumour was present. Postoperatively, antibiotic and corticosteroid drops were used in all subjects four times a day for 2–3 weeks. The pathological identification was evaluated by one of the authors (GP), qualified in ophthalmic pathology.
The statistical analysis of the results was performed using the SPSS V 9.05, for windows computed program. Kaplan–Meier plots were used to analyse the recurrence-free survival, and the logrank test was used for the comparison of the recurrence rates in patient groups.
Results
A total of 57 eyes of 55 subjects received a combination of excision and cryosurgery for the treatment of malignant epithelial tumour of the conjunctiva. In two patients, both eyes were involved. Patients' age ranged between 15 and 82 years (mean 55±14 years, median 56 years). There were 36 male (65%) and 19 female (35%) patients with a mean age of 53±15 and 59.5±11 years, respectively.
In 46 eyes (81%), the tumour was located at the corneoscleral limbus. Of these 46 eyes, the cornea or the limbus was involved in 32 (56%), and both the cornea and the conjunctiva were involved in 14 (25%) eyes. In eight eyes (14%) the tumour was located on the bulbar conjunctiva, and in three (5%) at the medial or lateral canthus. Tumour sizes varied from 0.5 × 0.5 to 1.5 × 2 cm. In 31 eyes (54%) the tumour was less than 1 × 1 cm, whereas in 26 eyes (46%) it was larger.
The histological diagnosis was invasive SCC of the conjunctiva in 29 eyes (51%) and CIN in 28 eyes (49%). A total of 49 eyes (86%) were primarily seen and treated at our clinic. Eight (14%) subjects had excision of the primary tumour elsewhere and were referred to us for recurrent tumours.
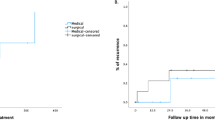
The follow-up time of patients in this study ranged from 6 months to 15 years, with a mean of 31.7±28 months. In the follow-up period, seven recurrences (12.3%) were detected. The overall success rate of performing cryosurgery in addition to excision of the tumour was 87.7% in patients with malignant epithelial tumours of the conjunctiva for a mean follow-up of 30 months. The success rate in patients with histological diagnosis of CIN was 89.3% (25 in 28 eyes), and in patients with invasive SCC it was 86.2% (25 in 29 eyes). Cumulative recurrence-free survival of patients was 91% at 1 year, 87% at 2 years, and 68% at 5 years. The cumulative recurrence-free survivals for CIN and invasive SCC were 93 and 88% for the first postoperative year, 83 and 81% for the second year, and 66 and 69% for the fifth year, respectively (Figure 1). With the logrank test, there was no statistically significant difference for recurrence rates between CIN and invasive SCC groups (P=0.68).
The features of the patients with recurrence are presented in Table 1. All seven cases had their primary surgery at our clinic. The recurrent cases were four females and three males, and the mean age was 60±16.5 years. Primary tumour size ranged between 0.5 and 1.5 cm. The median (±SE) time to recurrence was 18±8 months and the confidence interval (CI) ranged between 3 and 33 months. Histological diagnosis was CIN in three eyes and invasive SCC in four eyes. The median time for recurrence after surgery was 36±20 months in the CIN, and 12±4 months in the invasive SCC diagnosed group.
In one subject, cryosurgery alone was sufficient as the secondary treatment. We applied the same surgical technique to four of the recurrent cases and two of them were tumour free during the follow-up. Three of the 57 eyes (5%) were lost (exenterated) owing to intraocular or orbital involvement. Considering the secondary treatment, the overall success rate was raised to 94.7%. The success rate rose to 100% in the CIN group when the secondary procedures were included. In the invasive SCC group, three eyes were exenterated because of advanced tumour infiltrating the intraorbital tissues.
In the follow-up period, temporary ocular hypertension was observed in five eyes, and minimal corneal scarring and mild superficial corneal vascularization were observed in three eyes. No other complications were seen in the remaining patients.
Discussion
Malignant epithelial tumours of the conjunctiva grow in all directions resembling tree roots. Therefore, simple surgical excision, even with wide margins, could miss small root tips at the edge and/or base of the scleral bed. It is proposed that superficial freezing with cryoprobe destroys small islands of tumour cells resulting in improved cure rates.18 Lee and Hirst2 suggested that cryosurgery affects initially by its thermal effect; later it obliterates the microcirculation, and ischemic infarction of the tissue occurs. Thus, it acts on the superficially as well as deeply infiltrated tumours. It has also been suggested that cryosurgery may also act by way of an immunologic response to released tumour antigens as a late result.19
Adjunctive cryosurgery with double freeze–thaw technique can be used at the scleral base of the tumour as well as on tumour-free conjunctival margins.1 For the best results, repeated rapid freeze and slow thaw is recommended.20 Fraunfelder and Wingfield9 reported a recurrence rate of 8% for the tumour excision followed by cryosurgery with a liquid-nitrogen probe (Table 2). Divine and Anderson19 reported their recurrence rate as 11% in patients with nitrous oxide cryosurgery after surgical removal of the tumour. Peksayar et al20 reported a 9% recurrence rate after excision combined with cryosurgery with the same technique. In the present series with a longer follow-up, we observed a recurrence rate of 12.3%, with seven recurrences in 57 eyes, after primary surgery. The surgical technique in this study is similar to the previous studies.19,20,21 In a study reporting the results of frozen section controlled excision and adjunctive cryosurgery, the rate of new recurrences was 4.5% for CIN and 5.3% for invasive SCC.22 In our clinical practice, we do not perform frozen section because it is not technically feasible.
Statistically there was no difference in the recurrence rates for CIN and invasive SCC groups. However, the results of retreatments are apparently more favourable for CIN, since there were no eye losses in the CIN group, but three of four recurrent cases with invasive SCC had to be exenterated.
Cryosurgery is suggested to destroy small islands of tumour cells in the above-mentioned manners.2,18,19 Therefore, while performing this procedure, surgeons should avoid the removal of deeper tissues such as the sclera. Excessive freezing of the corneoscleral limbus and ciliary body may result in sectorial iris atrophy, ocular hypotony, thermal inflammatory oedema, iritis, and corneal scarring.20 In this series, such complications were not observed. Only temporary ocular hypertension and minimal corneal scarring with mild superficial corneal vascularization was observed in five and three eyes, respectively. This is probably owing to diligent application of cryosurgery avoiding excessive freezing.
The interval between the first excision and recurrence is reported to be approximately 22 months;23 in the present study, it was 27 months. Although epithelial tumours usually recur within the first 2 years,2 recurrence even 11 years after treatment has been reported.8 In the present study, we observed recurrences up to 5 years after primary treatment. Since it is possible for the patients to have a predilection to get new primary tumour, these patients should be observed for a long period after first surgery. We treated both the primary tumours and recurrences successfully with excision plus cryosurgery if the tumour has no intraocular invasion; thus, we think that excision combined with cryosurgery is successful in the treatment of recurrent tumours. With advanced tumours, unfortunately more radical treatment options like exenteration of the orbit are to be chosen.
Over the long-term follow-up, we observed that excision combined with cryosurgery is a successful method in the treatment of conjunctival malignant epithelial tumours. We think excision of the surgical margins of the tumour combined with nitrous oxide cryosurgery should be the preferred form of treatment for CIN and invasive SCC of the conjunctiva, if the tumour has no intraocular or intraorbital extensions. Additionally, we suggest observing the subjects with regular intervals for the rest of their lives.
References
Char DH . Conjunctival malignancies: diagnosis and management. In: Char DH (ed). Clinical Ocular Oncology, 2nd edn. Lippincott-Raven Publishers: Philadelphia, 1997, pp 60–86.
Lee GA, Hirst LW . Ocular surface squamous neoplasia. Surv Ophthalmol 1995; 39: 429–450.
Egbert JE, Kersten RC . Female genital papillomavirus in conjunctival papillomas of infancy. Am J Ophthalmol 1997; 123: 551–552.
Apple DJ, Rabb MF . Ocular Pathology: Clinical Application and Self Assessment, 4th edn. Mosby Year Book: St Louis, 1991.
Winter FC, Kleh TR . Precancerous epithelioma of the limbus. Arch Ophthalmol 1960; 64: 208–215.
Carroll JM, Kuwabara T . A classification of limbal epitheliomas. Arch Ophthalmol 1965; 73: 545–551.
Pizzarello LD, Jacobiec FA . Bowen's disease of the conjunctiva: a misnomer. In: Jacobiec FA (ed). Ocular and Adnexal Tumors. Aesculapius: Birmingham, AL, 1978, pp 553–571.
Tabin G, Levin S, Snibson G, Laughnan M, Taylor H . Late recurrences and necessity for long-term follow-up in corneal and conjunctival intraepithelial neoplasia. Ophthalmology 1997; 104: 485–492.
Fraunfelder FT, Wingfield D . Management of intraepithelial conjunctival tumors and squamous cell carcinoma. Am J Ophthalmol 1983; 95: 359–363.
Goldberg JR, Becker SC, Rosenbaum HD . Gamma radiation in the treatment of squamous-cell carcinoma of the limbus. Am J Ophthalmol 1963; 55: 811–815.
Lommatzsch P . Beta-ray treatment of malignant epithelial tumors of the conjunctiva. Am J Ophthalmol 1976; 81: 198–206.
Ullman S, Augsburger JJ, Brady LW . Fractioned epibulbar I-125 plaque radiotherapy for recurrent mucoepidermoid carcinoma of the bulbar conjunctiva. Am J Ophthalmol 1995; 119: 102–103.
Herbort CP, Zografos L, Zwingli M, Schoeneich M . Topical retinoic acid in dysplastic and metaplastic keratinization of corneoconjunctival epithelium. Graefes Arch Clin Exp Ophthalmol 1988; 226: 22–26.
Maskin SL . Regression of limbal epithelial dysplasia with topical interferon. Arch Ophthalmol 1994; 112: 1145–1146.
Vann RR, Karp CL . Perilesional and topical interferon alfa-2b for conjunctival and corneal neoplasia. Ophthalmology 1999; 106: 91–97.
Frucht-Pery J, Rozenman Y . Mitomycin C therapy for corneal intraepithelial neoplasia. Am J Ophthalmol 1994; 117: 164–168.
Frucht-Pery J, Rozenman Y, Pe'er J . Topical mitomycin-c for partially excised conjunctival squamous cell carcinoma. Ophthalmology 2002; 109: 548–552.
Fraunfelder FT . Cryosurgery of eyelid: conjunctival and intraocular tumors. In: Zacarian SA (ed). Cryosurgery for Skin Cancer and Cutaneous Disorders. CV Mosby: St Louis, 1985, pp 259–273.
Divine RD, Anderson RL . Nitrous oxide cryotherapy for intraepithelial epithelioma of the conjunctiva. Arch Ophthalmol 1983; 101: 782–786.
Peksayar G, Soytürk MK, Demiryont M . Long-term results of cryotherapy on malignant epithelial tumors of the conjunctiva. Am J Ophthalmol 1989; 107: 337–340.
Shields JA, Shields CL, DePotter P . Surgical management of conjunctival tumors. The 1994 Lynn B. McMahan Lecture. Arch Ophthalmol 1997; 115: 808–815.
Tunc M, Char DH, Crawford B, Miller T . Intraepithelial and invasive squamous cell carcinoma of the conjunctiva: analysis of 60 cases. Br J Ophthalmol 1999; 83: 98–103.
Erie JC, Campbell RJ, Liesegang J . Conjunctival and corneal intraepithelial and invasive neoplasia. Ophthalmology 1986; 93: 176–183.
Acknowledgements
This work was partially supported by the BEKADEP Project of Istanbul University.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented as a scientific paper at SOE ′99, XIIth European Congress of Ophthalmology, Stockholm, Sweden, 27 June–1 July 1999
Rights and permissions
About this article
Cite this article
Peksayar, G., Altan-Yaycioglu, R. & Onal, S. Excision and cryosurgery in the treatment of conjunctival malignant epithelial tumours. Eye 17, 228–232 (2003). https://doi.org/10.1038/sj.eye.6700331
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700331
Keywords
This article is cited by
-
Kasuistik: Management eines limbalen Carcinoma in situ der Bindehaut
Spektrum der Augenheilkunde (2022)
-
Ocular surface squamous neoplasia: outcomes following primary excision with 2 mm margin and cryotherapy
Eye (2021)
-
Role of topical interferon alpha-2b in ‘mitomycin-C-resistant’ ocular surface squamous neoplasia: our preliminary findings
International Ophthalmology (2019)
-
Invasives Plattenepithelkarzinom der Bindehaut
Der Ophthalmologe (2013)
-
Long-term follow-up of invasive ocular surface squamous cell carcinoma treated with excision, cryotherapy, and topical mitomycin C
Graefe's Archive for Clinical and Experimental Ophthalmology (2012)