Abstract
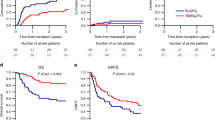
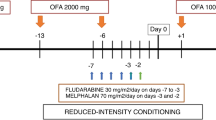
In the present paper, we evaluate tolerability, outcome and prognostic factors in patients with poor prognosis non-Hodgkin’s lymphoma (NHL) and Hodgkin’s disease (HD) when uniformly treated with BCNU, etoposide, cytarabine and melphalan (BEAM) and autologous stem cell transplant (ASCT). One hundred and forty-eight patients with NHL (n = 112) or HD (n = 36) received BEAM followed by infusion of bone marrow (n = 55), peripheral blood stem cells (n = 79) or both (n = 14). Twenty-eight patients had low-grade lymphoma (LGL), 68 intermediate- and 16 high-grade lymphoma (IGL). Within the NHL group, 21 patients were in 2nd or subsequent complete remission (CR) at transplant, 34 had sensitive disease and 11 resistant disease; 46 patients were transplanted in 1st CR due to the presence of ⩾2 adverse prognostic features at diagnosis or to a slow CR. Of the HD patients at transplant 17 had active disease, 16 were in ⩾2 CR and three in 1st CR. The overall percentage of toxic deaths was 5.4%, while in the group of patients transplanted with PBSC it was only 1.3%. NHL patients: 78% were in CR following ASCT, including 25 out of 45 patients (56%) who were transplanted with active disease. Only two of the 11 patients transplanted with resistant disease achieved CR. Incidence of overall survival (OS) and disease-free survival (DFS) at 3 years was 65 and 75%, respectively. As far as histology was concerned, OS was significantly better for patients with LGL in comparison with IGL (88 vs 56%) (P = 0.002). DFS was significantly higher for patients transplanted in first CR or first partial remission (PR) than it was for those transplanted in a later CR or PR (86 vs 53%) (P = 0.02). Multivariate analysis for OS showed that histology, bulky disease, poor performance status at transplant and achievement of CR were independent prognostic factors. In addition, a high number of infused MNC was associated with poor DFS. HD patients: 30 (83%) were in CR after transplantation, with 25 maintaining CR at the end of the study. Only one of the four patients transplanted with resistant disease reached CR. Incidence of OS and DFS at 3 years was 78 and 81%. DFS was similar for patients transplanted with early or late relapse (95 and 93%). With multivariate analysis, the only independent variable for OS was CR after transplant. In conclusion, the present results demonstrate the efficacy and low toxicity of the BEAM regimen in high-risk lymphoma patients with sensitive disease. Other strategies should be investigated for patients with refractory lymphoma.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Caballero, M., Rubio, V., Rifon, J. et al. BEAM chemotherapy followed by autologous stem cell support in lymphoma patients: analysis of efficacy, toxicity and prognostic factors. Bone Marrow Transplant 20, 451–458 (1997). https://doi.org/10.1038/sj.bmt.1700913
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1700913
Keywords
This article is cited by
-
CEAC (oral semustine, etoposide, cytarabine and cyclophosphamide) vs BEAM (carmustine, etoposide, cytarabine, and melphalan) conditioning regimen of autologous stem cell transplantation for diffuse large B-cell lymphoma: a post-hoc, propensity score-matched, cohort study in Chinese patients
Annals of Hematology (2024)
-
Toxicity Profile According to Etoposide and Cytarabine Dosing in Patients with Lymphoma Receiving Autologous Stem Cell Transplantation Following BEAM Conditioning
Annals of Hematology (2023)
-
Autologous Stem Cell Transplantation in Adult Hodgkin Lymphoma at a Tertiary Care Center in India: Analysis of Outcomes and Prognostic Factors
Indian Journal of Hematology and Blood Transfusion (2023)
-
Treosulfan plus fludarabine versus TEAM as conditioning treatment before autologous stem cell transplantation for B-cell Non-Hodgkin lymphoma
Bone Marrow Transplantation (2022)
-
Dose-adjusted high-dose chemotherapy with autologous stem cell transplantation for elderly (≥ 70 years old) lymphoma patients
Annals of Hematology (2022)