Abstract
Study design:
Case–control study.
Objectives:
(i) To describe the prevalence of sexual dysfunction in chronic low back pain (CLBP) patients, (ii) to compare the range of sexual function outcomes between patients with CLBP and healthy controls and (iii) to investigate which factors are associated with sexual function within the cohort of individuals with CLBP.
Setting:
Low back pain (LBP) clinic of Qazvin University of Medical Sciences, Qazvin, Iran.
Methods:
A total of 702 patients with CLBP and 888 healthy controls participated in the study. The Female Sexual Function Index (FSFI), International Index of Erectile Function (IIEF) and Premature Ejaculation Diagnostic Tool (PEDT) were used to evaluate sexual function. In addition, quality of life, anxiety, functional status and pain intensity were assessed in patients. Univariate and multiple linear regression analyses were performed for the identification of factors associated with sexual function.
Results:
The prevalence of sexual problems in female patients with CLBP was 71.1% (n=177) while the corresponding figure for healthy women was 36.8% (n=161). Erectile dysfunction was present in 59.5% of male patients and in 24.5% of healthy males. Higher sexual function in both male and female patients with CLBP were being younger, lower duration of back pain, lower BMI, higher education level, being unemployed, physically active shorter sick leave, lower level of pain intensity, lower disability, higher family income, lower levels of depressive and anxiety symptoms, and higher psychical functioning and mental functioning.
Conclusions:
CLBP patients report considerably higher prevalences of sexual problems compared with healthy controls. Sex therapy and sexual management should be added to routine care and treatment of patients with CLBP.
Similar content being viewed by others
Introduction
Chronic low back pain (CLBP) is considered an important and common medical health problem.1 CLBP is associated with deteriorated quality of life, restricted work-related activities and disability.2 Moreover, CLBP is considered one of most common reasons for seeking medical care.3 It has been estimated that up to 80% of people experience CLBP at some point in their lives.4 CLBP is also associated with an economic burden to society in terms of direct treatment costs as well as indirect costs (for example, through disability). In the United States, for example, CLBP-related costs have been estimated to be higher than $50 billion dollars a year.5 In Iran, as a developing country, the prevalence for CLBP ranges from 14.4 to 84.1% and has been reported to be the one of leading disease burdens.6
Sexuality is a multidimensional phenomenon and an integral part of human life and therefore considered an important part of quality of life.7 Previous studies have reported an association between CLBP and impaired sexual function and sexual health. A study by Berg et al., for example, showed that 84% out of 152 Swedish patients with CLBP reported impaired sexual functioning,8 and a more recent study found that CLBP was highly associated with both lower amounts of practiced sexual intercourse and a lower sexual quality of life.9 Despite evidence of the high prevalence of sexual dysfunction in patients with CLBP, there are only a few studies on sexual health in these patients,9 and to date no study has compared CLBP patients with matched healthy controls to ascertain the specific impact of CLBP on sexual function. In addition, no studies have used standardized, validated, gender-specific self-report questionnaires to screen patients for sexual problems but rather relied on self-constructed questionnaires. Therefore the aims of the present study were (i) to describe the prevalence of sexual dysfunction in CLBP patients, (ii) to compare the range of sexual function outcomes between patients with CLBP and healthy controls, (iii) to investigate which factors are associated with sexual function within the cohort of those with CLBP and (iv) to report on the differences in sexual functioning between men and women.
Materials and methods
Design
This study was approved by the ethical review committee at Qazvin University of Medical Sciences. Before participation, all patients provided verbal and written informed consent.
Patients
Two different samples of participants were included in this study. In the first sample, patients suffering from CLBP were recruited from an LBP clinic at the University Hospital of Qazvin (Shahid Rajaee Hospital, Qazvin), which is a referral center for neurological disorders in Qazvin province. Patients were eligible for inclusion if they were 18 years or older, sexually active for at least 6 months and had a confirmed diagnosis of CLBP (that is, persistent LBP with or without referred pain). Exclusion criteria were pregnancy, participation in a regular physical exercise program, having a history of spinal surgery, spinal deformities, LBP due to fractures, acute infections, suffering from cancer, cardiovascular diseases, hypertension, diabetes mellitus, endocrinological disorder, rheumatic diseases, and neurological and vestibular diseases, substance abuse (drugs and alcohol), use of psychiatric drugs (that is, hormone therapy, antidepressants, anxiolytics and neuroleptics) and suffering from cognitive impairment as assessed by the mini–mental state examination (MMSE: with scores of 23 or lower indicating the presence of cognitive impairment).
The second cohort was drawn from a community sample of people attending urban health centers. Family records from these centers were used to randomly select the healthy controls. In Iran, health care is provided by a nation-wide network consisting of urban health centers and running on a referral-based system. Each center covers around 12 000–15 000 people and retains vital information for all families within its coverage. For this study, five urban health centers were randomly selected out of 15 urban health centers. Individuals fulfilling the following criteria were contacted and asked about their interest in study participation: 18 years or older, sexually active for at least 6 months, not being pregnant, absence of musculoskeletal pain (that is, LBP), not having visited a physician, a chiropractor or a physiotherapist for back pain within the past 12 months and no signs of cognitive impairment (using the same assessment and criteria as in the CLBP cohort). Furthermore, to be included in the study, the healthy controls had to report.
Measures
Pain
Back pain intensity in the past week was measured on a 0–100 visual analog scale.10
Functional status
To assess the extent to which back or leg trouble has affected the ability to manage activities of everyday life, the 10-item Oswestry Disability Index (ODI) was used.11 In addition, the Roland–Morris Disability Questionnaire (RMDQ) was used to capture a patient’s functional status.
Hospital anxiety and depression scale (HADS)
For the assessment of anxiety and depression, the HADS consisting of two subscales including anxiety (seven items) and depression (seven items) was used. The HADS scored on a 4-item scale ranging from 0 (absence of symptoms) to 3 (maximum symptomatology). Each subscale scoring system ranges from 0 to 21 with higher scores representing more symptomatology.12
The short form-36
The short form-36 (SF-36) consists of 36 items with eight dimensions including physical function, role physical, bodily pain, general health, vitality, social function, role-function emotional and mental health and is used to capture an individual’s overall health status. It can also be summarized into two component scales: the Physical Component Scale (PCS) and the Mental Component Scale (MCS).13
Female sexual function index
Female sexual function was assessed using the female sexual function index (FSFI).14 The FSFI consists of 19 items that cover six subscales including sexual desire (two items), arousal (four items), lubrication (four items), orgasm (three items), satisfaction (three items) and pain (three items). The total score is obtained by adding the six domain scores and ranges from 2 to 36. A score ⩽26.55 is used to discriminate healthy from sexually dysfunctional women.15
International index of erectile function
The international index of erectile function (IIEF) is a brief self-report measure to assess male erectile dysfunction (ED). The measure consists of 15 items that form five subscales including erectile function (six items), orgasmic function (two items), sexual desire (two items), intercourse satisfaction (three items) and overall satisfaction (two items).16
Premature ejaculation diagnostic tool
The premature ejaculation diagnostic tool (PEDT) is a brief and multidimensional instrument for the diagnosis of premature ejaculation (PE).17
Statistical analysis
Chi-square test, Independent t-test and Mann–Whitney U-test were used for sample comparison. For comparison of the questionnaire subscale scores between samples (IIEF, PEDT, HADS and SF-36) analysis of covariance (ANCOVA)—adjusted for age, education and physical activity—was conducted. To control for multiple testing and therefore to balance the amount of type I and II errors, the Benjamini-Hochberg method for corrected P-values was used. For the identification of factors associated with sexual problems, a series of multiple regressions were conducted in both males and females with low back pain. First, univariate regressions were performed. The significant independent variables (that is, P<0.05) were then entered into the multiple linear regression models. All variables were treated continuously and were standardized to avoid multi-collinearity among variables in the regression models.
Results
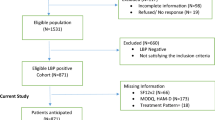
A total of 884 patients with low back pain and 1000 healthy controls were invited to participate in the study. Of 884 invited patients with low back pain, 84 patients did not meet the inclusion criteria and 98 patients declined to participate (54 males and 44 females; 12.25%) with 115 healthy controls (62 males and 53 females; 11.5%) also declining to take part in the study. No significant differences between study participants and non-participants in respect of age, educational status, accommodation, family income, work status or physical activity could be detected (data not shown).
Sample characteristics are shown in Table 1. The mean age of male CLBP patients was 40.1±11.9 years and 39.89±21.84 years for healthy controls. Female patients were slightly younger with a mean age of 38.9±11.2 years and a mean age of 39.35 ±17.0 years for healthy controls. The majority of participants (%) were city residents. Most of males in both groups had completed secondary schools (36.2 and 37.9%), whereas most women in both groups had completed primary schools (32.5 and 30.9%). In all, 60% of participants had monthly family income between 300 and 1000 $. Both male and female CLBP patients were more frequently sedentary compared with their healthy counterparts. None of the patients or healthy controls was undergoing sex therapy or sexual treatment during the course of the study.
No significant differences between the two samples could be detected for any of the demographic and lifestyle variables assessed, with the exception of physical activity and the frequency of sexual intercourse per month. Intercourse frequency was significantly lower in both men and women with CLBP compared with their healthy counterparts (Table 1).
Both male and female patients with LBP scored significantly lower in all quality of life subscales (as assessed by the SF-36) after applying the Benjamini-Hochberg correction (Table 2). Furthermore, the differences were more evident for role limitations due to physical health and physical component summary (Table 2).
The prevalence of sexual dysfunction (that is, FSFI⩽26.55) in female patients with LBP was 71.1% (n=177) while the corresponding figure for healthy women was 36.8% (n=161). In addition, women with LBP reported lower scores on all FSFI domains in comparison with healthy controls even after adjusting for age, education and physical activity (Table 3). Similarly, males suffering from LBP reported significantly lower scores on the IIEF compared with their healthy counterparts, also after adjusting for age, education and physical activity (Table 4). ED was present in 59.5% of patients and in 24.5% of healthy controls. The degree of dysfunction was scored mild, mild-to-moderate, moderate and severe in 17 (4.6.0%), 69 (18.6%), 89 (24.1%) and 45 (12.2%) of patients, respectively. In healthy men, 4.5% (n=19) had moderate or severe ED, 9.6% (n=41) had mild-to-moderate ED and 10.4% (n=44) had mild ED. No significant difference between two groups in terms of PE could be detected (as assessed by the PEDT) (Table 4).
Variables included in the multiple regression model for LBP women indicated that the model was able to explain 62.6% of the variance in FSFI scores (Table 5). In this model, younger age, lower duration of back pain, lower BMI, higher education, being employed, regular menstruation, physical activity, shorter sick leave, lower level of pain intensity, less disability as assessed by the ODI and RMDQ, higher family income, less depressive and anxiety symptoms, better psychological and mental functioning were associated with better sexual function (Table 5).
The multiple regression model used for LBP men with ED explained 57.2% of the total variance (Table 6). The main predictors of an increased erectile function were younger age, lower duration of back pain, lower BMI, higher education level, being unemployed, being physically active, shorter sick leave, lower level of pain intensity, lower disability as assessed by the ODI and RMDQ, higher family income, less depressive and anxiety symptoms, better psychological andand mental functioning.
Discussion
Despite the number of studies investigating sexual dysfunction among patients with CLBP being scarce, they consistently report that sexual problems and poor quality of life are common phenomena among these patients.2 No study to date has yet assessed risk factors for sexual problems in patients with CLBP. The aim of the study was to explore the impact of CLBP on sexual function and to investigate socio-demographic, psychological and clinical factors with sexual functioning in a sample of Iranian patients with CLBP.
In the present study, patients with CLBP reported lower health-related quality of life compared with healthy controls. Furthermore, significant associations were found between health-related quality of life and sexual functioning in both male and female patients with CLBP. Poor quality of life not only affects patient’s daily living but as a consequence also sexual functioning. The few investigating the impact of CLBP on sexual quality of life found consistent evidence for the detrimental effects that such a chronic condition can have on sexual quality of life and well-being.9
In accordance with these findings, we also report considerable high prevalences of sexual problems in our CLBP patient sample, with 71.1% of women with CLBP reporting any kind of sexual problem and 59.5 and 21.9% of men with CLPB reporting ED and PE, respectively. These prevalences were significantly higher compared with the matched healthy male and female controls. A study conducted on Moroccan patients with CLBP found similar rates of sexual problems, with 90% of women and 72% of men reporting some kind of sexual impairment.9 Ambler et al. reported similar burden rates for sexual problems with a similar high prevalence of sexual problems of 73% in patients with chronic pain.18 Another study reported 46% for sexual problem in CLBP patients.19 The novel aspect of this study was to use gender-specific tools to assess sexual functioning as well as comparing rates between CLBP patients and healthy controls. Research has shown that women with specific physiological conditions such as menstruation, gestation and lactation have different sexual needs.20 Research has already shown that women with concerns about pain may wish to avoid further perceived pain through sexual activities.18
Clearly this study, as with other previous studies, has shown the considerable detrimental association between CLBP and sexual function. As mentioned within the introduction, sexual function (of sexually active adults) is an important aspect on the quality of life for individuals. The potential disruption of this quality for individuals with pain may compound the burden of other psychosocial factors related to poor patient prognosis (for example, depression, anxiety and fear avoidance). However, this issue may well have broader social effects on the individual with pain. There is an emerging growth of research that shows the inclusion of partners within treatment paradigms for chronic pain patients can be beneficial.21 One key factor in having a supportive partner is the level of intimacy and empathy shown,22 and it could be argued that the sexual union between partners, or lack of it as appears the case for those with CLBP, could be an important determinant of this social influence. Clinicians do routinely assess the impact CLBP has on their patient; our research suggests inquiry on the possible disruption of sexual activity due to CLBP may be a worthwhile additional question to highlight a potentially important psychosocial influence.
In conclusion patients with CLPB are at a higher risk of reporting sexual problems. As a result, older patients, higher BMI, lower educational level, lower family income, poor functional status, being physically inactive, being unemployed, irregular menstruation, prolonged duration of disease and sick leave, higher levels of depression and anxiety and poor quality of life have been found to be associated with lower female sexual function in female patients with CLBP. In contrast, older patients, higher BMI, lower educational level, lower family income, poor functional status, being physically inactive, being retired or employed, prolonged duration of disease and sick leave, higher levels of depression and anxiety and poor quality of life put males at risk of sexual dysfunction.
Clinicians may benefit from inquiring about the impact of back pain on the sexual functioning of their patients. Where the patient clearly indicates the occurrence of such impact the clinician may offer advice on the reduction of this impact in addition to the primary goal of pain management. For example, advice could be given on body positioning during sexual activity to avoid pain, and advice on increasing exercise to reduce fatigue. Further advice could be given to help the patient to adjust and accommodate if their pain is likely to persist, a good example is the ‘Good-Enough Sex’ model that can help patients to adjust physically and mentally to changes in sexual functioning.23
Data archiving
There were no data to deposit.
References
Picavet HS, Schouten JS . Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC(3)-study. Pain 2003; 102: 167–178.
Huijnen IP, Kindermans HP, Seelen HA, Peters ML, Smeets RJ, Serroyen J et al. Effects of self-discrepancies on activity-related behaviour: explaining disability and quality of life in patients with chronic low back pain. Pain 2011; 152: 2165–2172.
Jordan KP, Kadam UT, Hayward R, Porcheret M, Young C, Croft P . Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskelet Disord 2010; 11: 144–163.
Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ . Outcome of low back pain in general practice: a prospective study. BMJ 1998; 316: 1356–1359.
National Institute of Neurological Disorders and Stroke. Low Back Pain Fact Sheet. National Institutes of Health Publication number 03-5161. Washington DC: National Institute of Neurological Disorders and Stroke. 2003.
Mousavi SJ, Akbari ME, Mehdian H, Mobini B, Montazeri A, Akbarnia B et al. Low back pain in Iran: a growing need to adapt and implement evidence-based practice in developing countries. Spine 2011; 36: E638–E646.
Stock SR, Cole DC, Tugwell P, Streiner D . Review of applicability of existing functional status measures to the study of workers with musculoskeletal disorders of the neck and upper limb. Am J Ind Med 1996; 29: 679–688.
Berg S, Fritzell P, Tropp H . Sex life and sexual function in men and women before and after total disc replacement compared with posterior lumbar fusion. Spine J 2009; 9: 987–994.
Bahouq H, Fadoua A, Hanan R, Ihsane H, Najia HH . Profile of sexuality in Moroccan chronic low back pain patients. BMC Musculoskelet Disord 2013; 14: 63–68.
Haefeli M, Elfering A . Pain assessment. Eur Spine J 2006; 15 (Suppl 1): S17–S24.
Mousavi SJ, Parnianpour M, Mehdian H, Montazeri A, Mobini B . The Oswestry Disability Index, the Roland-Morris Disability Questionnaire, and the Quebec Back Pain Disability Scale: translation and validation studies of the Iranian versions. Spine 2006; 31: E454–E459.
Zigmond AS, Snaith RP . The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370.
Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B . The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Qual Life Res 2005; 14: 875–882.
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R et al. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 2000; 26: 191–208.
Fakhri A, Pakpour AH, Burri A, Morshedi H, Zeidi IM . The Female Sexual Function Index: translation and validation of an Iranian version. J Sex Med 2012; 9: 514–523.
Pakpour AH, Zeidi IM, Yekaninejad MS, Burri A . Validation of a translated and culturally adapted Iranian version of the International Index of Erectile Function (IIEF-15). J Sex Marital Ther, (e-pub ahead of print 10 October 2013; doi:10.1080/0092623x.2013.788110).
Pakpour AH, Yekaninejad MS, Nikoobakht MR, Burri A, Fridlund B . Psychometric Properties of the Iranian version of the Premature Ejaculation Diagnostic Tool (PEDT). Sex Med, (in press).
Ambler N, Williams AC, Hill P, Gunary R, Cratchley G . Sexual difficulties of chronic pain patients. Clin J Pain 2001; 17: 138–145.
Duquesnoy B, Allaert FA, Verdoncq B . Psychosocial and occupational impact of chronic low back pain. Rev Rhum Engl Ed 1998; 65: 33–40.
Leiblum RS . Reconsidering gender differences in sexual desire: An update. Sex Relation Ther 2002; 17: 57–68.
Abbasi M, Dehghani M, Keefe FJ, Jafari H, Behtash H, Shams J . Spouse-assisted training in pain coping skills and the outcome of multidisciplinary pain management for chronic low back pain treatment: a 1-year randomized controlled trial. Eur J Pain 2012; 16: 1033–1043.
Campbell P, Jordan KP, Dunn KM . The role of relationship quality and perceived partner responses with pain and disability in those with back pain. Pain Med 2012; 13: 204–214.
Metza ME, McCarthy BW . The ‘Good-Enough Sex’ model for couple sexual satisfaction. Sex Relation Ther 2007; 22: 351–362.
Acknowledgements
We thank Qazvin University of Medical Sciences for support to conduct the study. We also thank all the patients and nurses as well as Mrs Mahdieh Pakpour who kindly helped us to collect data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nikoobakht, M., Fraidouni, N., Yaghoubidoust, M. et al. Sexual function and associated factors in Iranian patients with chronic low back pain. Spinal Cord 52, 307–312 (2014). https://doi.org/10.1038/sc.2013.151
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.151
Keywords
This article is cited by
-
Posterior lumbar fusion surgery doesn’t change sexual activities in patients with lumbar degenerative disease: an observational study
BMC Musculoskeletal Disorders (2023)
-
The correlation between sexual dysfunction and intimate partner violence in young women during pregnancy
BMC International Health and Human Rights (2020)
-
Association between low back pain and various everyday performances
Wiener klinische Wochenschrift (2019)
-
Sexual Functioning and Selected Clinical and Psychosocial Factors Among Individuals with Chronic Non-specific Low Back Pain in Ibadan, Nigeria
Sexuality and Disability (2018)
-
Discussing sexual health in spinal care
European Spine Journal (2016)