Abstract
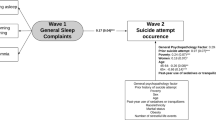
In recent years, there has been a growing interest in understanding the relationship between sleep and suicide. Although sleep disturbances are commonly cited as critical risk factors for suicidal thoughts and behaviours, it is unclear to what degree sleep disturbances confer risk for suicide. The aim of this meta-analysis was to clarify the extent to which sleep disturbances serve as risk factors (i.e., longitudinal correlates) for suicidal thoughts and behaviours. Our analyses included 156 total effects drawn from 42 studies published between 1982 and 2019. We used a random effects model to analyse the overall effects of sleep disturbances on suicidal ideation, attempts, and death. We additionally explored potential moderators of these associations. Our results indicated that sleep disturbances are statistically significant, yet weak, risk factors for suicidal thoughts and behaviours. The strongest associations were found for insomnia, which significantly predicted suicide ideation (OR 2.10 [95% CI 1.83–2.41]), and nightmares, which significantly predicted suicide attempt (OR 1.81 [95% CI 1.12–2.92]). Given the low base rate of suicidal behaviours, our findings raise questions about the practicality of relying on sleep disturbances as warning signs for imminent suicide risk. Future research is necessary to uncover the causal mechanisms underlying the relationship between sleep disturbances and suicide.
Similar content being viewed by others
Introduction
Sleep is fundamental to survival1,2,3. A single poor night of sleep can result in mood changes4, worsening executive function5, and memory impairment6. Chronic sleep disturbances have been linked to increased risk for depression7, bipolar disorder8, and anxiety9. A growing body of research has also uncovered a link between sleep disturbances and suicide.
The notion that sleep disturbances contribute to suicide risk is gaining momentum. Sleep disturbance is commonly considered a warning sign for suicide10, and associations between sleep disturbances and suicidal thoughts and behaviours are consistently detected11,12,13,14,15. These associations are notable for several reasons. First, sleep problems are highly prevalent16,17,18. Approximately one-third of adults experience insomnia symptoms, with 6–10% meeting criteria for insomnia disorder19. To accurately assess risk, it is critical to determine the magnitude of the association between sleep disturbances and suicide. Second, sleep disturbances, unlike many other suicide risk factors, are modifiable. Sleep is already an intervention target in many mainstream therapeutic approaches, and treatments for sleep disturbances have been firmly established20,21. If sleep disturbances are reliably shown to be risk factors for suicide, sleep interventions could be leveraged as suicidality interventions. Third, sleep is an intervention target with relatively low stigma22, especially compared to suicidality23. Addressing suicidality by targeting sleep may increase the likelihood that at-risk individuals will seek treatment.
Until recently, research on the relationship between sleep and suicide has been predominantly cross-sectional24. Because risk factors must precede outcomes of interest25, cross-sectional evidence is insufficient to conclude that disturbed sleep is a risk factor for suicide. While longitudinal studies are filling this critical gap in the literature, results are mixed. Some studies have found large effects of sleep disturbances on suicide risk26,27,28, but others have found smaller29,30,31 or nonsignificant effects32,33,34. These discrepancies raise questions about the extent to which sleep disturbances confer risk for suicidal thoughts and behaviours. Moreover, these studies cannot provide information about causal mechanisms. Although risk factors are typically assumed to play a causal role in the outcome of interest, other variables may be responsible for observed longitudinal associations. For sleep disturbances to be considered causal risk factors for suicide, studies must examine whether manipulating sleep leads to systematic differences in suicide-related outcomes.
It is also unclear whether certain sleep disturbances are stronger predictors of suicidal thoughts and behaviours. Many studies focus on insomnia 32,35,36; others examine nightmares37, daytime sleepiness33, total sleep time38, and nonspecific or undifferentiated categories like “sleep problems”30. Even among studies that examine the same category of sleep disturbance, effect sizes range widely. Perhaps as a result of these inconsistent findings, the existing clinical guidelines are relatively nonspecific. Clinicians must rely on indicators like “unable to sleep” or “sleeping all the time” as warning signs for suicidal behaviours10. Given the seriousness of managing suicide risk, it is critical that clinical guidelines are clear so clinicians can make informed decisions about how to maintain their patients’ safety.
Measurement of sleep disturbances also varies across studies. Some studies use self-report scales29,39; others use clinical interviews40, and recent studies have begun to evaluate objective sleep parameters using actigraphy41 and polysomnography42. While novel methodologies refine the measurement of sleep disturbances, the comparative utility of objective versus subjective measures is unclear. Some evidence suggests that objective and subjective sleep measures are highly correlated43, whereas other studies find that individuals who present with subjective sleep complaints may not demonstrate objective evidence of disturbed sleep44. Therefore, their associations with suicide risk may be discrepant. Studies examining the relationship between objective sleep measures and suicide risk remain rare, but recent evidence indicates that both subjective and objective measures significantly predict risk, with similar effect sizes41,42. Given the cost and inconvenience of continuous sleep monitoring45, scalable subjective self-report measures may be preferable for routine monitoring of sleep disturbances.
Follow-up intervals also vary, ranging from one day46 to ten years29 for suicidal ideation, one month47 to eight years33 for suicide attempt, and one week48 to up to 50 years49 for suicide death. As clinicians are often tasked with identifying risk in the very short term, the most useful risk factors would accurately indicate imminent risk. It is critical to examine whether the effect of sleep disturbances on suicide risk varies with respect to time interval.
In short, the existing literature raises questions about the extent to which sleep disturbances serve as risk factors for future suicidal thoughts and behaviours. Although some have endeavoured to provide quantitative summaries of this literature50, these efforts have focused predominately on synthesizing cross-sectional research. Accordingly, it remains unclear whether sleep disturbances confer risk for suicidal thoughts and behaviours or whether they simply represent a correlate of those experiences. Advancing knowledge toward this end is critical to improving suicide prediction and prevention efforts.
The objective of this study is to substantively advance our understanding of the link between sleep disturbance and suicidal thoughts and behaviours. Using meta-analytic methods, the present study advances our knowledge in five ways. First, we will summarize the longitudinal literature on the relationship between sleep disturbances and suicide. Second, we will meta-analyse categories of sleep disturbances to determine whether certain categories (e.g., insomnia, nightmares, sleep quality) are stronger risk factors for suicide-related outcomes. Third, we will examine whether effects vary across outcomes (i.e., suicide ideation, attempts, or death). Fourth, we will evaluate the influence of potential moderators including study publication date, follow-up length, sample severity, and sleep measure type. Given recent methodological advances in the measurement of acute sleep disturbances, we hypothesized that more recent studies, particularly those which objectively measure sleep disturbances, would provide the most robust prediction. Although relatively little research has examined short-term prediction of suicide51, recent evidence indicates that shorter follow-up lengths may improve predictive accuracy52; therefore, we expected to detect stronger effects over shorter follow-up periods. Fifth, we will evaluate whether sleep disturbances serve as clinically useful predictors of suicidal thoughts and behaviours by contextualizing our findings in terms of the absolute risk of suicide-related outcomes.
Methods
Literature search
Our literature search was conducted as part of a larger meta-analytic effort53. Using identical methods and search terms, we updated the comprehensive literature search conducted by Franklin and colleagues53 to include articles published through October 31, 2019. Databases used were PubMed, PsycINFO, and Google Scholar. Search terms included variants of the words “longitudinal” (i.e., “longitudinal,” “longitudinally,” “predict,” “predicts,” “prospective,” “prospectively,” “future,” “later,”) and “suicide” (i.e., “self-injury,” “self-injurious,” “self-injurer,” “suicide,” “suicidal,” “suicidality,” “self-harm,” “NSSI,” “DSH,” “self-cutting,” “self-burning,” “self-poisoning”). Because many studies include measures of sleep disturbances even when they are not central to the study (e.g., a study about the effects of mood disorders on suicide may include information about insomnia), we intentionally did not constrain our search based on sleep-specific key words. We reasoned that this more comprehensive approach accordingly increased the likelihood that all potentially relevant articles would be captured.
Inclusion and exclusion criteria
All articles were required to include at least one longitudinal analysis in which a sleep-related variable (i.e., any measure designed to assess sleep or sleep-related symptoms) predicted suicide ideation, attempt, or death. We focused on these outcomes for two reasons. First, we were interested in effects on suicidal thoughts and behaviours, which are self-directed and involve a nonzero intent to die. This excludes behaviours unrelated to suicidality, such as nonsuicidal self-injury, or mixed terms capturing both suicidal and nonsuicidal behaviours, such as deliberate self-harm. Second, we were interested in understanding specific effects on discrete suicide-related outcomes. Therefore, studies that collapsed these variables into a single measure (e.g., subsuming suicidal ideation and attempts under a “suicidality” item) were excluded. All articles were required to be peer-reviewed published articles with an English language version available. We chose to include only published studies because we were interested in publicly available data that clinicians may use to make decisions.
Treatment studies were excluded, as treatment effects may influence risk factor effects. Systematic reviews and meta-analyses were also excluded. Studies which did not provide necessary statistical information were also excluded (i.e., insufficient data to calculate an odds ratio and its variance).
Study selection
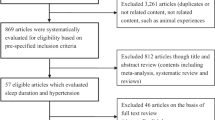
Our initial search yielded 5,091 unique articles published between 1965 and 2019. We screened in 743 papers for a full-text review. We retained 42 studies for our final analyses based on our inclusion criteria. Across studies, there were 156 unique effect sizes (see Fig. 1 for PRISMA flowchart; see Supplementary Materials for a full reference list of included studies).
PRISMA flowchart84.
Data extraction and coding
The following data were extracted from each study: author, publication year, follow-up length in months, sample size, sample type (i.e., general population, clinical population, or participants recruited for a history of self-injurious or suicidal behaviours), sample age (i.e., “child/adolescent” if the study included only participants under 18 years of age at the start of the study, “mixed” if the study included both participants under and over 18 at the start of the study, or “adult” if all participants were over 18 years old), predictor (i.e., type of sleep disturbance), outcome (i.e., ideation, attempt, or death), sleep measure type (i.e., self-report, interview, actigraphy, or polysomnography), and relevant statistics. Any statistical test in which a sleep-related variable predicted suicide ideation, attempt, or death was retained as a “prediction case.”
Predictor variables varied across studies. To improve interpretability, we coded specific predictor variables into secondary broad predictor categories; see Supplementary Materials for a complete list. Initial codes for each article were determined by the first author. Each code was subsequently examined by two additional authors (CPB and KPL). All discrepancies were discussed until consensus and resolved. Outcomes were coded as suicide ideation, attempt, or death. One study32 included interrupted and aborted suicide attempts; these were coded as suicide attempts. Our pattern of findings remained unchanged when this study was excluded from analyses.
Meta-analyses often code for study quality, especially when the included studies contain a high degree of methodological variability. Compared to other meta-analyses, however, the present set of studies was relatively uniform, as they all shared a common core design (i.e., longitudinal prediction of a discrete suicide-relevant outcome). Because there are no objective criteria to assess study quality in this particular literature, we conducted moderator analyses of methodological differences (e.g., length of follow-up, predictor type, sample type, etc.) to examine the impact of how certain methodological differences may influence risk factor magnitude. This approach was consistent with the methods used in prior meta-analyses of suicide risk factor research53,54,55.
Statistical analyses
All analyses were conducted using R56. Meta-analytic procedures were conducted using the metafor package57. We used odds ratios, which represent the odds of an event in one group compared to another, as our effect sizes. When odds ratios were not available, they were calculated from given data and summary statistics (e.g., 2 × 2 contingency tables, independent group means, risk ratios). If insufficient data were reported to compute an odds ratio and its variance (e.g., beta weights with no additional information, hazard ratios), that prediction case was excluded.
We used random effects models for all meta-analyses. Random effects models do not assume that a single, true effect exists, but that there will be a distribution of effects across studies. Due to the variability in predictors, outcomes, populations, and methodology, significant between-study heterogeneity was expected. Random effects models account for heterogeneity by relying on unconditional variance, which takes into account both sample size and variance between studies and weights effect sizes accordingly. Between-study heterogeneity was quantified using I2 tests. To improve the reliability of obtained estimates, only models including at least three effect sizes were run.
Publication bias was examined in several ways. We visually inspected funnel plots, which tend to be asymmetrical when publication bias is present and symmetrical when it is absent. Because visual inspection can be subjective, we also calculated Egger’s regression test as an objective index of funnel plot symmetry and used Duval and Tweedie’s trim and fill method to determine how many studies would be needed to make the funnel plot symmetrical. Classic and Orwin’s failsafe N analyses were conducted to estimate the robustness of observed effects.
Moderator analyses were conducted through a series of metaregressions using a random-effects model with unrestricted maximum likelihood estimation. Moderators included publication date, follow-up length, sample severity, and sleep measure type.
Results
Descriptive summary
Publication dates ranged from 1982 to 2019. The number of longitudinal studies examining the relationship between sleep disturbances and suicide has increased over time; most studies (N = 22; 52.38%) were published between 2015 and 2019 (Fig. 2). Suicide ideation was the most common outcome (k = 85; 54.49%), followed by attempt (k = 39; 25%) and death (k = 32; 20.51%).
Nearly half of prediction cases (k = 75; 48.07%) were drawn from community samples; 19.23% (k = 30) were drawn from clinical samples, and 32.69% (k = 51) were drawn from samples recruited for a history of self-injurious thoughts and behaviours. Most samples comprised only adults (k = 106; 67.95%); 29.49% of samples included only participants under 18 at the start of the study, and 2.56% (k = 4) included both participants under and over 18 at the start of the study.
Follow-up lengths ranged from 1 day to 50 years, with an average of 61.31 months (SD = 100.37, Mdn = 12). The follow-up lengths for suicide death cases (M = 197.40 months, range = 0.25–600, SD = 148.04, Mdn = 132) were longer on average than those for ideation (M = 23.61 months, range = 0.03–120, SD = 34.47, Mdn = 12) or attempt (M = 31.60 months, range = 0.03–100, SD = 30.44, Mdn = 12).
Insomnia was the most common predictor (k = 55; 35.26%), followed by unspecified “sleep problems” (k = 27; 17.31%), sleep duration (k = 16; 10.26%), and nightmares (k = 13; 8.33%). The majority of cases (k = 110; 70.51%) measured sleep disturbances via self-report, with the remainder using interviews (k = 29; 18.59%), actigraphy (k = 10; 6.41%), or polysomnography (k = 7; 4.49%).
Overall prediction and publication bias
Overall prediction estimates reflect the pooled effects of all predictors on the outcome of interest. Odds ratio analyses included 156 prediction cases. The overall weighted odds ratio for all outcomes was 1.59 (95% CI 1.46–1.73). Between-study heterogeneity was high (I2 = 83.40%). See Table 1 for all random-effects results. Significant evidence of publication bias was not detected (Table 2).
Suicidal ideation
Odds ratio analyses for suicidal ideation included 84 prediction cases. Heterogeneity was high between studies (I2 = 83.91%). The overall weighted odds ratio was 1.73 (95% CI 1.54–1.94). While failsafe N analyses indicated that this was a robust effect, evidence of publication bias was detected via visual inspection of the funnel plot and Egger’s test of the intercept (Fig. 3a; Table 2).
Suicide attempt
Odds ratio analyses for suicide attempt included 36 prediction cases. The overall weighted odds ratio was 1.54 (95% CI 1.32–1.81). Between-study heterogeneity was high (I2 = 83.16%). While visual inspection of the funnel plot indicated possible publication bias, significant evidence for publication bias was not detected via Egger’s test of the intercept, and failsafe N analyses indicated this was a robust effect (Fig. 3b; Table 2).
Suicide death
Odds ratio analyses for suicide death included 32 prediction cases. The overall weighted odds ratio was 1.33 (95% CI 1.11–1.60). Between-study heterogeneity was high (I2 = 73.94%). Although visual inspection of the funnel plot indicated possible publication bias, no significant evidence for publication bias was detected via Egger’s test of the intercept, and failsafe N analyses indicated this was a robust effect (Fig. 3c; Table 2).
Prediction by risk factor category
Insomnia
Insomnia significantly predicted suicidal ideation (OR 2.10 [95% CI 1.83–2.41], k = 31). Point estimates were smaller predicting suicide attempt (OR 1.78 [95% CI 1.38–2.29], k = 16) and suicide death (OR 1.54 [95% CI 1.04–2.29], k = 8).
Nightmares
Nightmares significantly predicted suicide attempt (OR 1.81 [95% CI 1.12–2.92], k = 5), but not suicide ideation (OR 1.08 [95% CI 0.61–1.91], k = 4) or death (OR 1.31 [95% CI 0.83–2.06], k = 4).
Sleep disturbances
Sleep disturbances did not significantly predict suicide ideation (OR 1.61 [95% CI 0.60–2.69], k = 6) or attempt (OR 1.85 [95% CI 0.98–3.48], k = 3). An insufficient number of cases were available to examine effects on suicide death.
Sleep duration
Sleep duration did not significantly predict suicide ideation (OR 0.95 [95% CI 0.70–1.29], k = 12), or attempt (OR 1.12 [95% CI 0.75–1.68], k = 4). An insufficient number of cases were available to examine effects on suicide death.
Sleep efficiency
Sleep efficiency did not significantly predict suicidal ideation (OR 1.26 [95% CI 0.56–2.81], k = 4). An insufficient number of cases were available to examine effects on suicide attempt or death.
Sleep problems
Sleep problems significantly predicted suicidal ideation (OR 1.80 [95% CI 1.30–2.50], k = 9). Effects were not significant for suicide death (OR 1.27 [95% CI 0.97–1.66], k = 16). An insufficient number of cases were available to examine effects on suicide attempt.
Sleep quality
Sleep quality significantly predicted suicidal ideation (OR 1.74 [95% CI 1.13–2.67], k = 6). Effects were not significant for suicide attempt (OR 1.35 [95% CI 0.84–2.15], k = 3). An insufficient number of cases were available to examine effects on suicide death.
Sleep-onset latency
Sleep-onset latency did not significantly predict suicidal ideation (OR 1.34 [95% CI 0.75–2.42], k = 6). An insufficient number of cases were available to examine effects on suicide attempt or death.
Tiredness
Tiredness did not significantly predict suicidal ideation (OR 1.81 [95% CI 1.00–3.27], k = 5). An insufficient number of cases were available to examine effects on suicide attempt or death.
Moderator analyses
We report metaregression results in terms of QM, the model sum of squares, which is a test of whether any of the regression coefficients in the model are significantly different from zero.
Publication date
Metaregression results indicated no significant effects of publication date on suicide ideation (QM [df = 2] = 0.31, p = 0.85), attempt (QM[df = 2] = 1.15, p = 0.56), or death (QM[df = 5] = 1.23, p = 0.94), indicating that effect sizes have remained stable over time.
Follow-up length
There was a significant effect of follow-up length for suicide ideation (QM[df = 5] = 160.62, p < 0.0001), attempt (QM[df = 5] = 39.71, p < 0.0001), and death (QM[df = 5] = 13.29, p = 0.02). Effects were strongest when the follow-up length was 6 months or less for all outcomes (ideation OR 2.30 [95% CI 2.00–2.65]; attempt OR 2.48 [95% CI 1.33–4.62]; death OR 2.19 [95% CI 1.08–4.43]).
Sample severity
Moderation analyses revealed a significant effect of sample severity on suicide ideation (QM[df = 2] = 21.61, p < 0.001), but not attempt (QM[df = 2] = 0.20, p = 0.90) or death (QM[df = 2] = 2.65, p = 0.27). Predicting ideation, effects were slightly stronger in community samples (OR 1.52 [95% CI 1.30–1.79]) and samples recruited for a history of self-injurious thoughts and behaviours (OR 1.45 [95% CI 1.17–1.80]) compared to other clinical populations (OR 0.78 [95% CI 0.57–1.05]).
Sleep measure type
Metaregression results indicated no significant effects of sleep measure type (i.e., self-report, interview, actigraphy, or polysomnography) on suicide ideation (QM[df = 3] = 4.55, p = 0.21), attempt (QM[df = 2] = 3.62, p = 0.16), or death (QM[df = 1] = 0.25, p = 0.62). We also conducted post-hoc moderator analysis using each specific measure (e.g., specific self-report measures, interviews, and actigraphy/polysomnography measures) as a moderator. Our analyses revealed a significant effect of specific measure for suicide ideation (QM[df = 13 ] = 54.50 , p < 0.001), but not attempt (QM[df = 10] = 16.73, p = 0.08), or death (QM[df = 12] = 11.88, p = 0. 46). For suicide ideation, effects were strongest when sleep disturbances were measured with the Insomnia Severity Index (OR = 1.55 [95% CI 1.07–2.23]) and the Adolescent Health Questionnaire (OR 1.63 [95% CI 1.10–2.42]).
Discussion
Our findings indicate that sleep disturbances are statistically significant predictors of suicide ideation, attempt, and death. However, these effects were weak, at least as examined within the methodological constraints of the literature. Our results are consistent with a growing body of evidence which demonstrates that most commonly cited risk factors only weakly predict suicide53,58,59. Odds ratios for each outcome ranged from 1.33 to 1.73, and effects were consistent regardless of study publication date and type of sleep measure used (i.e., self-report, clinical interview, actigraphy, or polysomnography).
The literature on the longitudinal relationship between sleep and suicide has grown exponentially in recent years. Because the most recent meta-analysis of this literature was published nearly a decade ago and focused primarily on cross-sectional studies, the present study represents a critical step toward advancing our knowledge of the extent to which disturbed sleep confers risk for future suicidal thoughts and behaviours. Indeed, over half of the studies we uncovered in our review of the literature were published within the last 5 years (Fig. 2). Results indicated, however, that this increase in research has not corresponded with improved predictive accuracy, though it may have contributed to improved reliability of detected effects. We found that most studies examined the effects of disturbed sleep on suicide ideation, rather than suicidal behaviours (i.e., attempts or death). Moreover, very few studies examined proximal risk; the average follow-up length was over 5 years, and follow-up intervals were much longer on average for suicidal behaviours compared to suicidal ideation.
Effects varied depending on follow-up length, with slightly stronger effects observed over shorter follow-up periods (≤ 6 months); however, these effects remained weak. Prior evidence is mixed regarding the effects of follow-up length on risk factor strength. In a meta-analysis of hundreds of risk factors, no consistent patterns of predictive ability over different follow-up intervals were detected53. Given the fluctuating nature of sleep disturbances60,61 and suicidality62,63, it is possible that short-term follow-up windows yielded slightly stronger effects by producing more reliable measurement. Although these results indicate that it is sensible to focus on short-term prediction, studies with brief follow-up periods remain rare. Because suicide is fortunately a low base-rate event, it is difficult to detect statistically meaningful effects over brief intervals. Recent studies have used novel techniques to overcome this challenge, such as leveraging large, severe samples recruited online64,65. Online studies yield faster recruitment than in-person data collection and produce comparable results to in-person studies66,67. These methods may provide a fruitful path for future research.
Slightly stronger effects were detected in less severe samples. These findings are likely a methodological artefact. When studies rely on homogenous samples, the range of severity is restricted, making it difficult to detect significant differences from the reference group; in contrast, samples with high levels of heterogeneity capture both extremes of severity, making it easier to detect significant effects. Studies in clinical and self-injurious samples are also likely to control for additional risk factors, which may further reduce effect sizes. Other meta-analyses have found similar moderating effects of sample severity54,58. Despite statistically significant moderation, effects detected in less severe samples remained weak.
In addition to overall prediction, we examined the effects of specific sleep disturbances. The strongest effects were found for insomnia, which significantly predicted suicide ideation (OR 2.10 [95% CI 1.83–2.41]), and nightmares, which significantly predicted suicide attempts (OR 1.81 [95% CI 1.12–2.92]). Only insomnia significantly predicted suicide death (OR 1.54 [95% CI 1.04–2.29]). This pattern of findings is consistent with other meta-analytic evidence that the strongest predictive effects are typically observed for suicide ideation, followed by attempt and death (e.g., anxiety symptoms58; depression and hopelessness54); however, the evidence reliably demonstrates that even the strongest predictors are weak in absolute terms53. The majority of effects (76%) were nonsignificant, and for several predictors, there were too few cases to provide reliable estimates. Although additional cases may have allowed us to detect more reliable effects, it is unlikely that stronger effects would be detected, as overall estimates all achieved statistical significance yet remained weak.
This meta-analysis cannot provide direct insight into the relationship between sleep disturbances and suicide risk; it can only reflect the value of this relationship as examined within the methodological constraints of the literature. It is therefore important to consider limitations when interpreting these findings. First, although self-report was the most common way to assess sleep disturbances, nearly every study relied on different measures. The exceptions were three studies32,65,68 which used the Insomnia Severity Index (ISI), and two studies35,69 which used the Women’s Health Initiative Insomnia Rating Scale (WHIIRS). Other validated self-report measures included the Pittsburgh Sleep Quality Index28,42, the Adolescent Health Questionnaire33, the Youth Self Report questionnaire70, the Beck Depression Inventory47, and the Uppsala Sleep Inventory71. Multiple studies relied on single-item measures rather than validated questionnaires30,72,73. Although our moderation analyses did not reveal a significant effect of sleep measure type (i.e., self-report, interview, actigraphy, or polysomnography) on effect size, our post-hoc moderator analyses revealed that specific measures were statistically significant moderators for suicide ideation, with the strongest effects observed for the Insomnia Severity Index and the Adolescent Health Questionnaire. However, these effects remained weak (ORs 1.55 and 1.63, respectively). These two measures accounted for the largest proportion of effect sizes in our analyses; therefore, the significant moderation effect may reflect improved reliability as a consequence of their frequency of use. No significant effects were detected for suicide attempt or death.
Second, several sleep disorders were not represented in the existing literature, including sleep apnoea, restless leg syndrome, and narcolepsy. In fact, prior diagnoses of sleep disorders were sometimes used as exclusion criteria for study participation (e.g.,42). Although sleep disturbances may indicate the presence of a sleep disorder, it remains unknown whether their associations with suicide risk are distinct. Due to the lack of studies examining the longitudinal relationship between diagnosed sleep disorders and suicidal thoughts and behaviours, determining the extent to which they may confer risk for suicide is beyond the scope of the present meta-analysis; however, given prior meta-analytic evidence that diagnoses of particular disorders are limited in their ability to accurately predict suicide53, we reason that our pattern of results would have been comparable even with the addition of studies examining these disorders. Nevertheless, this represents an important area for future research.
Third, assessment windows varied substantially. Whereas the BDI assesses sleep disturbances over the last week, the ISI assesses the last two weeks, and the WHIIRS assesses the last four weeks. Some studies assessed sleep disturbances over the last year72,74. Consistent with a priori hypotheses, our moderator analyses demonstrated that effects were strongest over shorter intervals. Although relying on retrospective self-reported symptoms is common, doing so over longer periods of time is likely to be less valid and reliable than short-term assessment, as these methods may be affected by recall biases, especially for symptoms that occurred less recently75. These measurement issues may have contributed to the detection of less robust effects; however, the strongest short-term effect we detected (i.e., pooled effect of all sleep disturbances on suicide attempt over a follow-up period of 0–6 months) was still weak (OR = 2.48).
Fourth, although objective sleep measures address several limitations of subjective measures76, only three studies 41,42,46 used these methods, accounting for approximately 10% of effect sizes. It is possible that our failure to detect a significant effect of sleep measure type was due to the small number of studies using objective measures that fit our inclusion criteria. The included studies may not represent the effects of objective measures in general; sleep disturbances may emerge as stronger risk factors as additional studies are published. Because the effects of univariate predictors of self-injurious and suicidal behaviours are weak53,77, however, we reason that our results would be similar even with the inclusion of additional studies.
Our findings must also be evaluated with regards to clinical utility. According to the Centers for Disease Control and Prevention, the rate of suicide death in the United States is approximately 14.5 per 100,000. The strongest predictor of suicide death in this study was insomnia, which approximately doubles the risk of suicide death (OR 2.10). This increases the odds to 0.0003, representing a marginal improvement in predictive ability. Although sleep disturbances play a statistically significant role in predicting suicide, these results raise questions about the usefulness of designating sleep disturbances as suicide “warning signs,” at least when considered in isolation.
It is possible that methodological constraints account for the weak prediction estimates found in this study. However, our moderator analyses indicate this is unlikely. Even statistically significant influences on effects due to variations in follow-up length, sleep measure type, and sample severity did not meaningfully improve prediction. We accordingly reason that the most significant methodological issue is the focus on univariate-level prediction.
Our first recommendation for future research is to advance beyond examining the effects of sleep disturbances in isolation, and instead consider their function in the context of complex associations with other biopsychosocial factors. Studies which focus on individual sleep disturbances as predictors of suicide implicitly assume that this relationship is simple. Simple theories are cognitively manageable, but they stand in contrast to evidence demonstrating that it may be necessary to consider many biopsychosocial factors, combined in complex ways, to accurately predict suicide65,78,79. Results of the present study are consistent with complexity. Whereas no individual sleep disturbance was found to be particularly relevant to suicide, several were weak predictors. Although this does not mean that sleep disturbances are inconsequential for suicide risk, it indicates that the relationships between sleep disturbances and suicide are likely to be small, individual, and highly variable. Sleep disturbances are not necessary or sufficient in isolation for suicidality to arise. Continuing to examine which sleep disturbances contribute to suicide risk is unlikely to improve suicide prediction and prevention. Instead, a more promising path may be identifying how sleep disturbances can be incorporated into complex conceptualizations of suicide risk.
The aim of suicide science is not only to predict risk, but to uncover the causal processes underlying suicide and disrupt them. Our second recommendation is for future research to clarify causal mechanisms underlying the relationship between sleep and suicide. Longitudinal studies can establish risk factors, but they are unable to test causal hypotheses25. Experimental designs, in contrast, isolate the direct influence of risk factors; only experiments can be used to draw causal conclusions. Experiments are rare within the field of suicide research, but technological advances make it possible to safely and validly test causal hypotheses about suicide80. Experiments are more common in sleep research. The effects of experimentally induced sleep deprivation have been examined in the context of working memory81, pain perception82, and inflammation83. To our knowledge, no experiments to date have examined the influence of sleep disturbances on suicide. Future studies which leverage sleep deprivation paradigms in tandem with experimental approaches to studying suicide would advance our knowledge of whether sleep disturbances represent causal risk factors for suicide. This is a critical step toward designing interventions that directly target the causes of suicidal behaviour.
In sum, sleep disturbances increase risk for future suicide ideation, attempt, and death; however, these effects are weak in magnitude. The existing literature is methodologically constrained, but even with methodological advances, sleep disturbances are unlikely to emerge as strong univariate predictors of suicide. Although our results cast doubt on the utility of relying on sleep disturbances in isolation as warning signs for suicide, we look forward to future research examining the complex contributions of sleep disturbances to suicide risk. Future experimental studies are also needed to uncover potential causal mechanisms underlying the relationship between sleep disturbances and suicide.
Data availability
All relevant data are available upon reasonable request to the corresponding author.
References
Czeisler, C. A. & Klerman, E. B. Circadian and sleep-dependent regulation of hormone release in humans. Recent Prog. Hormdiscussion 130–2. Res. 54, 97–130 (1999).
Dattilo, M. et al. Sleep and muscle recovery: Endocrinological and molecular basis for a new and promising hypothesis. Med. Hypotheses 77, 220–222 (2011).
Stickgold, R. Sleep-dependent memory consolidation. Nature 437, 1272–1278 (2005).
Gerner, R. H., Post, R. M., Gillin, C. & Bunney, W. E. Biological and behavioral effects of one night’s sleep deprivation in depressed patients and normals. J. Psychiatry Res. 15, 21–40 (1979).
Nilsson, J. P. et al. Less effective executive functioning after one night’s sleep deprivation. J. Sleep Res. 14, 1–6 (2005).
Williams, H. L., Gieseking, C. F. & Lubin, A. Some effects of sleep loss on memory. Percept. Mot. Skills 23, 1287–1293 (1966).
Tsuno, N., Besset, A. & Ritchie, K. Sleep and depression. J. Clin. Psychiatry 66, 1254–1269 (2005).
Plante, D. T. & Winkelman, J. W. Sleep disturbance in bipolar disorder: Therapeutic implications. Am. J. Psychiatry 165, 830–843 (2008).
Babson, K. A., Trainor, C. D., Feldner, M. T. & Blumenthal, H. A test of the effects of acute sleep deprivation on general and specific self-reported anxiety and depressive symptoms: An experimental extension. J. Behav. Ther. Exp. Psychiatry 41, 297–303 (2010).
Rudd, M. D. et al. Warning signs for suicide: Theory, research, and clinical applications. Suicide Life. Threat. Behav. 36, 255–262 (2006).
Agargun, M. Y. & Cartwright, R. REM sleep, dream variables and suicidality in depressed patients. Psychiatry Res. 119, 33–39 (2003).
Ağargün, M. Y., Kara, H. & Solmaz, M. Sleep disturbances and suicidal behavior in patients with major depression. J. Clin. Psychiatry 58, 249–251 (1997).
Krakow, B., Ribeiro, J. D., Ulibarri, V. A., Krakow, J. & Joiner, T. E. Sleep disturbances and suicidal ideation in sleep medical center patients. J. Affect. Disord. 131, 422–427 (2011).
Lee, Y. J., Cho, S.-J., Cho, I. H. & Kim, S. J. Insufficient sleep and suicidality in adolescents. Sleep 35, 455–460 (2012).
Woosley, J. A., Lichstein, K. L., Taylor, D. J., Riedel, B. W. & Bush, A. J. Insomnia complaint versus sleep diary parameters: Predictions of suicidal ideation. Suicide Life. Threat. Behav. 46, 88–95 (2016).
Roth, T. et al. Sleep problems, comorbid mental disorders, and role functioning in the National Comorbidity Survey Replication (NCS-R). Biol. Psychiatry 60, 1364–1371 (2006).
Sivertsen, B., Krokstad, S., Øverland, S. & Mykletun, A. The epidemiology of insomnia: Associations with physical and mental health. J. Psychosom. Res. 67, 109–116 (2009).
Taylor, D. J., Lichstein, K. L., Durrence, H. H., Reidel, B. W. & Bush, A. J. Epidemiology of insomnia, depression, and anxiety. Sleep 28, 1457–1464 (2005).
Diagnostic and statistical manual of mental disorders: DSM-5 (American Psychiatric Association, 2013).
Morin, C. M., Colecchi, C., Stone, J., Sood, R. & Brink, D. Behavioral and pharmacological therapies for late-life insomnia: A randomized controlled trial. JAMA 281, 991–999 (1999).
Taylor, D. J. & Pruiksma, K. E. Cognitive and behavioural therapy for insomnia (CBT-I) in psychiatric populations: A systematic review. Int. Rev. Psychiatry 26, 205–213 (2014).
Stinson, K., Tang, N. K. Y. & Harvey, A. G. Barriers to treatment seeking in primary insomnia in the United Kingdom: A cross-sectional perspective. Sleep 29, 1643–1646 (2006).
Sudak, H., Maxim, K. & Carpenter, M. Suicide and stigma: A review of the literature and personal reflections. Acad. Psychiatry 32, 136–142 (2008).
Pigeon, W. R., Bishop, T. M. & Titus, C. E. The relationship between sleep disturbance, suicidal ideation, suicide attempts, and suicide among adults: A systematic review. Psychiatry Ann. 46, 177–186 (2016).
Kraemer, H. et al. Coming to term with the terms of risk. Arch. Gen. Psychiatry 54, 337–343 (1997).
Blumenthal, S., Bell, V., Neumann, N. U., Schuttler, R. & Vogel, R. Mortality and rate of suicide of first admission psychiatric patients: A 5-year follow-up of a prospective longitudinal study. Psychopathology 50–56 (1989).
Li, S. X., Lam, S. P., Yu, M. W. M., Zhang, J. & Wing, Y.-K. Nocturnal sleep disturbances as a predictor of suicide attempts among psychiatric outpatients: A clinical, epidemiologic Prospective Study. J. Clin. Psychiatry 71, 1440–1446 (2010).
Pien, F.-C. et al. Changes in quality of life after a suicide attempt. West. J. Nurs. Res. 38, 721–737 (2016).
Bernert, R. A., Turvey, C. L., Conwell, Y. & Joiner, T. E. Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: A longitudinal, population-based study of late life. JAMA Psychiatry 71, 1129 (2014).
Bjørngaard, J. H., Bjerkeset, O., Romundstad, P. & Gunnell, D. Sleeping problems and suicide in 75,000 Norwegian Adults: A 20 year follow-up of the HUNT I Study. Sleep 34, 1155–1159 (2011).
Mars, B. et al. Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: A population-based birth cohort study. Lancet Psychiatry 6, 327–337 (2019).
Allan, N. P. et al. Insomnia and suicidal ideation and behaviors in former and current U.S. service members: Does depression mediate the relations?. Psychiatry Res. 252, 296–302 (2017).
Liu, X. et al. Daytime sleepiness predicts future suicidal behavior: A longitudinal study of adolescents. Sleep 42, zsy225 (2019). https://doi.org/10.1093/sleep/zsy225.
Wakefield, J. C. & Schmitz, M. F. Feelings of worthlessness during a single complicated major depressive episode predict postremission suicide attempt. Acta Psychiatry Scand. 133, 257–265 (2016).
Eikelenboom, M., Beekman, A. T. F., Penninx, B. W. J. H. & Smit, J. H. A 6-year longitudinal study of predictors for suicide attempts in major depressive disorder. Psychol. Med. 49, 911–921 (2019).
Hung, G.C.-L., Kwok, C.-L., Yip, P. S., Gunnell, D. & Chen, Y.-Y. Predicting suicide in older adults—A community-based cohort study in Taipei City, Taiwan. J. Affect. Disord. 172, 165–170 (2015).
Sandman, N. et al. Nightmares as predictors of suicide: An extension study including war veterans. Sci. Rep. 7, 44756 (2017).
Kim, S. Y., Sim, S. & Choi, H. G. High stress, lack of sleep, low school performance, and suicide attempts are associated with high energy drink intake in adolescents. PLoS ONE 12, e0187759 (2017).
Schneider, B. et al. Living alone, obesity, and smoking increase risk for suicide independently of depressive mood findings from the population-based MONICA/KORA Augsburg cohort study. J. Affect. Disord. 152–154, 416–421 (2014).
Suh, S. et al. Longitudinal course of depression scores with and without insomnia in non-depressed individuals: A 6-year follow-up longitudinal study in a Korean Cohort. Sleep 36, 369–376 (2013).
Bernert, R. A., Hom, M. A., Iwata, N. G. & Joiner, T. E. Objectively assessed sleep variability as an acute warning sign of suicidal ideation in a longitudinal evaluation of young adults at high suicide risk. J. Clin. Psychiatry 78, e678–e687 (2017).
Littlewood, D. L. et al. Short sleep duration and poor sleep quality predict next-day suicidal ideation: An ecological momentary assessment study. Psychol. Med. 49, 403–411 (2018).
Armitage, R., Trivedi, M., Hoffmann, R. A. & John, R. Relationship between objective and subjective sleep measures in depressed patients and healthy controls. Depress. Anxiety 5, 97–102 (1997).
Bertocci, M. A. et al. Subjective sleep complaints in pediatric depression: A controlled study and comparison with EEG measures of sleep and waking. J. Am. Acad. Child Adolesc. Psychiatry 44, 1158–1166 (2005).
Ancoli-Israel, S. et al. The role of actigraphy in the study of sleep and circadian rhythms. Sleep 26, 342–392 (2003).
Ballard, E. D. et al. Nocturnal wakefulness is associated with next-day suicidal ideation in major depressive disorder and bipolar disorder. J. Clin. Psychiatry 77, 825–831 (2016).
Ribeiro, J. D. et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J. Affect. Disord. 136, 743–750 (2012).
Britton, P. C., Ilgen, M. A., Rudd, M. D. & Conner, K. R. Warning signs for suicide within a week of healthcare contact in Veteran decedents. Psychiatry Res. 200, 395–399 (2012).
Ribeiro, J. D., Yen, S., Joiner, T. & Siegler, I. C. Capability for suicide interacts with states of heightened arousal to predict death by suicide beyond the effects of depression and hopelessness. J. Affect. Disord. 188, 53–59 (2015).
Pigeon, W. R., Pinquart, M. & Conner, K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J. Clin. Psychiatry 73, e1160–e1167 (2012).
Glenn, C. R. & Nock, M. K. Improving the short-term prediction of suicidal behavior. Am. J. Prev. Med. 47, S176–S180 (2014).
Walsh, C. G., Ribeiro, J. D. & Franklin, J. C. Predicting risk of suicide attempts over time through machine learning. Clin. Psychol. Sci. 5, 457–469 (2017).
Franklin, J. C. et al. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol. Bull. 143, 187–232 (2017).
Ribeiro, J. D., Huang, X., Fox, K. R. & Franklin, J. C. Depression and hopelessness as risk factors for suicide ideation, attempts and death: Meta-analysis of longitudinal studies. Br. J. Psychiatry 212, 279–286 (2018).
Ribeiro, J. D. et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: A meta-analysis of longitudinal studies. Psychol. Med. 46, 225–236 (2016).
R Core Team. R: A Language and Environment for Statistical Computing. (R Foundation for Statistical Computing, 2019).
Viechtbauer, W. Conducting Meta-Analyses in R with the metafor Package (Version 2.4). J. Stat. Softw. 36, (2010). https://www.jstatsoft.org/v36/i03/.
Bentley, K. H. et al. Anxiety and its disorders as risk factors for suicidal thoughts and behaviors: A meta-analytic review. Clin. Psychol. Rev. 43, 30–46 (2016).
Witte, T. K., Gauthier, J. M., Huang, X., Ribeiro, J. D. & Franklin, J. C. Is externalizing psychopathology a robust risk factor for suicidal thoughts and behaviors? A meta-analysis of longitudinal studies. J. Clin. Psychol. 74, 1607–1625 (2018).
Lemola, S., Ledermann, T. & Friedman, E. M. Variability of sleep duration is related to subjective sleep quality and subjective well-being: An actigraphy study. PLOS ONE 8, e71292 (2013).
Chung, S. et al. Environmental noise and sleep disturbance: Night-to-night variability of sleep/wake pattern. Sleep Med. Res. 7, 78–81 (2016).
Cukrowicz, K. C. et al. Course of suicide ideation and predictors of change in depressed older adults. J. Affect. Disord. 113, 30–36 (2009).
Glenn, C. R. et al. Implicit identification with death predicts change in suicide ideation during psychiatric treatment in adolescents. J. Child Psychol. Psychiatry 58, 1319–1329 (2017).
Franklin, J. C. et al. A brief mobile app reduces nonsuicidal and suicidal self-injury: Evidence from three randomized controlled trials. J. Consult. Clin. Psychol. 84, 544–557 (2016).
Ribeiro, J. D., Huang, X., Fox, K. R., Walsh, C. G. & Linthicum, K. P. Predicting imminent suicidal thoughts and nonfatal attempts: The role of complexity. Clin. Psychol. Sci. 7, 941–957 (2019).
Casler, K., Bickel, L. & Hackett, E. Separate but equal? A comparison of participants and data gathered via Amazon’s MTurk, social media, and face-to-face behavioral testing. Comput. Hum. Behav. 29, 2156–2160 (2013).
Hauser, D. J. & Schwarz, N. Attentive Turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behav. Res. Methods 48, 400–407 (2016).
Zuromski, K. L., Cero, I. & Witte, T. K. Insomnia symptoms drive changes in suicide ideation: A latent difference score model of community adults over a brief interval. J. Abnorm. Psychol. 126, 739–749 (2017).
Kivelä, L. et al. Longitudinal course of suicidal ideation and predictors of its persistence—A NESDA study. J. Affect. Disord. 257, 365–375 (2019).
Wong, M. M., Brower, K. J. & Zucker, R. A. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J. Psychiatry Res. 45, 505–511 (2011).
Sjöström, N., Hetta, J. & Waern, M. Persistent nightmares are associated with repeat suicide attempt. Psychiatry Res. 170, 208–211 (2009).
Roane, B. M. & Taylor, D. J. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep 31, 1351–1356 (2008).
Tanskanen, A. et al. Nightmares as predictors of suicide. Sleep 24, 845–848 (2001).
Li, S. X. et al. Sleep disturbances and suicide risk in an 8-year longitudinal study of schizophrenia-spectrum disorders. Sleep 39, 1275–1282 (2016).
Shiffman, S. et al. Remember that? A comparison of real-time versus retrospective recall of smoking lapses. J. Consult. Clin. Psychol. 65, 292 (1997).
Littlewood, D., Kyle, S. D., Pratt, D., Peters, S. & Gooding, P. Examining the role of psychological factors in the relationship between sleep problems and suicide. Clin. Psychol. Rev. 54, 1–16 (2017).
Fox, K. R. et al. Meta-analysis of risk factors for nonsuicidal self-injury. Clin. Psychol. Rev. 42, 156–167 (2015).
Fox, K. R. et al. Model complexity improves the prediction of nonsuicidal self-injury. J. Consult. Clin. Psychol. 87, 684 (2019).
Ribeiro, J. D. et al. Letter to the Editor: Suicide as a complex classification problem: machine learning and related techniques can advance suicide prediction—A reply to Roaldset (2016). Psychol. Med. 46, 2009–2010 (2016).
Franklin, J. C., Huang, X. & Bastidas, D. Virtual reality suicide: Development of a translational approach for studying suicide causes. Behav. Res. Ther. https://doi.org/10.1016/j.brat.2018.12.013 (2018).
Lim, J. & Dinges, D. F. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychol. Bull. 136, 375–389 (2010).
Schrimpf, M. et al. The effect of sleep deprivation on pain perception in healthy subjects: A meta-analysis. Sleep Med. 16, 1313–1320 (2015).
Irwin, M. R., Olmstead, R. & Carroll, J. E. Sleep disturbance, sleep duration, and inflammation: A systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol. Psychiatry 80, 40–52 (2016).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6, e1000097 (2009).
Author information
Authors and Affiliations
Contributions
LMH and JDR devised the present project. LMH took the lead in writing the manuscript, in consultation with all other authors. LMH, XH, CPB, and KPL coded data for analyses. LMH analysed the data. JDR supervised the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Harris, L.M., Huang, X., Linthicum, K.P. et al. Sleep disturbances as risk factors for suicidal thoughts and behaviours: a meta-analysis of longitudinal studies. Sci Rep 10, 13888 (2020). https://doi.org/10.1038/s41598-020-70866-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-70866-6
This article is cited by
-
Prevalence and correlates of sleep disturbance among adolescents in the eastern seaboard of China
BMC Public Health (2024)
-
Identifying major depressive disorder with associated sleep disturbances through fMRI regional homogeneity at rest
BMC Psychiatry (2023)
-
Mediation effect of insomnia symptoms between positive psychotic like experiences and suicidal ideation among Lebanese young adults
BMC Psychiatry (2023)
-
Mental health of South Korean adolescents in the COVID-19 Era: Web-based survey focused on suicide-related factors
Child and Adolescent Psychiatry and Mental Health (2023)
-
Insomnische Symptome und Suizidalität – Zusammenhänge und Management
neuropsychiatrie (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.