Abstract
The magnetic sphincter augmentation (MSA) device has been proven safe and effective in controlling typical reflux symptoms and esophageal acid exposure for up to 6-year follow-up. Longer term outcomes have not been reported yet. A prospectively maintained database was reviewed to assess long-term safety and efficacy of the laparoscopic MSA procedure at a single referral center. Gastro-Esophageal Reflux Disease-Health Related Quality of Life (GERD-HRQL), use of proton-pump inhibitors (PPI), and esophageal acid exposure were compared to baseline. Favorable outcomes were defined as ≥ 50% improvement of GERD-HRQL total score and PPI discontinuation. Between March 2007 and March 2020, 335 patients met the study inclusion criteria, and 124 of them were followed from 6 to 12 years after surgery (median 9 years, IQR 2). Mean total GERD-HRQL score significantly improved from 19.9 to 4.01 (p < 0.001), and PPI were discontinued by 79% of patients. The mean total percent time with pH < 4 decreased from 9.6% at baseline to 4.1% (p < 0.001), with 89% of patients achieving pH normalization. Independent predictors of a favorable outcome were age at intervention < 40 years (OR 4.17) and GERD-HRQL score > 15 (OR 4.09). We confirm long-term safety and efficacy of MSA in terms of symptom improvement, decreased drug dependency, and reduced esophageal acid exposure.
Similar content being viewed by others
Introduction
The global burden of gastroesophageal reflux disease (GERD) is enormous, with a pooled prevalence of 13.3% in community-based studies1. Symptoms and complications of GERD persist in up to 40% of patients treated with proton-pump inhibitors (PPI)2,3, and fundoplication is largely underused because of the steep learning curve and reported variability in outcomes4. The aim of fundoplication is to restore lower esophageal sphincter (LES) function by remodeling the esophagogastric junction5. Both total (Nissen) and partial (Toupet) fundoplication procedures require mobilization of the gastric fundus to be wrapped around the distal esophagus6. To further enhance the antireflux barrier, a crural diaphragmatic repair is routinely added7. Currently, the fact that fundoplication is offered to less than 1% of the GERD population may have an impact on the progression of symptoms and the development of Barrett’s esophagus8.
The magnetic sphincter augmentation (MSA) procedure (Linx Reflux Management System, Ethicon, Johnson & Johnson, Shoreview, Mn, USA) was developed as a less disruptive and more standardized and reproducible laparoscopic surgical option for the treatment of GERD. The MSA device is composed by a variable number of interlinked titanium beads with a magnetic core inside. This ring-like system produces a magnetic force that augments the LES. The first feasibility trial and a large prospective nonrandomized study were published in 20089 and 201310, respectively. The MSA procedure has been granted approval for clinical use by the Food and Drug Administration in 2012. Previous reports from our group have shown feasibility, safety, and efficacy of the MSA procedure up to 6 years of follow-up11,12. We now provide the long-term outcomes of a cohort of patients followed for a minimum of 6 years.
Subjects and methods
The study was a single-center, retrospective, single-arm study, where patients served as their own controls. The study protocol was approved by the Internal Review Board of IRCCS Policlinico San Donato (HSD 2019-072), and the research was performed in accordance with the relevant regulations. Informed consent was obtained from all study participants. The prospectively maintained database was reviewed to assess long-term safety and efficacy of the MSA. All patients who underwent a MSA procedure between March 2007 and March 30, 2020 were included in the study. Data analysis was performed in the whole group of patients and in a cohort of individuals followed for 6- to 12 years. Gastro-Esophageal Reflux Disease-Health Related Quality of Life (GERD-HRQL), use of proton-pump inhibitors (PPI), and esophageal pH monitoring parameters were compared to patients’ own preoperative data. Favorable outcome of the MSA procedure was defined as ≥ 50% improvement in GERD-HRQL total score and PPI discontinuation.
Preoperative assessment and patient selection
Before surgery, all patients referred for surgical therapy of GERD were evaluated by a multidisciplinary team including gastroenterologists, dieticians, and clinical psycologists at our center. The diagnostic assessment included the foregut symptom questionnaire and the GERD-HRQL questionnaire, upper gastrointestinal endoscopy, barium swallow study, ambulatory esophageal pH monitoring, and esophageal manometry. The foregut symptom questionnaire gives a score for heartburn, regurgitation, dysphagia, and chest pain on a scale of 0 to 4 (grade 0, none; grade 1, less than once a week; grade 2, several times a week; grade 3, daily, affecting lifestyle; grade 4, always, markedly affecting lifestyle. The GERD-HRQL score consists of 10 questions that specifically address GERD symptoms. Each question has a score ranging from 0 to 5, and the total score ranges from 0 to 5013. Preoperative determination of hernia size was based on upper gastrointestinal endoscopy and barium swallow study. Endoscopy evaluated the presence of hiatus hernia, morphology of the gastroesophageal valve using the Hill classification, grade of esophagitis using the Los Angeles classification, and the presence of Barrett esophagus using the Prague classification. Ambulatory esophageal pH monitoring was performed using trans-nasal pH-impedance equipment or the Bravo wireless system (48–96 h pH study). Measurements collected from esophageal pH testing included the DeMeester score and its individual components. A standard or, more recently, a high-resolution manometry were performed14. Main parameters investigated were the resting pressure and length of the LES, the distal esophageal amplitude (DEA) and/or the distal contractile integral (DCI), and the percent of effective contractions. An esophageal amplitude of less than 40 mm Hg and a greater than 50% of non-transmitted swallows indicated ineffective esophageal motility. Initial criteria for patient selection were the following: persistent reflux symptoms despite optimal PPI therapy, abnormal esophageal acid exposure confirmed by ambulatory esophageal pH monitoring, hiatus hernia < 3 cm, esophagitis < grade B, body mass index < 35 kg/m2, and absence of specific motility disorders. With further clinical experience and research, the criteria have been expanded to include patients with larger hiatus hernia, short Barrett’s esophagus, and mild esophageal dysmotility. The MSA procedure was not offered to patients with recurrent GERD after failed fundoplication or other surgical/endoscopic procedures at the esophagogastric junction, and to those with known history of nickel allergy or eating disorders.
Surgical approach
The MSA device was implanted via laparoscopy as previously described15. Under general anesthesia, the esophago-gastric junction was exposed following incision of the peritoneal reflection. The posterior vagus nerve was identified and separated from the esophagus for a length of about 1 cm. No short gastric vessels were divided. The esophageal circumference was measured with an appropriate magnetic sizer inserted through the retroesophageal tunnel. A minimal or formal posterior crura repair was performed depending on the size of the hiatal defect and the degree of hiatus hernia. Over the study period and starting from 2014, modifications of the surgical technique occurred. First, formal mediastinal dissection became routine practice; second, a new generation MSA device was introduced for use in magnetic resonance up to 1.5 T; and, third, a new generation sizer device for measuring the esophageal circumference was introduced.
Postoperative assessment and follow-up
All patients underwent a comprehensive clinical evaluation including the foregut symptom and the GERD-HRQL questionnaires, use and dosage of PPI, esophageal pH measurements, upper gastrointestinal endoscopy, and esophageal manometry. The treatment was considered successful if, compared to baseline, at least a 50% reduction in the total GERD-HRQL score and PPI discontinuation or at least a 50% dose reduction was achieved.
Statistical analysis
Continuous data are reported as median ± interquartile range (IQR) or mean ± standard deviation (SD). Patients served as their own control, and pre- and postoperative data were compared using the two-tailed, paired Student’s t test. Categorical demographic and baseline variables are reported as proportions or frequencies, and compared using Wilcoxon test for continuous outcomes and McNemar’s test for paired samples. A p value < 0.05 was considered statistically significant. Parameters of the univariate analysis with p < 0.05 were included in a multivariate logistic regression test to determine what independent variables might predict the clinical success of the surgical procedure. A p value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS software 23.0 (IBM, Armonk, New York, U.S.).
Results
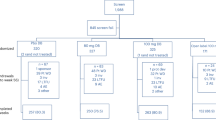
Between March 2007 and March 30, 2020, a total of 1,052 patients underwent laparoscopic surgery for GERD at our institution. A Toupet fundoplication was performed in 499 patients, Nissen fundoplication in 218, and MSA procedure in 335. The baseline demographic and clinical characteristics of patients who received MSA are listed in Table 1. Two patients died during the follow-up for unrelated reasons. Overall, there was more than 50% reduction in the total GERD-HRQL score compared to baseline in each year of follow-up (Fig. 1). Table 2 shows the median GERD-HRQL scores by question.
Postoperative adverse events and long-term safety profile
Adverse events were assessed from the time of implant through to the final visit. The rate of procedure-related adverse events was 11.6% (39/335) throughout the overall study period.
Eight patients (2.4%) required a single endoscopic pneumatic dilation due to persistent dysphagia at 11, 13, 21, 23, 28, 53, 60, and 65 months, respectively, after surgery. Thirty-one patients (9.2%) required laparoscopic device removal for various reasons (Table 3). The most common one-stage remedial procedure was a laparoscopic Toupet fundoplication (n = 18).
Long-term (6–12 year) outcomes
One-hundred-twenty-four patients, who were implanted between March 2007 and February 2014, had a minimum follow-up of 6 years. The median follow-up was 9 years (IQR 2). At the latest follow-up, 92 of 124 patients (74.2%) did not report any esophageal symptom (grade 0–1 for heartburn, regurgitation, dysphagia, and chest pain). The mean total GERD-HRQL score decreased from 19.9 at baseline to 4.01 at the latest follow-up (p < 0.001); 89% of patients met the criteria of favorable long-term outcome, Clinically significant improvement in GERD-HRQL is also reflected by the reported patient satisfaction, which was achieved in 92.7% of patients. The prevalence of grade 2–4 regurgitation significantly decreased from 59.6% at baseline to 9.6% postoperatively (p < 0.01). At the latest follow-up, complete or at least 50% reduction in the average daily dose of PPI was achieved by 79% and 89.5% of patients, respectively.
The majority of patients (86.3%) underwent upper gastrointestinal endoscopy after 6 years of follow-up. Hiatus hernia was found in 7 patients (6.5%), grade A esophagitis in 5 patients (4.7%), and incomplete intestinal metaplasia in 3 (2.8%). Four additional patients, who had been treated with radiofrequency ablation for short-segment Barrett’s esophagus without dysplasia before the MSA procedure, were followed endoscopically for up to 8 years without recurrence of intestinal metaplasia. The Hill grade was measured in 45 patients before and after surgery. At the latest endoscopic follow-up, 41 patients (91%) retained their preoperative Hill grade I or improved, 3 (7%) remained stable, and in 1 (2%) patient the Hill grade worsened (p < 0.01) (Fig. 2).
Esophageal pH testing off PPI therapy showed that the mean percentage of time that pH was < 4 decreased from 9.7% at baseline to 4.2% at latest follow-up (p < 0.001). All the other pH monitoring variables were significantly reduced at 6–12 years compared with baseline (Table 4). Eighty-nine percent of patients who completed esophageal pH monitoring at 6- to 12 years follow-up achieved either normal esophageal acid exposure or had at least a 50% reduction compared to baseline. Sequential pH studies were performed in 37 patients at various time intervals since surgery (Fig. 3).
Table 5 shows the long-term results in a subgroup of patients with follow-up longer than 10 years. Overall patient satisfaction, based on the question “would you undergo the operation again or recommend it to a friend?”, was 93.8%.
Predictors of long-term clinical success
Eighty-one percent of patients had a successful clinical outcome, defined as GERD-HRQL score improvement > 50% and complete discontinuation of PPI use. At univariate analysis, age at intervention < 40 years, preoperative GERD-HRQL total score > 15, duration of symptoms, regurgitation, atypical symptoms and absence of generalized anxiety disorder were statistically significant as independent predictors of clinical success and were included in the multivariate logistic regression test (Table 6). At multivariate analysis, independent predictive variables of successful outcome were confirmed to be age < 40 years and GERD-HRQL score > 15 (Table 7).
Discussion
This 6- to 12-year follow-up study of a cohort of patients undergoing MSA confirms satisfactory and durable clinical outcomes over a median follow-up of 9 years. The present report corroborates the findings of two previous studies with up to 6-year follow-up documenting symptom relief, discontinuation of PPI, minimal side effects, and long-term safety11,12.
The incidence of adverse events was low during the study time-frame, providing reasonable assurance that the risk of MSA complications does not increase with longer implant duration. The reasons for late device removal included dysphagia, continued reflux symptoms, and planned magnetic resonance imaging, but no erosions or migrations were observed. The overall reported rate of MSA device erosion is less than 0.5%; most events occurred within 4 years of the implant and have been managed electively without complications16,17,18. In our whole series, including 335 implants, most complications requiring MSA removal have occurred in patients implanted with a smaller (no.12 and 13) device. It should be noted that, during the study period, the sizer instrument has been replaced with a more user-friendly device in an attempt to improve the reproducibility of measurements. Furthermore, it has become clear over time that it is wiser to oversize by increasing 3 beads from the point of sizer release, and to use a larger MSA device to minimize dysphagia and decrease the likelihood of removal19,20. In our cohort of patients followed for 6–12 years, the overall estimated probability of MSA explant was 0.1 (Fig. 4).
Kaplan–Meier estimate of explant-free probability over 6- to 12-year follow-up after magnetic sphincter augmentation (95% confidence interval indicated pointwise). [Graph created using SPSS software 23.0, URL = https://www.ibm.com/software/analytics/spss/register/].
The results of the present study show a 0.7 estimated probability of clinical success of at 6 to 12 years of follow-up (Fig. 5). The overall satisfaction rate of our patients was 92.5%. The prevalence of grade 2–4 regurgitation was significantly decreased (p < 0.01), and this is consistent with the one-year results of a recent randomized trial comparing the effect of MSA versus PPI21. Our multivariate analysis indicated that age < 40 years is an independent predictive variable of successful outcome. This is consistent with the study by Ayazi et al.22 who found that male sex was also an independent predictive factor. The fact that MSA is more effective in younger and male patients is of particular interest because this operation may have a profound impact on the course of GERD if performed in an earlier disease stage23. In addition, a recent population-based study showed lower recurrence rates after fundoplication in young men who would otherwise require several decades of PPI therapy24.
Kaplan–Meier estimate of clinical success (GERD-HRQL < 50% reduction or PPI discontinuation) over 6- to 12-year follow-up after magnetic sphincter augmentation (95% confidence interval indicated pointwise).[Graph created using SPSS software 23.0, URL = https://www.ibm.com/software/analytics/spss/register/].
Although MSA was not directly compared with fundoplication in the present study, historical data from other clinical studies provide evidence that side effects typically associated with Nissen fundoplication, such as persistent dysphagia, gas bloat, and inability to belch/vomit, are less frequent and severe after the MSA procedure25,26. Of interest, disease-specific quality of life was similar in a propensity-score matched analysis comparing MSA and Toupet fundoplication27. In the present study, gas bloat and inability to belch/vomit were reported by 4% and 1.6% of patients, respectively.
The present study also suggests that the effect of MSA on esophageal acid exposure is sustained over time, as demonstrated by sequential pH studies showing reflux control up to 12 years of follow-up. Further, in a recent study, we showed that ineffective esophageal motility detected by high-resolution manometry can reverse to normal at a median of 12 months after MSA, and the only factor significantly associated to postoperative dysphagia was the presence of preoperative dysphagia14.
In recent years, it has become evident that the effectiveness of MSA can be enhanced by adding a formal crural repair28,29. The rationale behind this concept is that the extent of hiatus hernia can be underestimated both pre- and intraoperatively. Therefore, minimizing the amount of dissection performed and preserving the phreno-esophageal ligament may cause placement of the device below the true esophagogastric junction and may result in less effective reflux control. On the other hand, the MSA procedure is feasible even in large hernias based on our own clinical experience and other recent reports30,31,32,33,34.
Finally, encouraging data support the hypothesis that intestinal metaplasia can reverse after MSA35, especially in patients with short Barrett’s segments and in those with normalized DeMeester score. Although experience with MSA before or after radiofrequency ablation for Barrett’s esophagus is still very limited, we have successfully treated 4 patients who have been followed by endoscopy up to 8 years without recurrence.
The main limitations of this study are the retrospective design, the fact that there was no comparison treatment group, and the possible selection bias. However, despite the fact that criteria for patient selection, surgical technique, and type of device and sizer have evolved during the study period, the patient population of this study was homogeneous and indications for surgical therapy were consistent based on the preoperative pH study confirming GERD. Finally, this is the first report of a cohort of patients who completed the 6–12 year follow-up after MSA.
Conclusions
When offered as a first-line surgical option, MSA allows durable control of symptoms and esophageal acid exposure, and improves patient quality of life up to 12 years of follow-up without significant safety issues. A preoperative GERD-HRQL total score > 15 and age below 40 years are independent predictive factors of favorable outcome. Based on the above results and the high levels of patient satisfaction, MSA may represent a true paradigm shift that has the potential to fill the current therapy gap in GERD. A randomized clinical trial comparing MSA and either total or partial fundoplication could provide more robust and definitive conclusions.
References
Eusebi, L. H. et al. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut67, 430–440 (2018).
El-Serag, H. B., Becher, A. & Jones, R. Systematic review: persistent reflux symptoms on proton pump inhibitor therapy in primary care and community studies. Aliment Pharmacol. Ther.32, 720–737 (2010).
Kahrilas, P. J. et al. Regurgitation is less responsive to acid suppression than heartburn in patients with gastroesophageal reflux disease. Clin. Gastroenterol. Hepatol.10, 612–619 (2012).
Watson, D. I., Baigrie, R. J. & Jamieson, G. G. A learning curve for laparoscopic fundoplication. Definable, avoidable, or a waste of time?. Ann. Surg.224, 198–203 (1996).
Pandolfino, J. E. et al. Restoration of normal distensive characteristics of the esophagogastric junction after fundoplication. Ann. Surg.242, 43–48 (2005).
Bona, D., Aiolfi, A., Asti, E. & Bonavina, L. Laparoscopic Toupet fundoplication for gastroesophageal reflux disease and hiatus hernia: proposal for standardization using the “critical view” concept. Updates Surg.72(2), 555–558 (2020).
Louie, B. E. et al. Length and pressure of the reconstructed lower esophageal sphincter is determined by both crural closure and Nissen fundoplication. J. Gastrointest. Surg.17, 236–243 (2013).
Inadomi, J. et al. Recent advances in Barrett’s esophagus. Ann. N. Y. Acad. Sci.1434, 227–238 (2018).
Bonavina, L. et al. Magnetic augmentation of the lower esophageal sphincter: Results of a feasibility clinical trial. J. Gastrointest. Surg.12, 2133–2140 (2008).
Ganz, R. A. et al. Esophageal sphincter device for gastroesophageal reflux disease. N. Engl. J. Med.368, 719–727 (2013).
Saino, G., Bonavina, L., Lipham, J. C., Dunn, D. & Ganz, R. A. Magnetic sphincter augmentation for gastroesophageal reflux at 5 years: final results of a pilot study show long-term acid reduction and symptom improvement. J. Laparoendosc. Adv. Surg. Tech.25, 787–792 (2015).
Bonavina, L., Saino, G., Bona, D., Sironi, A. & Lazzari, V. One hundred consecutive patients treated with magnetic sphincter augmentation for gastroesophageal reflux disease: 6 years of clinical experience from a single center. J. Am. Coll. Surg.217, 577–585 (2013).
Velanovich, V. The development of the GERD-HRQL symptom severity instrument. Dis. Esophagus.20, 130–134 (2007).
Riva, C. G. et al. High-resolution manometry findings after Linx procedure for gastro-esophageal reflux disease. Neurogastroenterol. Motil.32(3), e13750 (2020).
Bonavina, L. et al. Laparoscopic sphincter augmentation devices eliminates reflux symptoms and normalizes esophageal acid exposure: one- and 2-year results of a feasibility trial. Ann. Surg.252, 857–862 (2010).
Lipham, J. C., Taiganides, P. A., Louie, B. E., Ganz, R. A. & DeMeester, T. R. Safety analysis of first 1000 patients treated with magnetic sphincter augmentation for gastroesophageal re- flux disease. Dis. Esophagus.28, 305–311 (2015).
Alicuben, E. T. et al. Worldwide experience with erosion of the magnetic sphincter augmentation device. J. Gastrointest. Surg.22, 1442–1447 (2018).
Asti, E. et al. Removal of the magnetic sphincter augmentation device. Surgical technique and results of a single-center cohort study. Ann. Surg.265(5), 941–945 (2017).
Tatum, J. M. et al. Removing the magnetic sphincter augmentation device: operative management and outcomes. Surg. Endosc.33, 2663–2669 (2019).
Ayazi, S. et al. Magnetic sphincter augmentation and postoperative dysphagia; characterization, clinical risk factors, and management. J. Gastrointest. Surg.24, 39–49 (2020).
Bell, R. et al. Magnetic sphincter augmentation superior to proton pump inhibitors for regurgitation in a 1-year randomized trial. Clin. Gastroenterol. Hepatol.18, 1736–1743 (2020).
Ayazi, S. et al. Clinical outcomes and predictors of favorable result after laparoscopic magnetic sphincter augmentation: single institution experience with over 500 patients. J. Am. Coll. Surg.230, 733–743 (2020).
Bonavina, L., Fisichella, P. M., Gavini, S., Lee, Y. Y. & Tatum, R. P. Clinical course of gastroesophageal reflux disease and impact of treatment in symptomatic young patients. Ann. N. Y. Acad. Sci. https://doi.org/10.1111/nyas.14350 (2020).
Maret-Ouda, J., Wahlin, K., El-Serag, H. B. & Lagergren, J. Association between laparoscopic antireflux surgery and recurrence of gastroesophageal reflux. JAMA318(10), 939–946 (2017).
Reynolds, J. L. et al. Laparoscopic magnetic sphincter augmentation vs laparoscopic Nissen fundoplication: A matched-pair analysis of 100 patients. J. Am. Coll. Surg.221, 123–128 (2015).
Ganz, R. A. et al. Long-term outcomes of patients receiving a magnetic sphincter augmentation device for gastroesophageal reflux. Clin. Gastroenterol. Hepatol.14, 671–677 (2016).
Asti, E., Bonitta, G., Lovece, A., Lazzari, V. & Bonavina, L. Longitudinal comparison of quality of life in patients undergoing laparoscopic Toupet fundoplication versus magnetic sphincter augmentation. Medicine.95, 30 (2016).
Schwameis, K. et al. Crural closure improves outcomes of magnetic sphincter augmentation in GERD patients with hiatal hernia. Sci. Rep.8, 7319 (2018).
Tatum, J. M. et al. Minimal versus obligatory dissection of the diaphragmatic hiatus during magnetic sphincter augmentation surgery. Surg. Endosc.33(3), 782–788 (2019).
Asti, E. et al. Magnetic sphincter augmentation for gastroesophageal reflux disease: review of clinical studies. Updates Surg.70, 323–330 (2018).
Mihura Irribarra, M. M. et al. Does treatment of the hiatus influence the outcomes of magnetic sphincter augmentation for chronic GERD?. J. Gastrointest. Surg.23(6), 1104–1112 (2019).
Buckley, F. P. III., Bell, R. C. W., Freeman, K., Doggett, S. & Heidrick, R. Favorable results from a prospective evaluation of 200 patients with large hiatal hernias undergoing LINX magnetic sphincter augmentation. Surg. Endosc.32(4), 1762–1768 (2018).
Kuckelman, J. P., Phillips, C. J., Hardin, M. O. & Martin, M. J. Standard vs expanded indications foe esophageal magnetic sphincter augmentation for reflux disease. JAMA Surg.152(9), 890–891 (2017).
Rona, K. A. et al. Efficacy of magnetic sphincter augmentation in patients with large hiatal hernias. Surg. Endosc.31, 2096–2102 (2017).
Alicuben, E. T. et al. Regression of intestinal metaplasia following magnetic sphincter augmentation. Surg. Endosc.33, 76–579 (2019).
Acknowledgements
Supported by AIRES (Associazione Italiana Ricerca Esofago).
Author information
Authors and Affiliations
Contributions
Study conception and design: L.B. Acquisition of data: V.L., S.S., D.B. Analysis and interpretation of data: D.F., E.A. Drafting of manuscript: D.F., L.B. Critical revision: L.B. All authors reviewed the manuscript and approved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ferrari, D., Asti, E., Lazzari, V. et al. Six to 12-year outcomes of magnetic sphincter augmentation for gastroesophageal reflux disease. Sci Rep 10, 13753 (2020). https://doi.org/10.1038/s41598-020-70742-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-70742-3
This article is cited by
-
Real-world evidence with magnetic sphincter augmentation for gastroesophageal reflux disease: a scoping review
European Surgery (2023)
-
S148: Long-term patient-reported outcomes of laparoscopic magnetic sphincter augmentation versus Nissen fundoplication: a 5-year follow-up study
Surgical Endoscopy (2022)
-
Magnetic Sphincter Augmentation Algorithm for Post-bariatric Surgery Gastroesophageal Reflux Disease Patients
Obesity Surgery (2022)
-
Practice-Changing Milestones in Anti-reflux and Hiatal Hernia Surgery: a Single Surgeon Perspective over 27 years and 1200 Operations
Journal of Gastrointestinal Surgery (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.