Abstract
Knowledge of pancreatitis in the 20th century was shaped predominantly by animal data and clinical trials. Several large general population-based cohort studies and comprehensive systematic literature reviews in the 21st century have had a major effect on our understanding of pancreatitis and its sequelae. This Review provides precise and up-to-date data on the burden of acute pancreatitis, chronic pancreatitis and post-pancreatitis diabetes mellitus. Exocrine pancreatic insufficiency and altered bone metabolism following pancreatitis are also discussed. Furthermore, the article introduces a framework for the holistic prevention of pancreatitis with a view to providing guidance on strategies and intervention objectives at primary, secondary and tertiary levels. Concerted efforts by not only gastroenterologists and surgeons but also primary care physicians, endocrinologists, radiologists, pain specialists, dietitians, epidemiologists and public health specialists will be required to reduce meaningfully the burden of pancreatitis and its sequelae over the ensuing decades.
Key points
-
Per 100,000 people in the general population, the yearly global incidence of acute pancreatitis is 34 cases, chronic pancreatitis is 10 cases and post-pancreatitis diabetes mellitus is 6 cases.
-
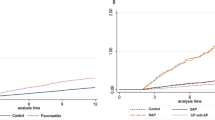
The global transition rate from the first episode of acute pancreatitis to a recurrent episode is ~20% and, from recurrent acute pancreatitis to chronic pancreatitis, the rate is ~35%.
-
Acute pancreatitis (including its non-necrotizing form) leads to a number of sequelae long after clinical resolution and, hence, should no longer be considered a self-limited disease.
-
Post-pancreatitis diabetes mellitus is the most frequent sequelae of pancreatitis, caused by acute and recurrent acute pancreatitis in ~80% and chronic pancreatitis in ~20% of cases.
-
Patients with pancreatitis have a greater than twofold higher lifetime risk of developing new onset diabetes than individuals in the general population without a history of pancreatitis.
-
The holistic prevention of pancreatitis (HPP) concept postulates that primary, secondary and tertiary prevention strategies need to be systematically employed to lessen the effect of pancreatitis and its sequelae.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Petrov, M. S. Abdominal fat: a key player in metabolic acute pancreatitis. Am. J. Gastroenterol. 108, 140–142 (2013).
Yadav, D., Papachristou, G. I. & Whitcomb, D. C. Alcohol-associated pancreatitis. Gastroenterol. Clin. North Am. 36, 219–238 (2007).
Sankaran, S. J. et al. Frequency of progression from acute to chronic pancreatitis and risk factors: a meta-analysis. Gastroenterology 149, 1490–1500 (2015).
Yadav, D. & Lowenfels, A. B. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology 144, 1252–1261 (2013).
DeSouza, S. V. et al. Pancreas volume in health and disease: a systematic review and meta-analysis. Expert Rev. Gastroenterol. Hepatol. 12, 757–766 (2018).
Machicado, J. D., Chari, S. T., Timmons, L., Tang, G. & Yadav, D. A population-based evaluation of the natural history of chronic pancreatitis. Pancreatology 18, 39–45 (2017).
Singh, R. G. et al. Abdominal obesity and insulin resistance after an episode of acute pancreatitis. Dig. Liver Dis. 50, 1081–1087 (2018).
Alsamarrai, A., Das, S. L., Windsor, J. A. & Petrov, M. S. Factors that affect risk for pancreatic disease in the general population: a systematic review and meta-analysis of prospective cohort studies. Clin. Gastroenterol. Hepatol. 12, 1635–1644 (2014).
Xiao, A. Y. et al. Global incidence and mortality of pancreatic diseases: a systematic review, meta-analysis, and meta-regression of population-based cohort studies. Lancet Gastroenterol. Hepatol. 1, 45–55 (2016).
Pendharkar, S. A., Mathew, J. & Petrov, M. S. Age- and sex-specific prevalence of diabetes associated with diseases of the exocrine pancreas: a population-based study. Dig. Liver Dis. 49, 540–544 (2017).
Pendharkar, S. A. et al. Ethnic and geographic variations in the incidence of pancreatitis and post-pancreatitis diabetes mellitus in New Zealand: a nationwide population-based study. N. Z. Med. J. 130, 55–68 (2017).
Roberts, S. E. et al. The incidence and aetiology of acute pancreatitis across Europe. Pancreatology 17, 155–165 (2017).
Lahariya, C. Vaccine epidemiology: a review. J. Family Med. Prim. Care 5, 7–15 (2016).
Lee, Y. K., Huang, M. Y., Hsu, C. Y. & Su, Y. C. Bidirectional relationship between diabetes and acute pancreatitis: a population-based cohort study in Taiwan. Medicine 95, e2448 (2016).
Shen, H. N., Yang, C. C., Chang, Y. H., Lu, C. L. & Li, C. Y. Risk of diabetes mellitus after first-attack acute pancreatitis: a national population-based study. Am. J. Gastroenterol. 110, 1698–1706 (2015).
Yadav, D., Timmons, L., Benson, J. T., Dierkhising, R. A. & Chari, S. T. Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. Am. J. Gastroenterol. 106, 2192–2199 (2011).
Hirota, M. et al. The seventh nationwide epidemiological survey for chronic pancreatitis in Japan: clinical significance of smoking habit in Japanese patients. Pancreatology 14, 490–496 (2014).
Frey, C., Zhou, H., Harvey, D. & White, R. H. Co-morbidity is a strong predictor of early death and multi-organ system failure among patients with acute pancreatitis. J. Gastrointest. Surg. 11, 733–742 (2007).
Hong, S., Qiwen, B., Ying, J., Wei, A. & Chaoyang, T. Body mass index and the risk and prognosis of acute pancreatitis: a meta-analysis. Eur. J. Gastroenterol. Hepatol. 23, 1136–1143 (2011).
Petrov, M. S., Shanbhag, S., Chakraborty, M., Phillips, A. R. & Windsor, J. A. Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology 139, 813–820 (2010).
Munigala, S. & Yadav, D. Case-fatality from acute pancreatitis is decreasing but its population mortality shows little change. Pancreatology 16, 542–550 (2016).
Yadav, D. & Lowenfels, A. B. Trends in the epidemiology of the first attack of acute pancreatitis: a systematic review. Pancreas 33, 323–330 (2006).
Acharya, C. et al. Fibrosis reduces severity of acute-on-chronic pancreatitis in humans. Gastroenterology 145, 466–475 (2013).
Nojgaard, C. et al. Danish patients with chronic pancreatitis have a four-fold higher mortality rate than the Danish population. Clin. Gastroenterol. Hepatol. 8, 384–390 (2010).
Petrov, M. S. Diabetes of the exocrine pancreas: American Diabetes Association-compliant lexicon. Pancreatology 17, 523–526 (2017).
Jivanji, C. J., Asrani, V. M., Windsor, J. A. & Petrov, M. S. New-onset diabetes after acute and critical illness: a systematic review. Mayo Clin. Proc. 92, 762–773 (2017).
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care 41, S13–S27 (2018).
Hart, P. A. et al. Type 3c (pancreatogenic) diabetes mellitus secondary to chronic pancreatitis and pancreatic cancer. Lancet Gastroenterol. Hepatol. 1, 226–237 (2016).
Wang, W. et al. Occurrence of and risk factors for diabetes mellitus in Chinese patients with chronic pancreatitis. Pancreas 40, 206–212 (2011).
Ito, T. et al. Pancreatic diabetes in a follow-up survey of chronic pancreatitis in Japan. J. Gastroenterol. 42, 291–297 (2007).
Das, S. L. et al. Newly diagnosed diabetes mellitus after acute pancreatitis: a systematic review and meta-analysis. Gut 63, 818–831 (2014).
Gillies, N. et al. Interleukin-6 is associated with chronic hyperglycemia and insulin resistance in patients after acute pancreatitis. Pancreatology 16, 748–755 (2016).
Gillies, N. A. et al. Fasting levels of insulin and amylin after acute pancreatitis are associated with pro-inflammatory cytokines. Arch. Physiol. Biochem. 123, 238–248 (2017).
Pendharkar, S. A., Singh, R. G., Chand, S. K., Cervantes, A. & Petrov, M. S. Pro-inflammatory cytokines after an episode of acute pancreatitis: associations with fasting gut hormone profile. Inflamm. Res. 67, 339–350 (2017).
Pendharkar, S. A. et al. The role of gut-brain axis in regulating glucose metabolism after acute pancreatitis. Clin. Transl Gastroenterol. 8, e210 (2017).
Pendharkar, S. A., Singh, R. G. & Petrov, M. S. Cross-talk between innate cytokines and the pancreatic polypeptide family in acute pancreatitis. Cytokine 90, 161–168 (2017).
Pendharkar, S. A., Walia, M., Drury, M. & Petrov, M. S. Calcitonin gene-related peptide: neuroendocrine communication between the pancreas, gut, and brain in regulation of blood glucose. Ann. Transl Med. 5, 419 (2017).
Gillies, N. A., Pendharkar, S. A., Singh, R. G., Asrani, V. M. & Petrov, M. S. Lipid metabolism in patients with chronic hyperglycemia after an episode of acute pancreatitis. Diabetes Metab. Syndr. 11, S233–S241 (2017).
Pendharkar, S. A., Singh, R. G. & Petrov, M. S. Pro-inflammatory cytokine-induced lipolysis after an episode of acute pancreatitis. Arch. Physiol. Biochem. https://doi.org/10.1080/13813455.2017.1415359 (2017).
Singh, R. G., Pendharkar, S. A., Plank, L. D. & Petrov, M. S. Role of human lipocalin proteins in abdominal obesity after acute pancreatitis. Peptides 91, 1–7 (2017).
Bharmal, S. H. et al. Relationship between circulating levels of pancreatic proteolytic enzymes and pancreatic hormones. Pancreatology 17, 876–883 (2017).
Pendharkar, S. A. et al. Relationship between pancreatic hormones and glucose metabolism: a cross-sectional study in patients after acute pancreatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 311, G50–G58 (2016).
Pendharkar, S. A., Drury, M., Walia, M., Korc, M. & Petrov, M. S. Gastrin-releasing peptide and glucose metabolism following pancreatitis. Gastroenterol. Res. 10, 224–234 (2017).
Woodmansey, C. et al. Incidence, demographics, and clinical characteristics of diabetes of the exocrine pancreas (type 3c): a retrospective cohort study. Diabetes Care 40, 1486–1493 (2017).
Ammann, R. W., Akovbiantz, A., Largiader, F. & Schueler, G. Course and outcome of chronic pancreatitis. Longitudinal study of a mixed medical-surgical series of 245 patients. Gastroenterology 86, 820–828 (1984).
Lankisch, P. G., Lohr-Happe, A., Otto, J. & Creutzfeldt, W. Natural course in chronic pancreatitis. Pain, exocrine and endocrine pancreatic insufficiency and prognosis of the disease. Digestion 54, 148–155 (1993).
Layer, P. et al. The different courses of early- and late-onset idiopathic and alcoholic chronic pancreatitis. Gastroenterology 107, 1481–1487 (1994).
DiMagno, E. P., Go, V. L. & Summerskill, W. H. Relations between pancreatic enzyme outputs and malabsorption in severe pancreatic insufficiency. N. Engl. J. Med. 288, 813–815 (1973).
Lankisch, P. G., Lembcke, B., Wemken, G. & Creutzfeldt, W. Functional reserve capacity of the exocrine pancreas. Digestion 35, 175–181 (1986).
Das, S. L. et al. Relationship between the exocrine and endocrine pancreas after acute pancreatitis. World J. Gastroenterol. 20, 17196–17205 (2014).
Migliori, M., Pezzilli, R., Tomassetti, P. & Gullo, L. Exocrine pancreatic function after alcoholic or biliary acute pancreatitis. Pancreas 28, 359–363 (2004).
Duggan, S. N. et al. High prevalence of osteoporosis in patients with chronic pancreatitis: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 12, 219–228 (2014).
Tignor, A. S. et al. High prevalence of low-trauma fracture in chronic pancreatitis. Am. J. Gastroenterol. 105, 2680–2686 (2010).
Munigala, S., Agarwal, B., Gelrud, A. & Conwell, D. L. Chronic pancreatitis and fracture: a retrospective, population-based veterans administration study. Pancreas 45, 355–361 (2016).
Bang, U. C., Benfield, T., Bendtsen, F., Hyldstrup, L. & Beck Jensen, J. E. The risk of fractures among patients with cirrhosis or chronic pancreatitis. Clin. Gastroenterol. Hepatol. 12, 320–326 (2014).
Lohr, J. M. et al. United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United Eur. Gastroenterol. J. 5, 153–199 (2017).
Hoogenboom, S. A., Lekkerkerker, S. J., Fockens, P., Boermeester, M. A. & van Hooft, J. E. Systematic review and meta-analysis on the prevalence of vitamin D deficiency in patients with chronic pancreatitis. Pancreatology 16, 800–806 (2016).
Lin, S. Y. et al. Effect of acute pancreatitis on the risk of developing osteoporosis: a nationwide cohort study. PLOS ONE 12, e0179358 (2017).
Doll, R. Prospects for prevention. Br. Med. J. (Clin. Res. Ed.) 286, 445–453 (1983).
Patterson, C. & Chambers, L. W. Preventive health care. Lancet 345, 1611–1615 (1995).
Maron, D. J. Nonlipid primary and secondary prevention strategies for coronary heart disease. Clin. Cardiol. 19, 419–423 (1996).
Orcau, A., Cayla, J. A. & Martinez, J. A. Present epidemiology of tuberculosis. Prevention and control programs. Enferm. Infecc. Microbiol. Clin. 29 (Suppl. 1), 2–7 (2011).
StoLoff, S. W. Asthma management and prevention: current perspectives. Clin. Cornerstone 8, 26–43 (2008).
Green, R., Charman, S. C. & Palser, T. Early definitive treatment rate as a quality indicator of care in acute gallstone pancreatitis. Br. J. Surg. 104, 1686–1694 (2017).
Nordback, I. et al. The recurrence of acute alcohol-associated pancreatitis can be reduced: a randomized controlled trial. Gastroenterology 136, 848–855 (2009).
Christian, J. B. et al. Clinical and economic benefits observed when follow-up triglyceride levels are less than 500 mg/dL in patients with severe hypertriglyceridemia. J. Clin. Lipidol. 6, 450–461 (2012).
Eibl, G. et al. Diabetes mellitus and obesity as risk factors for pancreatic cancer. J. Acad. Nutr. Diet 118, 555–567 (2018).
Korc, M. et al. Tobacco and alcohol as risk factors for pancreatic cancer. Best Pract. Res. Clin. Gastroenterol. 31, 529–536 (2017).
Cotton, P. B. et al. Effect of endoscopic sphincterotomy for suspected sphincter of Oddi dysfunction on pain-related disability following cholecystectomy: the EPISOD randomized clinical trial. JAMA 311, 2101–2109 (2014).
Yaghoobi, M. et al. Incidence and predictors of post-ERCP pancreatitis in patients with suspected sphincter of Oddi dysfunction undergoing biliary or dual sphincterotomy: results from the EPISOD prospective multicenter randomized sham-controlled study. Endoscopy 47, 884–890 (2015).
Akbar, A. et al. Rectal nonsteroidal anti-inflammatory drugs are superior to pancreatic duct stents in preventing pancreatitis after endoscopic retrograde cholangiopancreatography: a network meta-analysis. Clin. Gastroenterol. Hepatol. 11, 778–783 (2013).
Inamdar, S., Han, D., Passi, M., Sejpal, D. V. & Trindade, A. J. Rectal indomethacin is protective against post-ERCP pancreatitis in high-risk patients but not average-risk patients: a systematic review and meta-analysis. Gastrointest. Endosc. 85, 67–75 (2017).
Tse, F., Yuan, Y., Moayyedi, P., Leontiadis, G. I. & Barkun, A. N. Double-guidewire technique in difficult biliary cannulation for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Endoscopy 49, 15–26 (2017).
de-Madaria, E. Statins for the prevention of acute pancreatitis. Am. J. Gastroenterol. 112, 1765–1767 (2017).
Kaushik, N., Pietraszewski, M., Holst, J. J. & O’Keefe, S. J. Enteral feeding without pancreatic stimulation. Pancreas 31, 353–359 (2005).
Petrov, M. S. & Windsor, J. A. Nutritional management of acute pancreatitis: the concept of ‘gut rousing’. Curr. Opin. Clin. Nutr. Metab. Care 16, 557–563 (2013).
Wu, L. M., Pendharkar, S. A., Asrani, V. M., Windsor, J. A. & Petrov, M. S. Effect of intravenous fluids and analgesia on dysmotility in patients with acute pancreatitis: a prospective cohort study. Pancreas 46, 858–866 (2017).
Bevan, M. G., Asrani, V. & Petrov, M. S. The oral refeeding trilemma of acute pancreatitis: what, when and who? Expert Rev. Gastroenterol. Hepatol. 9, 1305–1312 (2015).
Pandol, S. J., Forsmark, C. E. & Hart, P. A. The Consortium for the Study of Chronic Pancreatitis, Diabetes, and Pancreatic Cancer (CPDPC). Acceleration of our understanding of recurrent acute and chronic pancreatitis. Pancreatology 16, 692–693 (2016).
Whitcomb, D. C. et al. Chronic pancreatitis: an international draft consensus proposal for a new mechanistic definition. Pancreatology 16, 218–224 (2016).
Ho, T. W. et al. Change of both endocrine and exocrine insufficiencies after acute pancreatitis in non-diabetic patients: a nationwide population-based study. Medicine 94, e1123 (2015).
Bellin, M. D. et al. Patient and disease characteristics associated with the presence of diabetes mellitus in adults with chronic pancreatitis in the United States. Am. J. Gastroenterol. 112, 1457–1465 (2017).
Soo, D. H. E. et al. Derivation and validation of the prediabetes self-assessment screening score after acute pancreatitis (PERSEUS). Dig. Liver Dis. 49, 1146–1154 (2017).
Jivanji, C. J., Soo, D. H. & Petrov, M. S. Towards reducing the risk of new onset diabetes after pancreatitis. Minerva Gastroenterol. Dietol. 63, 270–284 (2017).
Acknowledgements
M.S.P. is supported by the Royal Society of New Zealand in the form of a Rutherford Discovery Fellowship. D.Y. is supported by the National Cancer Institute and National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number U01 DK108306. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Reviewer information
Nature Reviews Gastroenterology & Hepatology thanks H. van Santwoort and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
Both authors contributed equally to the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Petrov, M.S., Yadav, D. Global epidemiology and holistic prevention of pancreatitis. Nat Rev Gastroenterol Hepatol 16, 175–184 (2019). https://doi.org/10.1038/s41575-018-0087-5
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41575-018-0087-5
This article is cited by
-
Neutrophil CD64 index as a new early predictive biomarker for infected pancreatic necrosis in acute pancreatitis
Journal of Translational Medicine (2024)
-
Critical appraisal of machine learning prognostic models for acute pancreatitis: protocol for a systematic review
Diagnostic and Prognostic Research (2024)
-
Revealing Prdx4 as a potential diagnostic and therapeutic target for acute pancreatitis based on machine learning analysis
BMC Medical Genomics (2024)
-
Therapeutic plasma exchange decreases serum triglyceride level rapidly and reduces early recurrence rate but no advantages in improving outcomes for patients with hyperlipidemic acute pancreatitis: a retrospective propensity score matching analysis based on twenty year’s experience
BMC Endocrine Disorders (2024)
-
An inflammation-based model for identifying severe acute pancreatitis: a single-center retrospective study
BMC Gastroenterology (2024)