Abstract
Data sources CENTRAL, MEDLINE, Embase and CINAHL.
Study selection Controlled studies (randomised or non-randomised) that evaluated the effect of full-body PPE on healthcare workers (HCW) exposed to highly infectious diseases, assessed which method of donning and doffing PPE was associated with reduced risk of contamination or infection for HCW, and which training methods increased compliance with PPE protocols.
Data extraction and synthesis Two reviewers independently screened the titles and abstracts for inclusion of studies. Full text articles were subsequently assessed for eligibility and disagreements were resolved through consensus. Using criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions, pairs of review authors independently assessed risk of bias for each randomised study and rated each potential source of bias as high, low, or unclear.
ROBINS-I tool was used for the assessment of risk of bias in non-randomised intervention studies. Where appropriate, random effects meta-analyses were conducted.
Results A total of 24 studies (randomised controlled trials [RCT] [n = 14]; Quasi-RCT [n = 1] and non-randomised design [n=9]) with 2278 participants were included. Included studies compared types of PPE (n = 8), evaluated modified PPE (n = 6), procedures for donning and doffing PPE (n = 8), and types of training (n = 3). Twenty-two studies were simulation studies, of which 18 simulated exposure of HCW to contaminated body fluids using fluorescent markers or harmless microbes and measured contamination outcomes, and four studies provided modified PPE or procedures and measured compliance with donning and doffing procedures.
Types of PPE
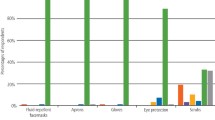
Powered, air-purifying respirator with coverall may protect against the risk of contamination better than a N95 mask and gown (risk ratio [RR] 0.27, 95% confidence interval [CI] 0.17 to 0.43) but was more difficult to don (non-compliance: RR 7.5, 95% CI 1.81 to 31.1). Gowns compared to aprons may protect better against contamination (MD) -10.28, 95% CI -14.77 to -5.79). Breathable types of PPE are more comfortable and may increase user satisfaction, however with little impact on contamination.
Modified PPE versus standard PPE
Appropriate modifications to PPE design may lead to less contamination compared to standard PPE. For example, contamination can be reduced using a sealed gown and glove combination so that they can be removed together and cover the wrist area (RR 0.27, 95% CI 0.09 to 0.78), tight fitting gown around the neck, wrist area and hands (RR 0.08, 95% CI 0.01 to 0.55) and added tabs to facilitate doffing of masks (RR 0.33, 95%nCI 0.14 to 0.80) or gloves (RR 0.22, 95% CI 0.15 to 0.31).
Guidance on PPE use: following the guidance and recommendations from the Centres for Disease Control and Prevention for doffing PPE compared to no guidance may reduce self-contamination (MD −5.44, 95% CI −7.43 to −3.45). One-step removal of gloves and gown compared to separate removal (RR 0.20, 95% CI 0.05 to 0.77), double gloving compared to single gloving (RR 0.34, 95% CI 0.17 to 0.66) and sanitising gloves before doffing with quaternary ammonium or bleach (but not alcohol-based hand rub) may decrease contamination. Additional verbal instructions may lead to fewer errors in doffing (MD −0.9, 95% CI −1.4 to −0.4).
User training
To a vast extent, face-to-face training may reduce non-compliance with doffing guidance (odds ratio 0.45, 95% CI 0.21 to 0.98) compared to solely providing folders or videos. In addition, computer simulation may lead to fewer errors in doffing (MD −1.2, 95% CI −1.6 to −0.7) and video lecture on donning PPE may lead to better skills scores (MD 30.70, 95% CI 20.14 to 41.26) compared to traditional lectures.
Conclusions The more body parts are covered with PPE the better protection it offers. However, this is also associated and increased difficulty in donning and doffing PPE, and the PPE is less comfortable. Coveralls are the most difficult PPE to remove but may offer the best protection, followed by long gowns, gowns and aprons. The included studies had a high or unclear risk of bias, indirectness of evidence in simulation studies and small participant numbers. This increases the uncertainty about the estimates of effects, and it is likely that the true effects may be substantially different from the ones reported in this review.
Similar content being viewed by others
A commentary on
Verbeek J H, Rajamaki B, Ijaz S et al.
Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev 2020; 4: CD011621. DOI: 10.1002/14651,858.CD011621.pub4.

GRADE rating
Commentary
The Cochrane systematic review and meta-analysis by Verbeek et al. (2020) comprehensively evaluated the effectiveness of different types of personal protective equipment (PPE) in reducing the risk of infection transmission among healthcare workers due to exposure to contaminated body fluids.1 In the midst of COVID-19 pandemic, this review provides timely and critical evidence to healthcare professionals on reducing transmission of infection in healthcare settings.
The World Health Organisation declared the COVID-19 outbreak as a public health emergency of international concern on 30 January 2020 and subsequently a global pandemic on 11 March 2020. Currently, there is no effective vaccine against COVID-19, and disease countermeasures mainly rely on preventing or slowing person-to-person transmission.2 Studies acknowledge the need to consider regional epidemic characteristics such as the prevalence of COVID-19 cases and trend of the epidemic curve when determining the level of PPE required within specific healthcare settings.3

© Morsa Images/DigitalVision/Getty Images Plus
The WHO guideline for 'infection prevention and control of pandemic respiratory infections in healthcare' recommends using appropriate types of PPE based on risk assessment, determined by the nature of procedure and suspected pathogen.4,5 Consequently, the type of PPE worn by HCWs is critical in reducing transmission of infection in healthcare settings, particularly when aerosol-generating medical or dental procedures are being performed.3 The potential for aerosol spread of the virus through dental procedures, such as use of high and low-speed handpieces, ultra-sonic scalers, air/water syringes, intra-oral radiographs or an infected patient coughing, places dental HCWs at an elevated risk of infection.6 Due to the unique characteristics of dental procedures where a large number of droplets and aerosols could be generated, the standard protective measures employed in routine clinical work may not be sufficient to prevent the spread of COVID-19, especially when patients are in the incubation period and unaware of their infections status.7
Up until now, there has been no universal guidelines for dental care provision during the time of epidemics, pandemics and national disaster.7 Pandemic planning for dental services has typically involved a step-down process, with cancellation of routine care first, then urgent care, followed by the provision of solely emergency care.6 Across the globe, dental settings have prioritised urgent and emergency care and suspended elective visits and procedures to protect HCWs and patients, preserve PPE supplies and expand available hospital capacity.6,7 However, mounting demand for PPE driven not only by number of COVID-19 cases but also by misinformation, panic buying, and stockpiling has resulted in shortages of PPE globally for the HCW.5,8
A coordinated set of PPE standards and a unified design for PPE are required to protect HCW when taking care of patients with highly infectious diseases.1 Studies point out that PPE scarcity could be mitigated to an extent through identification of effective reprocessing, extended use and re-use techniques.8 Evidence indicates that respirators maintain their protection when used for extended periods.9 However, using a respirator for longer than four hours should be avoided as it can lead to discomfort.9,10 Although studies have acknowledged that extended PPE use during times of severe shortages could reduce the utilisation rate,1,8,11 the safety of such techniques in containing the infection transmission has not been extensively researched in practical settings. During previous public health emergencies involving acute respiratory illnesses, respirators such as N95, FFP2 or equivalent standard have been successfully used for extended time.11 This entailed wearing the same respirator for multiple patients with the same diagnosis without removing it.1,8 Reprocessing PPE must consider material composition, functionality post treatment, along with appropriate disinfection.2 There is scant published literature on efficacy of reprocessing PPE.
The unprecedented pandemic situation and increased PPE burn rate has created a space for healthcare digital innovation. Telemedicine and teledentistry has become part of the care delivery process in many parts of the world, thereby minimising the need for PPE use and need for people to go to healthcare facilities to seek care. A recently updated Cochrane systematic review on the effects of interactive telemedicine on professional practice and healthcare outcomes using 93 eligible trials and over 22,000 participants concluded that interactive telemedicine can lead to similar health outcomes as face-to-face delivery of care.12
Several studies including guidance, based on clinical and epidemiological data, have highlighted the need for coordinated efforts to prevent and reduce transmission of infection to HCWs.2,8,11,13 In response to the lack of evidence and appropriate PPE guidance within dentistry, in many countries, healthcare quality and safety control centres including professional associations have put forward their recommendations for dental services during the COVID-19 outbreak. Concurrently, rapid reviews have been conducted to enable policy makers to develop comprehensive national guidance for dentistry.6 The majority of the studies included in the existing rapid reviews lack underpinning evidence and some areas are unlikely to ever have strong (or any) research evidence.6 Research is urgently required to build evidence on what types of PPE, and which modifications provide most appropriate, manageable protection for members of the dental team to deliver care safely.
References
Verbeek J, Rajamaki B, Ijaz S et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev 2020: DOI: 10.1002/14651858.CD011621.pub4
Rowan N J, Laffey J G. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from Coronavirus disease (COVID19) pandemic - Case study from the Republic of Ireland. Sci Tot Environ 2020; 138: 532.
Mick P, Murphy R. Aerosol-generating otolaryngology procedures and the need for enhanced PPE during the COVID-19 pandemic: a literature review. J Otolaryngol Head Neck Surg 2020; DOI: 10.1186/s40463-020-00424-7.
World Health Organisation. Infection prevention and control of epidemic and pandemic-prone acute respiratory infections in health care; WHO guideline. Geneva, Switzerland: World Health Organization; 2014.
World Health Organisation. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19): Interim guidance. 2020.
Clarkson J, Ramsay C, Aceves M et al. Recommendations for the re-opening of dental services: a rapid review of international sources. 2020. Available at https://oralhealth.cochrane.org/sites/oralhealth.cochrane.org/files/public/uploads/covid19_dental_reopening_rapid_review_07052020.pdf (accessed May 2020).
Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res 2020; 99: 481-487.
Boškoski I, Gallo C, Wallace M, Costamagna G. COVID-19 pandemic and personal protective equipment shortage: protective efficacy comparing masks and scientific methods for respirator reuse. Gastrointest Endosc 2020; DOI: 10.1016/j.gie.2020.04.048.
Janssen L, Zhuang Z, Shaffer R. Criteria for the collection of useful respirator performance data in the workplace. J Occup Environ Hyg 2014; 11: 218-226.
Radonovich L J, Cheng J, Shenal B V, Hodgson M, Bender B S. Respirator tolerance in health care workers. JAMA 2009; 301: 36-38.
Beckman S, Materna B, Goldmacher S et al. Evaluation of respiratory protection programmes and practices in California hospitals during the 2009-2010 H1N1 influenza pandemic. Am J Infect Control 2013; 41: 1024-1031.
Flodgren G, Rachas A, Farmer A J, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015; DOI: 10.1002/14651858.CD002098.pub2.
Adams J G, Walls R M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA 2020; 323: 1439-1440.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hegde, S. Which type of personal protective equipment (PPE) and which method of donning or doffing PPE carries the least risk of infection for healthcare workers?. Evid Based Dent 21, 74–76 (2020). https://doi.org/10.1038/s41432-020-0097-3
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41432-020-0097-3
This article is cited by
-
Reusable respirators as personal protective equipment in clinical practice
Wiener klinische Wochenschrift (2022)