Abstract
Objective:
To evaluate whether early childhood body mass index (BMI) is an appropriate indicator for monogenic obesity.
Methods:
A cohort of n = 21 children living in Germany or Austria with monogenic obesity due to congenital leptin deficiency (group LEP, n = 6), leptin receptor deficiency (group LEPR, n = 6) and primarily heterozygous MC4 receptor deficiency (group MC4R, n = 9) was analyzed. A control group (CTRL) was defined that consisted of n = 22 obese adolescents with no mutation in the above mentioned genes. Early childhood (0–5 years) BMI trajectories were compared between the groups at selected time points.
Results:
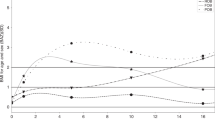
The LEP and LEPR group showed a tremendous increase in BMI during the first 2 years of life with all patients displaying a BMI >27 kg/m2 (27.2–38.4 kg/m2) and %BMIP95 (percentage of the 95th percentile BMI for age and sex) >140% (144.8–198.6%) at the age of 2 years and a BMI > 33 kg/m2 (33.3–45.9 kg/m2) and %BMIP95 > 184% (184.1–212.6%) at the age of 5 years. The MC4R and CTRL groups had a later onset of obesity with significantly lower BMI values at both time points (p < 0.01).
Conclusion:
As result of the investigation of early childhood BMI trajectories in this pediatric cohort with monogenic obesity we suggest that BMI values >27.0 kg/m2 or %BMIP95 > 140% at the age of 2 years and BMI values >33.0 kg/m2 or %BMIP95 > 184% at the age of 5 years may be useful cut points to identify children who should undergo genetic screening for monogenic obesity due to functionally relevant mutations in the leptin gene or leptin receptor gene.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–32.
NCD Risk Factor Collaboration (NCD-RisC. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Lubrano-Berthelier C, Dubern B, Lacorte JM, Picard F, Shapiro A, Zhang S, et al. Melanocortin 4 receptor mutations in a large cohort of severely obese adults: prevalence, functional classification, genotype-phenotype relationship, and lack of association with binge eating. J Clin Endocrinol Metab. 2006;91:1811–8.
Farooqi IS, Keogh JM, Yeo GS, Lank EJ, Cheetham T, O'Rahilly S. Clinical spectrum of obesity and mutations in the melanocortin 4 receptor gene. N Engl J Med. 2003;348:1085–95.
Vollbach H, Brandt S, Lahr G, Denzer C, von Schnurbein J, Debatin KM, et al. Prevalence and phenotypic characterization of MC4R variants in a large pediatric cohort. Int J Obes. 2017;41:13–22.
van der Klaauw AA, Farooqi IS. The hunger genes: pathways to obesity. Cell . 2015;161:119–32.
O'Rahilly S, Farooqi IS. Human obesity as a heritable disorder of the central control of energy balance. Int J Obes. 2005;2008:S55–61.
Farooqi IS, O'Rahilly S. 20 years of leptin: human disorders of leptin action. J Endocrinol. 2014;223:T63–70.
Funcke JB, von Schnurbein J, Lennerz B, Lahr G, Debatin KM, Fischer-Posovszky P, et al. Monogenic forms of childhood obesity due to mutations in the leptin gene. Mol Cell Pediatr. 2014;1:3.
Gibson WT, Farooqi IS, Moreau M, DePaoli AM, Lawrence E, O'Rahilly S, et al. Congenital leptin deficiency due to homozygosity for the Delta133G mutation: report of another case and evaluation of response to four years of leptin therapy. J Clin Endocrinol Metab. 2004;89:4821–6.
Wabitsch M, Funcke JB, von Schnurbein J, Denzer F, Lahr G, Mazen I, et al. Severe early-onset obesity due to bioinactive leptin caused by a p.N103K mutation in the leptin gene. J Clin Endocrinol Metab. 2015;100:3227–30.
Wabitsch M, Funcke JB, Lennerz B, Kuhnle-Krahl U, Lahr G, Debatin KM, et al. Biologically inactive leptin and early-onset extreme obesity. N Engl J Med. 2015;372:48–54.
Kühnen P, Clement K, Wiegand S, Blankenstein O, Gottesdiener K, Martini LL, et al. Proopiomelanocortin deficiency treated with a melanocortin-4 receptor agonist. N Engl J Med. 2016;375:240–6.
Montague CT, Farooqi IS, Whitehead JP, Soos MA, Rau H, Wareham NJ, et al. Congenital leptin deficiency is associated with severe early-onset obesity in humans. Nature. 1997;387:903–8.
Wabitsch M, Pridzun L, Ranke M, von Schnurbein J, Moss A, Brandt S, et al. Measurement of immunofunctional leptin to detect and monitor patients with functional leptin deficiency. Eur J Endocrinol. 2017;176:315–22.
Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity . 2009;17:941–64.
Puhl RM, Andreyeva T, Brownell KD. Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int J Obes. 2005;32:992–1000.
Wiegand S, Krude H. [Monogenic and syndromic symptoms of morbid obesity. Rare but important]. DerInternist. 2015;56:111–2. 114–20
Dubern B, Bisbis S, Talbaoui H, Le Beyec J, Tounian P, Lacorte JM, et al. Homozygous null mutation of the melanocortin-4 receptor and severe early-onset obesity. J Pediatr. 2007;150:613–7. 617.e1
Huvenne H, Le Beyec J, Pepin D, Alili R, Kherchiche PP, Jeannic E, et al. Seven novel deleterious LEPR mutations found in early-onset obesity: a DeltaExon6-8 shared by subjects from Reunion Island, France, suggests a founder effect. J Clin Endocrinol Metab. 2015;100:E757–66.
Kromeyer-Hauschild K, Wabitsch M, Kunze D, Geller F, Geiß HC, Hesse V, et al. Perzentile für den Body-mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Mon Kinderheilkd. 2001;149:807–18.
Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, et al. Pediatric obesity-assessment, treatment, and prevention: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2017;102:709–57.
von Schnurbein J, Moss A, Nagel SA, Muehleder H, Debatin KM, Farooqi IS, et al. Leptin substitution results in the induction of menstrual cycles in an adolescent with leptin deficiency and hypogonadotropic hypogonadism. Horm Res Paediatr. 2012;77:127–33.
Voigt M, Rochow N, Schneider KT, Hagenah HP, Scholz R, Hesse V, et al. [New percentile values for the anthropometric dimensions of singleton neonates: analysis of perinatal survey data of 2007-2011 from all 16 states of Germany]. Z Geburtshilfe Neonatol. 2014;218:210–7.
Farooqi IS, Wangensteen T, Collins S, Kimber W, Matarese G, Keogh JM, et al. Clinical and molecular genetic spectrum of congenital deficiency of the leptin receptor. N Engl J Med. 2007;356:237–47.
Farooqi IS, Jebb SA, Langmack G, Lawrence E, Cheetham CH, Prentice AM, et al. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N Engl J Med. 1999;341:879–84.
Tao YX. Molecular mechanisms of the neural melanocortin receptor dysfunction in severe early onset obesity. Mol Cell Endocrinol. 2005;239:1–14.
Stutzmann F, Tan K, Vatin V, Dina C, Jouret B, Tichet J, et al. Prevalence of melanocortin-4 receptor deficiency in Europeans and their age-dependent penetrance in multigenerational pedigrees. Diabetes. 2008;57:2511–8.
Delhanty PJ, Bouw E, Huisman M, Vervenne RM, Themmen AP, van der Lely AJ, et al. Functional characterization of a new human melanocortin-4 receptor homozygous mutation (N72K) that is associated with early-onset obesity. Mol Biol Rep. 2014;41:7967–72.
Freedman DS, Butte NF, Taveras EM, Goodman AB, Ogden CL, Blanck HM. The limitations of transforming very high body mass indexes into z-scores among 8.7 million 2- to 4-year-old children. J Pediatr. 2017;188:50–56.e1.
Freedman DS, Butte NF, Taveras EM, Lundeen EA, Blanck HM, Goodman AB, et al. BMI z-scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999-2000 to 2013-2014. Obesity. 2017;25:739–46.
Cole TJ. The LMS method for constructing normalized growth standards. Eur J Clin Nutr. 1990;44:45–60.
Strobel A, Issad T, Camoin L, Ozata M, Strosberg AD. A leptin missense mutation associated with hypogonadism and morbid obesity. Nat Genet. 1998;18:213–5.
Ozata M, Ozdemir IC, Licinio J. Human leptin deficiency caused by a missense mutation: multiple endocrine defects, decreased sympathetic tone, and immune system dysfunction indicate new targets for leptin action, greater central than peripheral resistance to the effects of leptin, and spontaneous correction of leptin-mediated defects. J Clin Endocrinol Metab. 1999;84:3686–95.
Fischer-Posovszky P, von Schnurbein J, Moepps B, Lahr G, Strauss G, Barth TF, et al. A new missense mutation in the leptin gene causes mild obesity and hypogonadism without affecting T cell responsiveness. J Clin Endocrinol Metab. 2010;95:2836–40.
Shabana HasnainS. The p. N103K mutation of leptin (LEP) gene and severe early onset obesity in Pakistan. Biol Res. 2016;49:23.
Mazen I, El-Gammal M, Abdel-Hamid M, Amr K. A novel homozygous missense mutation of the leptin gene (N103K) in an obese Egyptian patient. Mol Genet Metab. 2009;97:305–8.
Andiran N, Celik N, Andiran F. Homozygosity for two missense mutations in the leptin receptor gene (P316:W646C) in a Turkmenian girl with severe early-onset obesity. J Pediatr Endocrinol. 2011;24:1043–5.
Larsen LH, Echwald SM, Sorensen TI, Andersen T, Wulff BS, Pedersen O. Prevalence of mutations and functional analyses of melanocortin 4 receptor variants identified among 750 men with juvenile-onset obesity. J Clin Endocrinol Metab. 2005;90:219–24.
Xiang Z, Proneth B, Dirain ML, Litherland SA, Haskell-Luevano C. Pharmacological characterization of 30 human melanocortin-4 receptor polymorphisms with the endogenous proopiomelanocortin-derived agonists, synthetic agonists, and the endogenous agouti-related protein antagonist. Biochemistry. 2010;49:4583–600.
Biebermann H, Krude H, Elsner A, Chubanov V, Gudermann T, Gruters A. Autosomal-dominant mode of inheritance of a melanocortin-4 receptor mutation in a patient with severe early-onset obesity is due to a dominant-negative effect caused by receptor dimerization. Diabetes. 2003;52:2984–8.
Hinney A, Hohmann S, Geller F, Vogel C, Hess C, Wermter AK, et al. Melanocortin- 4 receptor gene: case-control study and transmission disequilibrium test confirm that functionally relevant mutations are compatible with a major gene effect for extreme obesst. J Clin Endocrinol Metab. 2003;88:4258–67.
Lubrano-Berthelier C, Durand E, Dubern B, Shapiro A, Dazin P, Weill J, et al. Intracellular retention is a common characteristic of childhood obesity-associated MC4R mutations. Hum Mol Genet. 2003;12:145–53.
Demiralp DO, Berberoglu M, Akar N. Melanocortin-4 receptor polymorphisms in Turkish pediatric obese patients. Clin Appl Thromb Hemost. 2011;17:70–4.
Valli-Jaakola K, Lipsanen-Nyman M, Oksanen L, Hollenberg AN, Kontula K, Bjorbaek C, et al. Identification and characterization of melanocortin-4 receptor gene mutations in morbidly obese finnish children and adults. J Clin Endocrinol Metab. 2004;89:940–5.
Acknowledgements
Funding
The study was funded by the German Ministry of Education and Research (BMBF) and is integrated in the Competence Network Obesity (FKZ 01GI1120A).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kohlsdorf, K., Nunziata, A., Funcke, JB. et al. Early childhood BMI trajectories in monogenic obesity due to leptin, leptin receptor, and melanocortin 4 receptor deficiency. Int J Obes 42, 1602–1609 (2018). https://doi.org/10.1038/s41366-018-0049-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0049-6
This article is cited by
-
Child and adolescent obesity
Nature Reviews Disease Primers (2023)
-
Rare genetic forms of obesity in childhood and adolescence, a comprehensive review of their molecular mechanisms and diagnostic approach
European Journal of Pediatrics (2023)
-
Congenital leptin and leptin receptor deficiencies in nine new families: identification of six novel variants and review of literature
Molecular Genetics and Genomics (2023)
-
The Uterine Environment and Childhood Obesity Risk: Mechanisms and Predictions
Current Nutrition Reports (2023)
-
Interaction of MC4R rs17782313 variants and dietary carbohydrate quantity and quality on basal metabolic rate and general and central obesity in overweight/obese women: a cross-sectional study
BMC Endocrine Disorders (2022)