Key Points
-
Gender-confirming surgery is becoming a more frequently encountered procedure for urologists, plastic surgeons, and gynaecologists
-
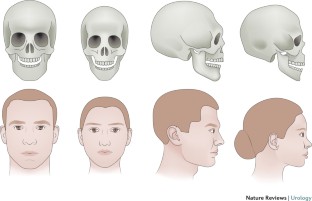
Female-to-male gender-confirming surgery consists of facial masculinization, chest masculinization, body contouring, and genital surgery
-
Metoidioplasty (hypertrophy with systemic hormones and mobilization of the clitoris with urethroplasty) can produce a sensate microphallus
-
Phalloplasty can produce an aesthetic and sensate phallus with ability to micturate in a standing position and engage in penetrative sexual intercourse if proper nerve coaptation and prosthetic insertion are performed
-
Urethral complications following genital surgery in transmen are generally higher than 30% and include urethral fistulas and strictures; revisional urethroplasty can address most urethral complications following genital surgery
-
Advances in basic sciences, transgender-specific prostheses, and patient-reported outcomes will continue to offer options for improvements in gender-confirming surgery
Abstract
Gender dysphoria is estimated to occur in approximately 25 million people worldwide, and can have severe psychosocial sequelae. Medical and surgical gender transition can substantially improve quality-of-life outcomes for individuals with gender dysphoria. Individuals seeking to undergo female-to-male (FtM) transition have various surgical options available for gender confirmation, including facial and chest masculinization, body contouring, and genital surgery. The World Professional Association for Transgender Health guidelines should be met before the patient undergoes surgery, to ensure that gender-confirming surgery is appropriate and indicated. Chest masculinization and metoidioplasty or phalloplasty are the most common procedures pursued, and both generally result in high levels of patient satisfaction. Phalloplasty, with a resultant aesthetic and sensate phallus along with implantable prosthetic, can take upwards of a year to accomplish, and is associated with a considerable risk of complications. Urethral complications are most frequent, and can be addressed with revision procedures. A number of scaffolds, implants, and prostheses are now in development to improve outcomes in FtM patients.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. 7th Version (World Professional Association for Transgender Health, 2011). Standards of care for transgender and gender nonconforming patients to assist all providers caring for patients within this population.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Benjamin, H. The Transsexual Phenomenon (Julian Press, 1966).
Byne, W. et al. Report of the American Psychiatric Association task force on treatment of gender identity disorder. Arch. Sex. Behav. 41, 759–796 (2012).
Dhejne, C. et al. Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS ONE 6, e16885 (2011).
Dhejne, C., Oberg, K., Arver, S. & Landen, M. An analysis of all applications for sex reassignment surgery in Sweden, 1960-2010: prevalence, incidence, and regrets. Arch. Sex. Behav. 43, 1535–1545 (2014).
Lawrence, A. A. Gender assignment dysphoria in the DSM-5. Arch. Sex. Behav. 43, 1263–1266 (2014).
Leiter, E., Futterweit, W. & Brown, G. R. in Reconstructive Urology Vol. 2 (eds Webster, G., Kirby, R., King, L. & Goldwasser, B.) 921–932 (Blackwell Scientific Publications, 1993).
Winter, S. et al. Transgender people: health at the margins of society. Lancet 388, 390–400 (2016). Evaluation of the difficulties experienced by transgender patients in seeking healthcare.
Wylie, K. et al. Serving transgender people: clinical care considerations and service delivery models in transgender health. Lancet 388, 401–411 (2016).
Gooren, L. J. Clinical practice. Care of transsexual persons. N. Engl. J. Med. 364, 1251–1257 (2011).
Deutsch, M. B. et al. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J. Am. Med. Inform. Assoc. 20, 700–703 (2013).
Morrison, S. D. The care transition in plastic surgery. Plast. Reconstr. Surg. 136, 861e–862e (2015).
Morrison, S. D. & Swanson, J. W. Surgical justice. Plast. Reconstr. Surg. 136, 291e–292e (2015).
De Cuypere, G., Elaut, E. & Heylens, G. Long-term follow-up: psychosocial outcome of Belgian transsexuals after sex reassignment surgery. Sexologies 15, 126–133 (2006).
De Cuypere, G. et al. Sexual and physical health after sex reassignment surgery. Arch. Sex. Behav. 34, 679–690 (2005).
Hage, J. J. & Karim, R. B. Ought GIDNOS get nought? Treatment options for nontranssexual gender dysphoria. Plast. Reconstr. Surg. 105, 1222–1227 (2000).
Lawrence, A. A. Sexuality before and after male-to-female sex reassignment surgery. Arch. Sex. Behav. 34, 147–166 (2005).
Wierckx, K. et al. Sexual desire in female-to-male transsexual persons: exploration of the role of testosterone administration. Eur. J. Endocrinol. 165, 331–337 (2011).
Wierckx, K. et al. Sexual desire in trans persons: associations with sex reassignment treatment. J. Sex. Med. 11, 107–118 (2014). Evaluation of the sexual desires experienced by transgender patients after gender-confirming surgery.
Wierckx, K. et al. Long-term evaluation of cross-sex hormone treatment in transsexual persons. J. Sex. Med. 9, 2641–2651 (2012).
Wierckx, K. et al. Quality of life and sexual health after sex reassignment surgery in transsexual men. J. Sex. Med. 8, 3379–3388 (2011).
Zaker-Shahrak, A., Chio, L. W., Isaac, R. & Tescher, J. Economic impact assessment: Gender nondiscrimination in health insurance. (ed. Department of Insurance) (State of California, 2012).
Monstrey, S. et al. Surgical therapy in transsexual patients: a multi-disciplinary approach. Acta Chir. Belg. 101, 200–209 (2001).
Selvaggi, G., Dhejne, C., Landen, M. & Elander, A. The 2011 WPATH standards of care and penile reconstruction in female-to-male transsexual individuals. Adv. Urol. 2012, 581712 (2012).
Gooren, L. J. Management of female-to-male transgender persons: medical and surgical management, life expectancy. Curr. Opin. Endocrinol. Diabetes Obes. 21, 233–238 (2014).
Davis, S. R. et al. Testosterone for low libido in postmenopausal women not taking estrogen. N. Engl. J. Med. 359, 2005–2017 (2008).
Gooren, L. J. & Giltay, E. J. Review of studies of androgen treatment of female-to-male transsexuals: effects and risks of administration of androgens to females. J. Sex. Med. 5, 765–776 (2008).
Gooren, L. J., Giltay, E. J. & Bunck, M. C. Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience. J. Clin. Endocrinol. Metab. 93, 19–25 (2008).
Mueller, A. & Gooren, L. Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. Eur. J. Endocrinol. 159, 197–202 (2008).
Van Caenegem, E. et al. Bone mass, bone geometry, and body composition in female-to-male transsexual persons after long-term cross-sex hormonal therapy. J. Clin. Endocrinol. Metab. 97, 2503–2511 (2012).
Monstrey, S. J., Ceulemans, P. & Hoebeke, P. Sex reassignment surgery in the female-to-male transsexual. Semin. Plast. Surg. 25, 229–244 (2011).
Morrison, S. D., Perez, M. G., Carter, C. K. & Crane, C. N. Pre- and post-operative care with associated intra-operative techniques for phalloplasty in female-to-male patients. Urol. Nurs. 35, 134–138 (2015).
Morrison, S. D., Perez, M. G., Nedelman, M. & Crane, C. N. Current state of female-to-male gender confirming surgery. Curr. Sex. Health Rep. 7, 38–48 (2015).
Selvaggi, G. & Bellringer, J. Gender reassignment surgery: an overview. Nat. Rev. Urol. 8, 274–282 (2011).
Morrison, S. D. et al. Educational exposure to transgender patient care in plastic surgery training. Plast. Reconstr. Surg. 138, 944–953 (2016). Evaluation of resident exposure to transgender patient care in plastic surgery.
Obedin-Maliver, J. et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA 306, 971–977 (2011).
Dy, G. W. et al. Exposure to and attitudes regarding transgender education among urology residents. J. Sex. Med. 13, 1466–1472 (2016). Evaluation of resident exposure to transgender patient care in urology.
Morrison, S. D. et al. Facial feminization: systematic review of the literature. Plast. Reconstr. Surg. 137, 1759–1770 (2016).
Ousterhout, D. K. Dr. Paul Tessier and facial skeletal masculinization. Ann. Plast. Surg. 67, S10–S15 (2011).
Deschamps-Braly, J. C., Sacher, C. L., Fick, J. & Ousterhout, D. K. First female-to-male facial confirmation surgery with description of a new procedure for masculinization of the thyroid cartilage (Adam's apple). Plast. Reconstr. Surg. 139, 883e–887e (2017). First report of facial masculinization in transmen.
Monstrey, S. et al. Chest-wall contouring surgery in female-to-male transsexuals: a new algorithm. Plast. Reconstr. Surg. 121, 849–859 (2008). Algorithmic approach to chest wall masculinization.
Richards, C. & Barrett, J. The case for bilateral mastectomy and male chest contouring for the female-to-male transsexual. Ann. R. Coll. Surg. Engl. 95, 93–95 (2013).
Berry, M. G., Curtis, R. & Davies, D. Female-to-male transgender chest reconstruction: a large consecutive, single-surgeon experience. J. Plast. Reconstr. Aesthet. Surg. 65, 711–719 (2012).
Colic, M. M. & Colic, M. M. Circumareolar mastectomy in female-to-male transsexuals and large gynecomastias: a personal approach. Aesthetic Plast. Surg. 24, 450–454 (2000).
Nelson, L., Whallett, E. J. & McGregor, J. C. Transgender patient satisfaction following reduction mammaplasty. J. Plast. Reconstr. Aesthet. Surg. 62, 331–334 (2009).
Vukadinovic, V., Stojanovic, B., Majstorovic, M. & Milosevic, A. The role of clitoral anatomy in female to male sex reassignment surgery. ScientificWorldJournal 2014, 437378 (2014).
Weyers, S. et al. Gynaecological aspects of the treatment and follow-up of transsexual men and women. Facts Views Vis. Obgyn. 2, 35–54 (2010).
Ergeneli, M. H., Duran, E. H., Ozcan, G. & Erdogan, M. Vaginectomy and laparoscopically assisted vaginal hysterectomy as adjunctive surgery for female-to-male transsexual reassignment: preliminary report. Eur. J. Obstet. Gynecol. Reprod. Biol. 87, 35–37 (1999).
Weyers, S., Selvaggi, G. & Monstrey, S. Two-stage versus one-stage sex reassignment surgery in female-to-male transsexual individuals. Gynecol. Surg. 3, 190–194 (2006).
Morrison, S. D. et al. Phalloplasty: a review of techniques and outcomes. Plast. Reconstr. Surg. 138, 594–615 (2016). Contemporary evaluation of techniques and outcomes of phalloplasty.
Perrone, A. M. et al. Hysterectomy and bilateral salpingoovariectomy in a transsexual subject without visible scaring. Diagn. Ther. Endosc. 2010, 845029 (2010).
Chen, Y. J. et al. Single-port compared with conventional laparoscopic-assisted vaginal hysterectomy: a randomized controlled trial. Obstet. Gynecol. 117, 906–912 (2011).
Bogliolo, S. et al. Robotic single-site surgery for female-to-male transsexuals: preliminary experience. ScientificWorldJournal 2014, 674579 (2014).
Obedin-Maliver, J., Light, A., Dehaan, G., Steinauer, J. & Jackson, R. Vaginal hysterectomy as a viable option for female-to-male transgender men. Obstet. Gynecol. 123 (Suppl. 1), 126S–127S (2014).
Djordjevic, M. L. et al. Urethral lengthening in metoidioplasty (female-to-male sex reassignment surgery) by combined buccal mucosa graft and labia minora flap. Urology 74, 349–353 (2009).
Djordjevic, M. L. & Bizic, M. R. Comparison of two different methods for urethral lengthening in female to male (metoidioplasty) surgery. J. Sex. Med. 10, 1431–1438 (2013). Assessment of outcomes of urethral lengthening following metoidioplasty.
Zhang, Y. F. et al. Is vaginal mucosal graft the excellent substitute material for urethral reconstruction in female-to-male transsexuals? World J. Urol. 33, 2115–2123 (2015).
Hage, J. J. & Bloem, J. J. Review of the literature on construction of a neourethra in female-to-male transsexuals. Ann. Plast. Surg. 30, 278–286 (1993).
Hage, J. J., Bouman, F. G. & Bloem, J. J. Construction of the fixed part of the neourethra in female-to-male transsexuals: experience in 53 patients. Plast. Reconstr. Surg. 91, 904–910 (1993).
Rohrmann, D. & Jakse, G. Urethroplasty in female-to-male transsexuals. Eur. Urol. 44, 611–614 (2003).
Selvaggi, G. & Elander, A. Penile reconstruction/formation. Curr. Opin. Urol. 18, 589–597 (2008).
Salgado, C. J., Chim, H., Tang, J. C., Monstrey, S. J. & Mardini, S. Penile reconstruction. Semin. Plast. Surg. 25, 221–228 (2011).
Hage, J. J. & De Graaf, F. H. Addressing the ideal requirements by free flap phalloplasty: some reflections on refinements of technique. Microsurgery 14, 592–598 (1993).
Monstrey, S. et al. Penile reconstruction: is the radial forearm flap really the standard technique? Plast. Reconstr. Surg. 124, 510–518 (2009). Largest evaluation of outcomes of RFFF phalloplasty.
Zhang, W. R., Garrett, G. L., Arron, S. T. & Garcia, M. M. Laser hair removal for genital gender affirming surgery. Transl Androl. Urol. 5, 381–387 (2016).
Durfee, R. & Rowland, W. in Proceedings of the Second Interdisciplinary Symposium on Gender Dysphoria Syndrome (eds Laub, D. R. & Gandy, P.) 181–183 (Stanford Univ. Press, 1973).
Lebovic, G. S. & Laub, D. R. in Reconstructive and Plastic Surgery of the External Genitalia (eds Ehrlich, R. M. & Alter, G. J.) 355–360 (WB Saunders, 1999).
Hage, J. J. Metaidoioplasty: an alternative phalloplasty technique in transsexuals. Plast. Reconstr. Surg. 97, 161–167 (1996).
Hage, J. J. & van Turnhout, A. A. Long-term outcome of metaidoioplasty in 70 female-to-male transsexuals. Ann. Plast. Surg. 57, 312–316 (2006).
Oakley, S. H. et al. Innervation and histology of the clitoral-urethal complex: a cross-sectional cadaver study. J. Sex. Med. 10, 2211–2218 (2013).
Djordjevic, M. L. et al. Metoidioplasty as a single stage sex reassignment surgery in female transsexuals: Belgrade experience. J. Sex. Med. 6, 1306–1313 (2009).
Perovic, S. V. & Djordjevic, M. L. Metoidioplasty: a variant of phalloplasty in female transsexuals. BJU Int. 92, 981–985 (2003).
Takamatsu, A. & Harashina, T. Labial ring flap: a new flap for metaidoioplasty in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62, 318–325 (2009).
Bogoras, N. Über die volle plastische Wiederherstellung eines zum Koitus fähigen Penis (Peniplastica totalis) [German]. Zentralbl. Chir. 63, 1271–1276 (1936).
Gillies, H. & Millard, R. The Principles and Art of Plastic Surgery Vol. II 369–388 (Little, Brown and Company, 1957).
Kaplan, I. A rapid method for constructing a functional sensitive penis. Br. J. Plast. Surg. 24, 342–344 (1971).
Puckett, C. L., Reinisch, J. F. & Montie, J. E. Free flap phalloplasty. J. Urol. 128, 294–297 (1982).
Hu, W. et al. A preliminary report of penile transplantation: part 2. Eur. Urol. 50, 1115–1116 (2006).
Hu, W. et al. A preliminary report of penile transplantation. Eur. Urol. 50, 851–853 (2006).
Morrison, S. D. et al. Penile replantation: a retrospective analysis of outcomes and complications. J. Reconstr. Microsurg. 33, 227–232 (2017).
Monstrey, S. et al. Radial forearm phalloplasty: a review of 81 cases. Eur. J. Plast. Surg. 28, 206–212 (2005).
Bettocchi, C., Ralph, D. J. & Pryor, J. P. Pedicled pubic phalloplasty in females with gender dysphoria. BJU Int. 95, 120–124 (2005).
Shaeer, O. & El-Sebaie, A. Construction of neoglans penis: a new sculpturing technique from rectus abdominis myofascial flap. J. Sex. Med. 2, 259–265 (2005).
Terrier, J. E., Courtois, F., Ruffion, A. & Morel Journel, N. Surgical outcomes and patients' satisfaction with suprapubic phalloplasty. J. Sex. Med. 11, 288–298 (2014).
Alanis, S. Z. An innovation in total penis reconstruction. Plast. Reconstr. Surg. 43, 418–422 (1969).
Davies, D. Phalloplasty. S. Afr. Med. J. 31, 990–991 (1957).
Davies, D. M. & Matti, B. A. A method of phalloplasty using the deep inferior epigastric flap. Br. J. Plast. Surg. 41, 165–168 (1988).
Dubin, B. J., Sato, R. M. & Laub, D. R. Results of phalloplasty. Plast. Reconstr. Surg. 64, 163–170 (1979).
Santi, P. et al. Immediate reconstruction of the penis using an inferiorly based rectus abdominis myocutaneous flap. Plast. Reconstr. Surg. 81, 961–964 (1988).
Zhang, Y., Lu, L., Zhang, W., Jiang, H. & Zhu, X. A simple and effective method for phalloplasty in female-to-male transsexuals. Plast. Reconstr. Surg. 126, 264e–265e (2010).
Lumen, N., Hoebeke, P. & Oosterlinck, W. Urethroplasty for urethral strictures: quality assessment of an in-home algorithm. Int. J. Urol. 17, 167–174 (2010).
Krauss, E. M., Tung, T. H. & Moore, A. M. Free functional muscle transfers to restore upper extremity function. Hand Clin. 32, 243–256 (2016).
Ranno, R. et al. Neo-phalloplasty with re-innervated latissimus dorsi free flap: a functional study of a novel technique. Acta Chir. Plast. 49, 3–7 (2007).
Ranno, R., Hyza, P., Vesely, J., Dessy, L. A. & Kadanka, Z. An objective evaluation of contraction power of neo-phallus reconstructed with free re-innervated LD in female-to-male transsexuals. Acta Chir. Plast. 49, 8–12 (2007).
Mori, R. L. & Angermeier, K. W. Staged urethroplasty in the management of complex anterior urethral stricture disease. Transl Androl. Urol. 4, 29–34 (2015).
Djordjevic, M. L., Bumbasirevic, M. Z., Vukovic, P. M., Sansalone, S. & Perovic, S. V. Musculocutaneous latissimus dorsi free transfer flap for total phalloplasty in children. J. Pediatr. Urol. 2, 333–339 (2006).
Lin, C. T. & Chen, L. W. Using a free thoracodorsal artery perforator flap for phallic reconstruction — a report of surgical technique. J. Plast. Reconstr. Aesthet. Surg. 62, 402–408 (2009).
Perovic, S. V., Djinovic, R., Bumbasirevic, M., Djordjevic, M. & Vukovic, P. Total phalloplasty using a musculocutaneous latissimus dorsi flap. BJU Int. 100, 899–905 (2007).
Vesely, J. et al. New technique of total phalloplasty with reinnervated latissimus dorsi myocutaneous free flap in female-to-male transsexuals. Ann. Plast. Surg. 58, 544–550 (2007).
Kessler, T. M. et al. Long-term results of surgery for urethral stricture: a statistical analysis. J. Urol. 170, 840–844 (2003).
Mathur, R. K. et al. Single-stage preputial skin flap urethroplasty for long-segment urethral strictures: evaluation and determinants of success. BJU Int. 113, 120–126 (2014).
Taguchi, H., Saito, K. & Yamada, T. A simple method of total reconstruction of the penis. Case reports. Plast. Reconstr. Surg. 60, 454–456 (1977).
Hage, J. J., Winters, H. A. & Van Lieshout, J. Fibula free flap phalloplasty: modifications and recommendations. Microsurgery 17, 358–365 (1996).
Sadove, R. C., Sengezer, M., McRoberts, J. W. & Wells, M. D. One-stage total penile reconstruction with a free sensate osteocutaneous fibula flap. Plast. Reconstr. Surg. 92, 1314–1323 (1993).
McRoberts, J. W. & Sadove, R. C. Penile reconstruction with a free sensate osteocutaneous fibula flap in the surgical management of the intersex patient. Adv. Exp. Med. Biol. 511, 283–287 (2002).
Sengezer, M., Ozturk, S., Deveci, M. & Odabasi, Z. Long-term follow-up of total penile reconstruction with sensate osteocutaneous free fibula flap in 18 biological male patients. Plast. Reconstr. Surg. 114, 439–450 (2004).
Dabernig, J., Chan, L. K. & Schaff, J. Phalloplasty with free (septocutaneous) fibular flap sine fibula. J. Urol. 176, 2085–2088 (2006).
Papadopulos, N. A., Schaff, J. & Biemer, E. The use of free prelaminated and sensate osteofasciocutaneous fibular flap in phalloplasty. Injury 39 (Suppl. 3), S62–S67 (2008).
Salgado, C. J., Rampazzo, A., Xu, E. & Chen, H. C. Treatment of dyspareunia by creation of a pseudojoint in rigid bone following total penile reconstruction with fibular osteocutaneous flap. J. Sex. Med. 5, 2947–2950 (2008).
Sun, G. C. & Huang, J. J. One-stage reconstruction of the penis with composite iliac crest and lateral groin skin flap. Ann. Plast. Surg. 15, 519–528 (1985).
Cutting, C. B. & McCarthy, J. G. Comparison of residual osseous mass between vascularized and nonvascularized onlay bone transfers. Plast. Reconstr. Surg. 72, 672–675 (1983).
Weiland, A. J., Phillips, T. W. & Randolph, M. A. Bone grafts: a radiologic, histologic, and biomechanical model comparing autografts, allografts, and free vascularized bone grafts. Plast. Reconstr. Surg. 74, 368–379 (1984).
Zielinski, T. Phalloplasty using a lateral groin flap in female-to-male transsexuals. Acta Chir. Plast. 41, 15–19 (1999).
Akoz, T., Erdogan, B., Gorgu, M., Kapucu, M. R. & Kargi, E. Penile reconstruction in children using a double vascular pedicle composite groin flap. Scand. J. Urol. Nephrol. 32, 225–230 (1998).
Akoz, T. & Kargi, E. Phalloplasty in a female-to-male transsexual using a double-pedicle composite groin flap. Ann. Plast. Surg. 48, 423–427 (2002).
Puckett, C. L. & Montie, J. E. Construction of male genitalia in the transsexual, using a tubed groin flap for the penis and a hydraulic inflation device. Plast. Reconstr. Surg. 61, 523–530 (1978).
Felici, N. & Felici, A. A new phalloplasty technique: the free anterolateral thigh flap phalloplasty. J. Plast. Reconstr. Aesthet. Surg. 59, 153–157 (2006).
Lee, G. K., Lim, A. F. & Bird, E. T. A novel single-flap technique for total penile reconstruction: the pedicled anterolateral thigh flap. Plast. Reconstr. Surg. 124, 163–166 (2009).
Hasegawa, K., Namba, Y. & Kimata, Y. Phalloplasty with an innervated island pedicled anterolateral thigh flap in a female-to-male transsexual. Acta Med. Okayama 67, 325–331 (2013).
Morrison, S. D. et al. Modification of the tube-in-tube pedicled anterolateral thigh flap for total phalloplasty: the mushroom flap. Ann. Plast. Surg. 72 (Suppl. 1), S22–S26 (2014).
Mutaf, M. A new surgical procedure for phallic reconstruction: Istanbul flap. Plast. Reconstr. Surg. 105, 1361–1370 (2000).
Hoebeke, P. B. et al. Erectile implants in female-to-male transsexuals: our experience in 129 patients. Eur. Urol. 57, 334–340 (2010).
Lumen, N. et al. Erectile implants in female-to-male transsexuals: our experience in 130 patients [abstract]. Eur. Urol. Suppl. 7, 117 (2008).
Neuville, P. et al. Surgical outcomes of erectile implants after phalloplasty: retrospective analysis of 95 procedures. J. Sex. Med. 13, 1758–1764 (2016). Recent evaluation of outcomes of prosthetics in phalloplasty.
Gurjala, A. N., Nazerali, R. S., Salim, A. & Lee, G. K. World's first baby born through natural insemination by father with total phalloplasty reconstruction. Ann. Plast. Surg. 76 (Suppl. 3), S179–S183 (2016).
Sinove, Y. et al. Preoperative planning of a pedicled anterolateral thigh (ALT) flap for penile reconstruction with the multidetector CT scan. Handchir. Mikrochir. Plast. Chir. 45, 217–222 (2013).
Liu, C. Y., Wei, Z. R., Jiang, H., Zhao, Y. Z. & Zhang, Y. F. Preconstruction of the pars pendulans urethrae for phalloplasty with digestive mucosa using a prefabricated anterolateral thigh flap in a one-arm patient. Plast. Reconstr. Surg. Glob. Open 1, e53 (2013).
Rubino, C. et al. Innervated island pedicled anterolateral thigh flap for neo-phallic reconstruction in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62, e45–e49 (2009).
Chang, T. S. & Hwang, W. Y. Forearm flap in one-stage reconstruction of the penis. Plast. Reconstr. Surg. 74, 251–258 (1984).
Monstrey, S. et al. Radial Forearm Phalloplasty: a Review of 91 Cases. ANIR-ANHP 6, 193–199 (2004).
Selvaggi, G. et al. Genital sensitivity after sex reassignment surgery in transsexual patients. Ann. Plast. Surg. 58, 427–433 (2007). Evaluation of genital sensitivity following phalloplasty for transmen.
Fang, R. H., Kao, Y. S., Ma, S. & Lin, J. T. Phalloplasty in female-to-male transsexuals using free radial osteocutaneous flap: a series of 22 cases. Br. J. Plast. Surg. 52, 217–222 (1999).
Kim, S. K. et al. The etiology and treatment of the softened phallus after the radial forearm osteocutaneous free flap phalloplasty. Arch. Plast. Surg. 39, 390–396 (2012).
Trost, L., Wanzek, P. & Bailey, G. A practical overview of considerations for penile prosthesis placement. Nat. Rev. Urol. 13, 33–46 (2016).
Biemer, E. Penile construction by the radial arm flap. Clin. Plast. Surg. 15, 425–430 (1988).
Doornaert, M. et al. Penile reconstruction with the radial forearm flap: an update. Handchir. Mikrochir. Plast. Chir. 43, 208–214 (2011).
Matti, B. A., Matthews, R. N. & Davies, D. M. Phalloplasty using the free radial forearm flap. Br. J. Plast. Surg. 41, 160–164 (1988).
Salgado, C. J. et al. Immediate pedicled gracilis flap in radial forearm flap phalloplasty for transgender male patients to reduce urinary fistula. J. Plast. Reconstr. Aesthet. Surg. 69, 1551–1557 (2016).
Selvaggi, G. et al. Donor-site morbidity of the radial forearm free flap after 125 phalloplasties in gender identity disorder. Plast. Reconstr. Surg. 118, 1171–1177 (2006).
Bardsley, A. F., Soutar, D. S., Elliot, D. & Batchelor, A. G. Reducing morbidity in the radial forearm flap donor site. Plast. Reconstr. Surg. 86, 287–292 (1990).
Boorman, J. G., Brown, J. A. & Sykes, P. J. Morbidity in the forearm flap donor arm. Br. J. Plast. Surg. 40, 207–212 (1987).
Richardson, D., Fisher, S. E., Vaughan, E. D. & Brown, J. S. Radial forearm flap donor-site complications and morbidity: a prospective study. Plast. Reconstr. Surg. 99, 109–115 (1997).
Van Caenegem, E. et al. Long-term evaluation of donor-site morbidity after radial forearm flap phalloplasty for transsexual men. J. Sex. Med. 10, 1644–1651 (2013).
Rieger, U. M. et al. Comparative study of the free microvascular groin flap: optimizing the donor site after free radial forearm flap phalloplasty. Urology 95, 192–196 (2016).
Fang, R. H., Lin, J. T. & Ma, S. Phalloplasty for female transsexuals with sensate free forearm flap. Microsurgery 15, 349–352 (1994).
Gottlieb, L. J. & Levine, L. A. A new design for the radial forearm free-flap phallic construction. Plast. Reconstr. Surg. 92, 276–283 (1993).
Hage, J. J., Bouman, F. G., de Graaf, F. H. & Bloem, J. J. Construction of the neophallus in female-to-male transsexuals: the Amsterdam experience. J. Urol. 149, 1463–1468 (1993).
Kim, S. K., Lee, K. C., Kwon, Y. S. & Cha, B. H. Phalloplasty using radial forearm osteocutaneous free flaps in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62, 309–317 (2009).
Koshima, I., Tai, T. & Yamasaki, M. One-stage reconstruction of the penis using an innervated radial forearm osteocutaneous flap. J. Reconstr. Microsurg. 3, 19–26 (1986).
Leriche, A. et al. Long-term outcome of forearm flee-flap phalloplasty in the treatment of transsexualism. BJU Int. 101, 1297–1300 (2008).
Ma, S., Cheng, K. & Liu, Y. Sensibility following innervated free radial forearm flap for penile reconstruction. Plast. Reconstr. Surg. 127, 235–241 (2011).
Ma, S., Liu, Y., Chang, T. & Cheng, K. Long-term follow-up of sensation recovery of the penis reconstructed by Cheng's method. Plast. Reconstr. Surg. 127, 1546–1552 (2011).
Papadopulos, N. A., Schaff, J. & Biemer, E. Usefulness of free sensate osteofasciocutaneous forearm and fibula flaps for neophallus construction. J. Reconstr. Microsurg. 17, 407–412 (2001).
Sasaki, K., Nozaki, M., Morioka, K. & Huang, T. T. Penile reconstruction: combined use of an innervated forearm osteocutaneous flap and big toe pulp. Plast. Reconstr. Surg. 104, 1054–1058 (1999).
Song, C., Wong, M., Wong, C. H. & Ong, Y. S. Modifications of the radial forearm flap phalloplasty for female-to-male gender reassignment. J. Reconstr. Microsurg. 27, 115–120 (2011).
Vriens, J. P., Acosta, R., Soutar, D. S. & Webster, M. H. Recovery of sensation in the radial forearm free flap in oral reconstruction. Plast. Reconstr. Surg. 98, 649–656 (1996).
Waits, C. A., Toby, E. B., Girod, D. A. & Tsue, T. T. Osteocutaneous radial forearm free flap: long-term radiographic evaluation of donor site morbidity after prophylactic plating of radius. J. Reconstr. Microsurg. 23, 367–372 (2007).
Ma, S., Cheng, K., Liu, Y. & Chen, F. A new surgical procedure for penile reconstruction by combined free radial forearm flap and dorsalis pedis flap. Urology 97, 232–237 (2016).
Hoebeke, P., de Cuypere, G., Ceulemans, P. & Monstrey, S. Obtaining rigidity in total phalloplasty: experience with 35 patients. J. Urol. 169, 221–223 (2003).
Selvaggi, G. et al. Scrotal reconstruction in female-to-male transsexuals: a novel scrotoplasty. Plast. Reconstr. Surg. 123, 1710–1718 (2009). Presentation of the novel technique for transman scrotoplasty.
Hage, J. J., Bouman, F. G. & Bloem, J. J. Constructing a scrotum in female-to-male transsexuals. Plast. Reconstr. Surg. 91, 914–921 (1993).
Millard, D. R. Jr. Scrotal construction and reconstruction. Plast. Reconstr. Surg. 38, 10–15 (1966).
Reid, C. F. & Wright, J. H. Jr. Scrotal reconstruction following an avulsion injury. J. Urol. 133, 681–682 (1985).
Sengezer, M. & Sadove, R. C. Scrotal construction by expansion of labia majora in biological female transsexuals. Ann. Plast. Surg. 31, 372–376 (1993).
Still, E. F. II & Goodman, R. C. Total reconstruction of a two-compartment scrotum by tissue expansion. Plast. Reconstr. Surg. 85, 805–807 (1990).
Lumen, N., Monstrey, S., Goessaert, A. S., Oosterlinck, W. & Hoebeke, P. Urethroplasty for strictures after phallic reconstruction: a single-institution experience. Eur. Urol. 60, 150–158 (2011). Analysis of outcomes and techniques for urethral fistula and stricture repair in phalloplasty.
Wilson, S. C. et al. Fasciocutaneous flap reinforcement of ventral onlay buccal mucosa grafts enables neophallus revision urethroplasty. Ther. Adv. Urol. 8, 331–337 (2016).
Dabernig, J., Shelley, O. P., Cuccia, G. & Schaff, J. Urethral reconstruction using the radial forearm free flap: experience in oncologic cases and gender reassignment. Eur. Urol. 52, 547–553 (2007).
Garaffa, G., Ralph, D. J. & Christopher, N. Total urethral construction with the radial artery-based forearm free flap in the transsexual. BJU Int. 106, 1206–1210 (2010).
Kim, S. K., Moon, J. B., Heo, J., Kwon, Y. S. & Lee, K. C. A new method of urethroplasty for prevention of fistula in female-to-male gender reassignment surgery. Ann. Plast. Surg. 64, 759–764 (2010).
Bayramicli, M. & Akdeniz, Z. D. Urethra reconstruction with lateral pectoral flap in female-to-male transsexual patients. J. Plast. Reconstr. Aesthet. Surg. 69, 1558–1560 (2016).
De Filippo, R. E., Yoo, J. J. & Atala, A. Urethral replacement using cell seeded tubularized collagen matrices. J. Urol. 168, 1789–1792 (2002).
Chen, K. L., Eberli, D., Yoo, J. J. & Atala, A. Bioengineered corporal tissue for structural and functional restoration of the penis. Proc. Natl Acad. Sci. USA 107, 3346–3350 (2010).
Joo, K. J. et al. Porcine vesical acellular matrix graft of tunica albuginea for penile reconstruction. Asian J. Androl. 8, 543–548 (2006).
Kwon, T. G., Yoo, J. J. & Atala, A. Autologous penile corpora cavernosa replacement using tissue engineering techniques. J. Urol. 168, 1754–1758 (2002).
Kropp, B. P. et al. Use of small intestinal submucosa for corporal body grafting in cases of severe penile curvature. J. Urol. 168, 1742–1745 (2002).
Raya-Rivera, A. M. et al. Tissue-engineered autologous vaginal organs in patients: a pilot cohort study. Lancet 384, 329–336 (2014).
Sopko, N. A. et al. Ex vivo model of human penile transplantation and rejection: implications for erectile tissue physiology. Eur. Urol. 71, 584–593 (2017).
Tuffaha, S. H. et al. Using the dorsal, cavernosal, and external pudendal arteries for penile transplantation: technical considerations and perfusion territories. Plast. Reconstr. Surg. 134, 111e–119e (2014).
Selvaggi, G., Branemark, R., Elander, A., Liden, M. & Stalfors, J. Titanium-bone-anchored penile epithesis: preoperative planning and immediate postoperative results. J. Plast. Surg. Hand. Surg. 49, 40–44 (2015).
Selvaggi, G., Elander, A. & Branemark, R. Penile epithesis: preliminary study. Plast. Reconstr. Surg. 126, 265e–266e (2010).
Massie, J. P., Morrison, S. D., Smith, J. R., Wilson, S. C. & Satterwhite, T. Letter to the editor regarding “Surgical outcome after penile inversion vaginoplasty: a retrospective study of 475 transgender women” by Buncamper et al. Plast. Reconstr. Surg. http://dx.doi.org/10.1097/PRS.0000000000003479 (2017).
Berli, J. U. et al. What surgeons need to know about gender confirmation surgery when providing care for transgender individuals: a review. JAMA Surg. 152, 394–400 (2017).
Author information
Authors and Affiliations
Contributions
S.D.M., C.N.C and M.C. researched data for article, made substantial contributions to discussions of content, and reviewed and edited the manuscript before submission. S.D.M. and M.C. wrote the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Gender dysphoria
-
Inherent discordance of a patient's gender expression and their anatomy leading to distress
- Nipple-areolar complex
-
Tissue forming the nipple and surrounding areola on the breast or chest
- Allen's test
-
A physical examination test to determine the patency of the palmar or plantar arches as a correlate for the dominant inflow vessel to the hand or foot. Most commonly it is used in the hand where the radial and ulnar arteries are both occluded with pressure from the examiners hand and each is released sequentially while maintaining the pressure on the other artery. The perfusion of the hand is monitored to ensure both vessels can perfuse the hand.
- Cismale
-
A person born as a male and whose gender identity is male.
- Johanson procedure
-
Urological procedure for urethral strictures, in which the ventral aspect of the phallus is opened through the urethra. The urethra is secured to the skin and urine is diverted. A second stage completed months later is used to repair the urethra with grafted tissue over a catheter.
- Chimeric flaps
-
Flaps containing multiple tissue types (skin, bone, mucosa.) based on a single angiosome used for complex reconstruction.
- V–Y advancement
-
Local flap used for advancing tissue generally to cover a wound, but can be used in other procedures. An incision shaped like a V is made through the subcutaneous tissue, advanced into its new position relying on subcutaneous perfusion, and closed in a Y pattern.
- Heineke–Mekulicz principle
-
Closure of a urethral stricture with a longitudinal incision followed by a transverse closure.
- Transman
-
A person born with female sexual organs, but whose gender identity is male
Rights and permissions
About this article
Cite this article
Morrison, S., Chen, M. & Crane, C. An overview of female-to-male gender-confirming surgery. Nat Rev Urol 14, 486–500 (2017). https://doi.org/10.1038/nrurol.2017.64
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2017.64
This article is cited by
-
Geschlechtsinkongruenz – Definition, Diagnosestellung und Transitionsoptionen
Urologie in der Praxis (2023)
-
(De-)centralized health care delivery, surgical outcome, and psychosocial health of transgender and gender-diverse people undergoing vaginoplasty: results of a retrospective, single-center study
World Journal of Urology (2023)
-
Gender Affirmation Surgery for the Transmasculine Patient
Current Obstetrics and Gynecology Reports (2022)
-
Urethral complications after gender reassignment surgery: a systematic review
International Journal of Impotence Research (2021)
-
Suprapubic phalloplasty in transmen: surgical results and critical review
International Journal of Impotence Research (2021)



