Key Points
-
Monogenic autoinflammatory diseases can be classified on the basis of their dominating clinical feature (for example, periodic fever) or their pathogenesis (for example, as IL-1 or NFκB activation disorders)
-
Among the monogenic autoinflammatory diseases, clinical diagnostic criteria have already been suggested for familial Mediterranean fever (FMF), and we suggest a flowchart to guide requests for mutation analysis of the associated gene
-
FMF is an autosomal recessive disease; however, a single mutation, or a clear disease-causing mutation together with a variant with low penetrance, can be associated with the clinical phenotype
-
Clinical classification criteria and flowcharts to guide physicians in decision-making and asking for specific genetic testing are also needed for other autoinflammatory diseases
-
Anti-IL-1 treatment has shown promising results in many of the autoinflammatory diseases
Abstract
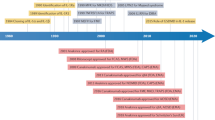
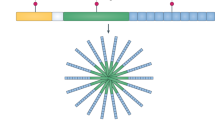
Autoinflammatory diseases are associated with abnormal activation of the innate immune system, leading to clinical inflammation and high levels of acute-phase reactants. The first group to be identified was the periodic fever diseases, of which familial Mediterranean fever (FMF) is the most common. In FMF, genetic results are not always straightforward; thus, flowcharts to guide the physician in requesting mutation analyses and interpreting the findings are presented in this Review. The other periodic fever diseases, which include cryopyrin-associated periodic syndromes (CAPS), TNF receptor-associated periodic syndrome (TRAPS) and mevalonate kinase deficiency/hyperimmunoglobulin D syndrome (MKD/HIDS), have distinguishing features that should be sought for carefully during diagnosis. Among this group of diseases, increasing evidence exists for the efficacy of anti-IL-1 treatment, suggesting a major role of IL-1 in their pathogenesis. In the past decade, we have started to learn about the other rare autoinflammatory diseases in which fever is less pronounced. Among them are diseases manifesting with pyogenic lesions of the skin and bone; diseases associated with granulomatous lesions; diseases associated with psoriasis; and diseases associated with defects in the immunoproteasome. A better understanding of the pathogenesis of these autoinflammatory diseases has enabled us to provide targeted biologic treatment at least for some of these conditions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Balow, J. E. Jr et al. A high-resolution genetic map of the familial Mediterranean fever candidate region allows identification of haplotype-sharing among ethnic groups. Genomics 44, 280–291 (1997).
French FMF Consortium. A candidate gene for familial Mediterranean fever. Nat. Genet. 17, 25–31 (1997).
Masters, S. L., Simon, A., Aksentijevich, I. & Kastner, D. L. Horror autoinflammaticus: the molecular pathophysiology of autoinflammatory disease. Annu. Rev. Immunol. 27, 621–668 (2009).
Park, H., Bourla, A. B., Kastner, D. L., Colbert, R. A. & Siegel, R. M. Lighting the fires within: the cell biology of autoinflammatory diseases. Nat. Rev. Immunol. 12, 570–580 (2012).
Toplak, N. et al. An international registry on autoinflammatory disease: the Eurofever experience. Ann. Rheum. Dis. 71, 1177–1182 (2012).
Ozen, S. Mutations/polymorphisms in a monogenetic autoinflammatory disease may be susceptibility markers for certain rheumatic diseases: lessons from the bedside for the benchside. Clin. Exp. Rheumatol. 27 (Suppl. 53), S29–S31 (2009).
Chae, J. J. et al. The B30.2 domain of pyrin, the familial Mediterranean fever protein interacts indirectly with caspase-1 to modulate IL-1β production. Proc. Natl Acad. Sci. USA. 103, 9982–9987 (2006).
Seshardi, S., Duncan, M. D., Hart, J. M., Gavrilin, M. A. & Wevers, M. D. Pyrin levels in human monocytes and monocyte derived macrophages regulate IL-1β processing and release. J. Immunol. 179, 1274–1281 (2007).
Papin, S. et al. The SPRY domain of Pyrin mutated in familial Mediterranean fever patients interacts with inflammasome components and inhibits pro IL-1β production. Cell Death Differ. 14, 1457–1466 (2007).
Chae, J. J. et al. Gain-of function Pyrin mutations induce NLRP3 protein independent interleukin-1β activation and severe autoinflammation in mice. Immunity 34, 755–768 (2011).
Tunca, M. et al. Familial Mediterranean fever in Turkey: results of a nationwide multicenter study. Medicine 84, 1–11 (2005).
Kogan, A. et al. Common MEFV mutations among Jewish ethnic groups in Israel: high frequency of carrier sand phenotype III states and absence of a perceptible biological advantage for the carrier state. Am. J. Med. Genet. 102, 272–276 (2001).
Ozen, S. et al. Mutations in the gene for FMF: do they predispose to inflammation? J. Rheumatol. 30, 2014–2018 (2003).
Ayaz, N. A. et al. MEFV mutations in systemic juvenile idiopathic arthritis. Rheumatology (Oxford) 48, 23–25 (2009).
Berkun, Y. et al. The familial Mediterranean fever gene as a modifier of periodic fever, aphtous stomatitis, pharyngitis and adenopathy syndrome. Semin. Arthritis Rheum. 40, 467–472 (2011).
Yilmaz, E. et al. Mutation frequency of familial Mediterranean fever and evidence of a high carrier rate in the Turkish population. Eur. J. Human Genet. 9, 553–555 (2001).
Daniels, M., Shohat, T., Brenner-Ullman, A. & Shohat, M. FMF: high gene frequency among the non-Ashkenazic and Ashkenazic Jewish populations in Israel. Am. J. Med. Genet. 55, 311–314 (1995).
Ozen, S. et al. Prevalence of juvenile chronic arthritis and FMF in Turkey: a field study. J. Rheumatol. 25, 2445–2449 (1998).
Gkretsi, V., Deltas, C., Yapijakis, C. & Lamnissou, K. Screening for familial Mediterranean fever M694V and V726A mutations in the Greek population. Genet. Test. Mol. Biomarkers 13, 291–293 (2009).
Ozen, S. et al. Results from a multicentre international registry of Familial Mediterranean Fever: impact of environment on the expression of a monogenic disease in children. Ann. Rheum. Dis. 10.1136/annrheumdis-2012-202708.
Migita, K. et al. Familial Mediterranean fever in Japan. Medicine 91, 337–343 (2012).
Xuelian, H. et al. E148Q polymorphism is associated with HSP in Chinese children. Pediatr. Nephrol. 25, 2077–2082 (2010).
Booth, D. R., Lachman, H. J., Gillmore, J. D., Booth, S. E. & Hawkins, P. N. Prevalance and significance of the familial Mediterranean gene mutation encoding pyrin Q148. Q. J. Med. 94, 527–531 (2001).
Samuels, J. & Ozen, S. FMF and the other autoinflammatory syndromes: evaluation of the patient with recurrent fever. Curr. Opin. Rheumatol. 18, 108–117 (2006).
Livneh, A. et al. Criteria for the diagnosis of familial Mediterranean fever. Arthritis Rheum. 40, 1879–1885 (1997).
Yalçinkaya, F. et al. A new set of criteria for the diagnosis of familial Mediterranean fever in childhood. Rheumatology (Oxford) 48, 395–398 (2009).
Kondi, A. et al. Validation of the new paediatric criteria for the diagnosis of familial Mediterranean fever: data from a mixed population of 100 children from the French reference center for autoinflammatory disorders. Rheumatology (Oxford) 49, 2200–2203 (2010).
Saatçi, U. et al. Familial Mediterranean fever in children: report of a large series and discussion of the risk and prognostic factors of amyloidosis. Eur. J. Pediatr. 156, 619–623 (1997).
Shinar, Y. et al. Guidelines for the genetic diagnosis of hereditary recurrent fevers. Ann. Rheum. Dis. 71, 1599–1605 (2012).
Ozen, S., Besbas, N., Bakkaloglu, A. & Yilmaz, E. Pyrin Q148 mutation and familial Mediterranean fever. Q. J. Med. 95, 332–333 (2002).
Topaloglu, R. et al. E148Q is a disease-causing MEFV mutation: a phenotypic evaluation in patients with familial Mediterranean fever. Ann. Rheum. Dis. 64, 750–752 (2005).
Gershoni-Baruch, R., Broza, Y. & Brik, R. Prevalence and significance of mutations in the familial Mediterranean fever gene in Henoch–Schönlein purpura. J. Pediatr. 143, 658–661 (2003).
Aksentijevich, I. & Kastner, D. L. Genetics of monogenic autoinflammatory diseases: past successes, future challenges. Nat. Rev. Rheumatol. 7, 469–478 (2011).
Ozen, S. Changing concepts in familial Mediterranean fever: is it possible to have an autosomal-recessive disease with only one mutation? Arthritis Rheum. 60, 1575–1577 (2009).
Marek-Yagel, D. et al. Clinical disease among patients heterozygous for familial Mediterranean fever. Arthritis Rheum. 60, 1862–1866 (2009).
Singh-Grewal, D., Chaitow, J., Aksentijevich, I. & Christodoulou, J. Coexistent MEFV and CIAS1 mutations manifesting as FMF plus deafness. Ann. Rheum. Dis. 66, 1541 (2007).
Zemer, D. et al. Colchicine in the prevention and treatment of the amyloidosis of familial Mediterranean fever. N. Engl. J. Med. 314, 1001–1005 (1986).
Kallinich, T. et al. Colchicine use in children and adolescents with familial Mediterranean fever: literature review and consensus treatment. Pediatrics 119, e474–e483 (2007).
Ozturk, M. A. et al. Therapeutic approach to familial Mediterranean fever: a review update. Clin. Exp. Rheumatol. 29 (Suppl. 67), S77–S86 (2011).
Ben-Zvi, I. & Livneh, A. Chronic inflammation in FMF; markers, risk factors, outcomes and therapy. Nat. Rev. Rheumatol. 7, 105–112 (2011).
Piram, M. et al. A preliminary score for the assessment of disease activity in hereditary recurrent fevers. Ann. Rheum. Dis. 70, 309–314 (2011).
Ozen, S., Bilginer, Y., Aktay Ayaz, N. & Calguneri, M. Anti-interleukin 1 treatment for patients with familial Meditarrenean fever resistant to colchicine. J. Rheumatol. 38, 516–518 (2011).
Kallinich, T., Wittkowski, H., Keitzer, R., Roth, J. & Foell, D. Neutrophil-derived S100A12 as novel biomarker of inflammation in familial Mediterranean fever. Ann. Rheum. Dis. 69, 677–682 (2010).
Ben-Chetrit, E. & Aamar, S. About colchicine compliance, resistance and virulence. Clin. Exp. Rheumatol. 27 (Suppl. 53), S1–S3 (2009).
Hashkes, P. J. et al. Rilonacept for colchicine-resistant or -intolerant familial Mediterranean fever: a randomized trial. Ann. Intern. Med. 157, 533–541 (2012).
Meinzer, U. et al. Interleukin-1 targeting drugs in familial Mediterranean fever: a case series and a review of the literature. Semin. Arthritis Rheum. 41, 265–271 (2011).
Hacihamdioglu, D. O. & Ozen, S. Canakinumab induces remission in a patient with resistant familial Mediterranean fever. Rheumatology (Oxford) 51, 1041 (2012).
Ozen, S., Frenkel, J., Ruperto, N. & Gattorno, M. The Eurofever Project: towards better care for autoinflammatory diseases. Eur. J. Pediatr. 170, 445–452 (2011).
Hoffman, H. M. et al. Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle–Wells syndrome. Nat. Genet. 29, 301–305 (2009).
Feldmann, J. et al. Chronic infantile neurological cutaneous and articular syndrome is caused by mutations in CIAS1, a gene highly expressed in polymorphonuclear cells and chondrocytes. Am. J. Hum. Genet. 71, 198–203 (2002).
Aksentijevich, I. et al. De novo CIAS1 mutations, cytokine activation, and evidence for genetic heterogeneity in patients with neonatal-onset multisystem inflammatory disease (NOMID): a new member of the expanding family of pyrin- associated autoinflammatory diseases. Arthritis Rheum. 46, 3340–3348 (2002).
Saito, M. et al. Disease-associated CIAS1 mutations induce monocyte death, revealing low level mosaicism in mutation-negative cryopyrin- associated periodic syndrome patients. Blood 111, 2132–2141 (2007).
Stych, B. & Dobrovolny, D. Familial cold autoinflammatory syndrome (FCAS): characterization of symptomatology and impact on patients' lives. Curr. Med. Res. Opin. 24, 1577–1582 (2008).
Glaser, R. L. & Goldbach-Mansky, R. The spectrum of monogenic autoinflammatory syndromes: understanding disease mechanisms and use of targeted therapies. Curr. Allergy Asthma Rep. 8, 288–298 (2008).
Deshner, J. B. et al. Two year results from an open-label, multicentre, phase III study evaluating the safety and efficacy of canakinumab in patients with cryopyrin associated periodic syndrome across different severity phenotypes. Ann. Rheum. Dis. 70, 2095–2102 (2011).
Ter Haar, N. et al. Treatment of autoinflammatory diseases: results from the Eurofever Registry and a literature review. Ann. Rheum. Dis. 72, 678–685 (2013).
Williamson, L. M. et al. Familial Hibernian fever. Q. J. Med. 51, 469–480 (1982).
McDermott, M. F. et al. Germline mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes. Cell 97, 133–144 (1999).
Touitou, I. et al. Infevers. An evolving mutation database for autoinflammatory syndromes. Hum. Mutat. 24, 194–198 (2004).
International Society of Systemic Auto-inflammatory Diseases. Infevers: The Registry of Hereditary Auto-inflammatory Disorders Mutations. Infevers [online].
Ravet, N. et al. Clinical significance of P46L and R92Q substitutions in the tumor necrosis superfamily 1A gene. Ann. Rheum. Dis. 65, 1158–1162 (2006).
Stojanov, S. et al. Clinical and functional characterization of a novel TNFRSF1A c.605T>A/V173D cleavage site mutation associated with tumour necrosis factor receptor associated periodic fever syndrome (TRAPS), cardiovascular complications and excellent response to etanercept treatment. Ann. Rheum. Dis. 67, 1292–1298 (2008).
Bulua, A. C. et al. Mitochondrial reactive oxygen species promote production of proinflammatory cytokines and are elevated in TNFR1-associated periodic syndrome (TRAPS). J. Exp. Med. 208, 519–533 (2011).
Bachetti, T. et al. Autophagy contributes to inflammation in patients with TNFR-associated periodic syndrome (TRAPS). Ann. Rheum. Dis. 72, 1044–1052 (2013).
Dickie, L. J. et al. Involvement of X-box binding protein 1 and reactive oxygen species pathways in the pathogenesis of tumor necrosis factor receptor associated periodic syndrome. Ann. Rheum. Dis. 71, 2035–2043 (2012).
Cantarini, L. et al. Tumor necrosis factor receptor-associated periodic syndrome (TRAPS): State of the art and future perspectives. Autoimmunity Rev. 12, 38–43 (2012).
Petterson, T., Kantonen, J., Matikainen, S. & Repo, H. Setting up TRAPS. Ann. Med. 4, 109–118 (2012).
Hull, K. M. et al. The TNF-receptor associated periodic syndrome (TRAPS): emerging concepts of an autoinflammatory disorder. Medicine 81, 349–368 (2002).
Drewe, E., Powell, R. J. & McDermott, E. M. Comment on: failure of anti-TNF therapy in TNF receptor 1-associated periodic syndrome (TRAPS). Rheumatology 46, 1865–1866 (2007).
Bulua, A. C. et al. Efficacy of etanercept in the tumor necrosis factor receptor associated periodic syndrome: a prospective, open-label, dose escalation study. Arthritis Rheum. 64, 908–913 (2012).
Jesus, A. A. et al. TNF-receptor associated periodic syndrome (TRAPS): description of a novel TNFRSF1A mutation and response to etanercept. Eur. J. Pediatr. 167, 1421–1425 (2008).
Gattorno, M. et al. Persistent efficacy of anakinra in patients with tumor necrosis factor receptor associated periodic syndrome. Arthritis Rheum. 58, 1516–1520 (2008).
Lachmann, H. J. et al. Canakinumab in patients with TRAPS. Abstract 1103, ISSAID 2013.
van der Meer, J. W. et al. Hyperimmunoglobulinemia D and periodic fever: a new syndrome. Lancet 1, 1087–1090 (1984).
Drenth, J. P. et al. Mutations in the gene encoding mevalonate kinase cause hyper-IgD and periodic fever syndrome. Nat. Genet. 22, 178–181 (1999).
van der Burgh, R., Ter Haar, N. M., Boes, M. L. & Frenkel, J. Mevolanate kinase deficiency, a metabolic autoinflammatory disease. Clin. Immunol. 147, 197–206 (2013).
Mandey, S. H., Kuijk, L. M., Frenkel, J. & Waterham, H. R. A role for geranylgeranylation in interleukin 1β secretion. Arthritis Rheum. 54, 3690–3695 (2006).
Federici, S., Caorsi, R. & Gattorno, M. The autoinflammatory diseases. Swiss Med. Wkly 142, w13602 (2012).
Frenkel, J. et al. Clinical and molecular variability in childhood periodic fever with hyperimmunoglobulinemia D. Rheumatology (Oxford) 40, 579–584 (2001).
Bader-Meunier, B. et al. Mevolanate kinase deficiency: a survey of 50 patients. Pediatrics 128, e152–e159 (2011).
Lachmann, H. J. et al. AA amyloidosis complicating hyperimmunoglobulinemia D with periodic fever syndrome: a report of two cases. Arthritis Rheum. 54, 2010–2014 (2006).
Stoffels, M. & Simon, A. Hyper-IgD syndrome or mevalonate kinase deficiency. Curr. Opin. Rheumatol. 23, 419–423 (2011).
Ammouri, M. et al. Diagnostic value of serum immunoglobulinemia D level in patients with a clinical suspicion of hyper IgD syndrome. Rheumatology (Oxford) 46, 1597–1600 (2007).
Takada, K. et al. Favorable preliminary experience with etanercept in two patients with the hyperimmunoglobulinemia D and periodic fever syndrome. Arthritis Rheum. 48, 2645–2651 (2003).
Rigante, D. et al. Treatment with anakinra in the hyperimmunoglobulinemia D/periodic fever syndrome. Rheumatol. Int. 27, 97–100 (2006).
Jeru, I. et al. Mutations in NALP12 cause hereditary periodic fever syndromes. Proc. Natl Acad. Sci. USA 105, 1614–1619 (2008).
Touitou, I. & Kone-Paut, I. Autoinflammatory diseases. Best Pract. Res. Clin. Rheumatol. 22, 811–829 (2008).
Aksentijevich, I. et al. An autoinflammatory disease with deficiency of the interleukin-1-receptor antagonist. N. Engl. J. Med. 360, 2426–2437 (2009).
Shoham, N. G. et al. Pyrin binds the PSTPIP1/CD2BP1 protein, defining familial Mediterranean fever and PAPA syndrome as disorders in the same pathway. Proc. Natl Acad. Sci. USA 100, 13501–13506 (2003).
Demidowich, A. P. et al. Brief report; genotype, phenotype, and clinical course in five patients with PAPA syndrome (pyogenic sterile arthritis, pyoderma gangrenosum and acne). Arthritis Rheum. 64, 2022–2027 (2012).
Ferguson, P. J. et al. Homozygous mutations in LPIN2 are responsible for the syndrome of chronic recurrent multifocal osteomyelitis and congenital dyserythropoietic anaemia (Majeed syndrome). J. Med. Genet. 42, 551–557 (2005).
Herlin, T. et al. Efficacy of IL-1 treatment in Majeed syndrome. Ann. Rheum. Dis. 72, 410–413 (2013).
Sfriso, P. et al. Blau syndrome, clinical and genetic aspects. Autoimmun. Rev. 12, 44–51 (2012).
Rose, C. D. et al. Pediatric granulomatous arthritis: an international registry. Arthritis Rheum. 54, 3337–3344 (2006).
Arostegui, J. I. et al. NOD2 gene-associated pediatric granulamatous arthritis: clinical diversity, novel and recurrent mutations, and evidence of clinical improvement with interleukin-1 blockade in a Spanish cohort. Arthritis Rheum. 56, 3805–3813 (2007).
Milman, M. et al. Favourable effect of TNFα inhibitor on Blau syndrome in monozygotic twins with a de novo CARD15 mutation. APMIS 114, 912–919 (2006).
Marrakchi, S. et al. Interleukin-36-receptor antagonist deficiency and generalized pustular psoriasis. N. Engl. J. Med. 365, 620–628 (2011).
Seifert, U. et al. Immunoproteasomes preserve protein homeostasis upon interferon-induced oxidative stress. Cell 142, 613–624 (2010).
Arima, K. et al. Proteasome assembly defect due to a proteasome subunit beta type 8 (PSMB8) mutation causes the autoinflammatory disorder, Nakajo–Nishimura syndrome. Proc. Natl Acad. Sci. USA 108, 14914–14919 (2011).
Garg, A. et al. An autosomal recessive syndrome of joint contractures, muscular atrophy, microcytic anemia, and panniculitis-associated lipodystrophy. J. Clin. Endocrinol. Metab. 95, E58–E63 (2010).
Liu, Y. et al. Mutations in proteosome subunit β type 8 cause chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature with evidence of genetic and phenotypic heterogeneity. Arthritis Rheum. 64, 895–907 (2012).
Vantyghem, M. C. et al. How to diagnose a lipodystrophy syndrome. Ann. Endocrinol. (Paris) 73, 170–189 (2012).
Ombrella, M. J. et al. Cold urticaria, immunodeficiency, and autoimmunity related to PLCG2 deficiency. N. Engl. J. Med. 366, 330–338 (2012).
Caorsi, R. et al. Periodic fever, apthous stomatitis, pharyngitis and adenitis syndrome. Curr. Opin. Rheumatol. 22, 579–584 (2010).
Acknowledgements
We thank I. Aksentijevich for her comments.
Author information
Authors and Affiliations
Contributions
Both authors contributed to writing the article. In addition, S. Ozen decided on the content of the article and reviewed the manuscript before submission, and Y. Bilginer researched data for the article.
Corresponding author
Ethics declarations
Competing interests
S. Ozen declares that she has received a consultancy fee from Novartis and speaker honouraria from Biovitrium. Y. Bilginer declares no competing interests.
Rights and permissions
About this article
Cite this article
Ozen, S., Bilginer, Y. A clinical guide to autoinflammatory diseases: familial Mediterranean fever and next-of-kin. Nat Rev Rheumatol 10, 135–147 (2014). https://doi.org/10.1038/nrrheum.2013.174
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrrheum.2013.174
This article is cited by
-
Recent Insights in Pyrin Inflammasome Activation: Identifying Potential Novel Therapeutic Approaches in Pyrin-Associated Autoinflammatory Syndromes
Journal of Clinical Immunology (2024)
-
Effect of interleukin-1 antagonist on growth of children with colchicine resistant or intolerant FMF
Pediatric Rheumatology (2023)
-
Early systemic inflammation induces neurodevelopmental disorders: results from ARTEMIS, a French multicenter study of juvenile rheumatisms and systemic autoimmune and auto-inflammatory disorders and meta-analysis
Molecular Psychiatry (2023)
-
The efficacy of a single-dose anakinra injection during disease attack in pediatric familial Mediterranean fever
Rheumatology International (2023)
-
Evaluation of bone changes on dental panoramic radiography using mandibular indexes and fractal dimension analysis in children with familial Mediterranean fever
Oral Radiology (2023)