Key Points
-
Multiple sclerosis is thought to be mediated by autoimmune T cell responses directed against antigens derived from the central nervous system (CNS). The clinical course, symptoms and pathology seen in patients with multiple sclerosis is heterogeneous, suggesting that multiple sclerosis in different patients may result from distinct pathogenic pathways.
-
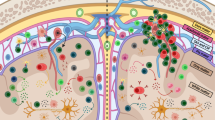
Autoimmune disease in the CNS occurs when self-reactive T cells specific for CNS antigens are activated in the periphery, either by presentation of the self antigen in the CNS-draining (cervical) lymph nodes or by a molecular mimic of the self antigen. Unlike naive T cells, activated T cells can cross the blood–cerebrospinal fluid (CSF) or blood–brain barrier. Activated T cells are believed to initially cross the blood–CSF barrier and enter the subarachnoid space, where their reactivation facilitates activation of the vascular endothelium and subsequent T cell entry into the perivascular space.
-
The myelin-specific CD4+ T cells that mediate CNS autoimmunity in animal models are usually T cells that circulate in the periphery because they escaped central tolerance owing to low avidity for their cognate antigen.
-
Both CD4+ T helper 1 (TH1) cells, characterized by interferon-γ (IFNγ) secretion, and TH17 cells, characterized by interleukin-17 (IL-17) secretion, can induce CNS autoimmune disease. The interplay between these T cell subsets as well as their interaction with other cells that reside within the CNS is poorly understood but is likely to have an important role in shaping the inflammatory response in different locations within the CNS.
-
During inflammation there are many cell types that can present antigen to CD4+ T cells; the relative contribution and activation state of these different antigen-presenting cells strongly influences the effector function and survival of T cells in the CNS.
-
CD8+ T cells exhibit more evidence of antigen-driven expansion in the CNS of patients with multiple sclerosis, and myelin-specific CD8+ T cells are highly pathogenic in experimental autoimmune encephalomyelitis. However, in addition to CD4+ regulatory T cells, several different types of regulatory CD8+ T cells have been described that may be important in the pathology of multiple sclerosis.
-
Despite the fact that T cells are believed to be the primary effector cells in the pathology of multiple sclerosis, depletion of B cells is a promising therapeutic treatment for patients with multiple sclerosis. It is not yet clear whether the beneficial effect of this therapy is due to disruption of the antigen-presenting function of B cells or their ability to produce antibodies.
Abstract
Autoreactive T cell responses have a crucial role in central nervous system (CNS) diseases such as multiple sclerosis. Recent data indicate that CNS autoimmunity can be mediated by two distinct lineages of CD4+ T cells that are defined by the production of either interferon-γ or interleukin-17. The activity of these CD4+ T cell subsets within the CNS influences the pathology and clinical course of disease. New animal models show that myelin-specific CD8+ T cells can also mediate CNS autoimmunity. This Review focuses on recent progress in delineating the pathogenic mechanisms, regulation and interplay between these different T cell subsets in CNS autoimmunity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
McFarland, H. F. & Martin, R. Multiple sclerosis: a complicated picture of autoimmunity. Nature Immunol. 8, 913–919 (2007).
Lucchinetti, C. et al. Heterogeneity of multiple sclerosis lesions: implications for the pathogenesis of demyelination. Ann. Neurol. 47, 707–717 (2000).
Raine, C. in Multiple Sclerosis: Clinical and Pathogenetic Basis (eds Raine, C. S., McFarland, H. F. & Tourtellotte, W. W.) 243–286 (Chapman and Hall, London, 1997).
Ransohoff, R. M., Kivisakk, P. & Kidd, G. Three or more routes for leukocyte migration into the central nervous system. Nature Rev. Immunol. 3, 569–581 (2003).
Huseby, E. S., Sather, B., Huseby, P. G. & Goverman, J. Age-dependent T cell tolerance and autoimmunity to myelin basic protein. Immunity 14, 471–481 (2001).
Perchellet, A., Stromnes, I., Pang, J. M. & Goverman, J. CD8+ T cells maintain tolerance to myelin basic protein by 'epitope theft'. Nature Immunol. 5, 606–614 (2004). This paper identifies a new form of tolerance that allows CD8+ T cells specific for MBP to circulate in the periphery without responding to endogenous MBP.
Pender, M. P., Tabi, Z., Nguyen, K. B. & McCombe, P. A. The proximal peripheral nervous system is a major site of demyelination in experimental autoimmune encephalomyelitis induced in the Lewis rat by a myelin basic protein-specific T cell clone. Acta Neuropathol. 89, 527–531 (1995).
Furtado, G. C. et al. Swift entry of myelin-specific T lymphocytes into the central nervous system in spontaneous autoimmune encephalomyelitis. J. Immunol. 181, 4648–4655 (2008).
Zhang, H., Podojil, J. R., Luo, X. & Miller, S. D. Intrinsic and induced regulation of the age-associated onset of spontaneous experimental autoimmune encephalomyelitis. J. Immunol. 181, 4638–4647 (2008).
Piccio, L. et al. Molecular mechanisms involved in lymphocyte recruitment in inflamed brain microvessels: critical roles for P-selectin glycoprotein ligand-1 and heterotrimeric Gi-linked receptors. J. Immunol. 168, 1940–1949 (2002).
Reboldi, A. et al. C-C chemokine receptor 6-regulated entry of TH-17 cells into the CNS through the choroid plexus is required for the initiation of EAE. Nature Immunol. 10, 514–523 (2009).
Lassmann, H. & Wisniewski, H. M. Chronic relapsing EAE. Time course of neurological symptoms and pathology. Acta Neuropathol. 43, 35–42 (1978).
Kivisakk, P. et al. Localizing central nervous system immune surveillance: Meningeal antigen-presenting cells activate T cells during experimental autoimmune encephalomyelitis. Ann. Neurol. 21 May 2008 (doi:10.1002/ana.21379).
Brown, D. A. & Sawchenko, P. E. Time course and distribution of inflammatory and neurodegenerative events suggest structural bases for the pathogenesis of experimental autoimmune encephalomyelitis. J. Comp. Neurol. 502, 236–260 (2007). This paper describes the temporal and spatial pattern of inflammatory and degenerative events that occur during the induction of EAE.
Gimenez, M. A., Sim, J., Archambault, A. S., Klein, R. S. & Russell, J. H. A tumor necrosis factor receptor 1-dependent conversation between central nervous system-specific T cells and the central nervous system is required for inflammatory infiltration of the spinal cord. Am. J. Pathol. 168, 1200–1209 (2006).
Kawakami, N. et al. The activation status of neuroantigen-specific T cells in the target organ determines the clinical outcome of autoimmune encephalomyelitis. J. Exp. Med. 199, 185–197 (2004).
Freeman, G. J. et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J. Exp. Med. 192, 1027–1034 (2000).
Kim, J. V., Kang, S. S., Dustin, M. L. & McGavern, D. B. Myelomonocytic cell recruitment causes fatal CNS vascular injury during acute viral meningitis. Nature 457, 191–197 (2009).
Carson, M. J., Reilly, C. R., Sutcliffe, J. G. & Lo, D. Disproportionate recruitment of CD8+ T cells into the central nervous system by professional antigen-presenting cells. Am. J. Pathol. 154, 481–494 (1999).
Brabb, T. et al. In situ tolerance within the central nervous system as a mechanism for preventing autoimmunity. J. Exp. Med. 192, 871–880 (2000).
Battistini, L. et al. CD8+ T cells from patients with acute multiple sclerosis display selective increase of adhesiveness in brain venules: a critical role for P-selectin glycoprotein ligand-1. Blood 101, 4775–4782 (2003).
Eikelenboom, M. J. et al. Chemokine receptor expression on T cells is related to new lesion development in multiple sclerosis. J. Neuroimmunol. 133, 225–232 (2002).
Hafler, D. A. et al. Risk alleles for multiple sclerosis identified by a genomewide study. N. Engl. J. Med. 357, 851–862 (2007).
Harrington, C. J. et al. Differential tolerance is induced in T cells recognizing distinct epitopes of myelin basic protein. Immunity 8, 571–580 (1998). This paper shows that the dependence of central tolerance on T cell functional avidity for antigen allows some, but not all, MBP-specific immune tolerance to escape immune tolerance.
Anderson, A. C. et al. High frequency of autoreactive myelin proteolipid protein-specific T cells in the periphery of naive mice: mechanisms of selection of the self-reactive repertoire. J. Exp. Med. 191, 761–770 (2000).
Klein, L., Klugmann, M., Nave, K. A., Tuohy, V. K. & Kyewski, B. Shaping of the autoreactive T-cell repertoire by a splice variant of self protein expressed in thymic epithelial cells. Nature Med. 6, 56–61 (2000).
Seamons, A., Perchellet, A. & Goverman, J. Immune tolerance to myelin proteins. Immunol. Res. 28, 201–221 (2003).
Cabbage, S. E. et al. Regulatory T cells maintain long-term tolerance to myelin basic protein by inducing a novel, dynamic state of T cell tolerance. J. Immunol. 178, 887–896 (2007).
Bielekova, B. et al. Expansion and functional relevance of high-avidity myelin-specific CD4+ T cells in multiple sclerosis. J. Immunol. 172, 3893–3904 (2004).
Burns, J., Bartholomew, B. & Lobo, S. Isolation of myelin basic protein-specific T cells predominantly from the memory T-cell compartment in multiple sclerosis. Ann. Neurol. 45, 33–39 (1999).
Scholz, C., Patton, K. T., Anderson, D. E., Freeman, G. J. & Hafler, D. A. Expansion of autoreactive T cells in multiple sclerosis is independent of exogenous B7 costimulation. J. Immunol. 160, 1532–1538 (1998).
Lovett-Racke, A. E. et al. Decreased dependence of myelin basic protein-reactive T cells on CD28-mediated costimulation in multiple sclerosis patients. A marker of activated/memory T cells. J. Clin. Invest. 101, 725–730 (1998).
Ponsford, M. et al. Differential responses of CD45+ve T-cell subsets to MBP in multiple sclerosis. Clin. Exp. Immunol. 124, 315–322 (2001).
Zhang, X. et al. Degenerate TCR recognition and dual DR2 restriction of autoreactive T cells: implications for the initiation of the autoimmune response in multiple sclerosis. Eur. J. Immunol. 38, 1297–1309 (2008).
Fujinami, R. S. & Oldstone, M. B. Amino acid homology between the encephalitogenic site of myelin basic protein and virus: mechanism for autoimmunity. Science 230, 1043–1045 (1985).
Münz, C., Lünemann, J. D., Getts, M. T. & Miller, S. D. Antiviral immune responses: triggers of or triggered by autoimmunity? Nature Rev. Immunol. 9, 246–258 (2009).
Wucherpfennig, K. W. & Strominger, J. L. Molecular mimicry in T cell-mediated autoimmunity: viral peptides activate human T cell clones specific for myelin basic protein. Cell 80, 695–705 (1995). This paper shows that a search using a molecular mimicry motif based on structural rather than sequence similarity identifies distinct, multiple peptides from microorganisms that can activate human T cells specific for MBP.
Lang, H. L. et al. A functional and structural basis for TCR cross-reactivity in multiple sclerosis. Nature Immunol. 3, 940–943 (2002).
Tejada-Simon, M. V., Zang, Y. C., Hong, J., Rivera, V. M. & Zhang, J. Z. Cross-reactivity with myelin basic protein and human herpesvirus-6 in multiple sclerosis. Ann. Neurol. 53, 189–197 (2003).
Holmoy, T., Kvale, E. O. & Vartdal, F. Cerebrospinal fluid CD4+ T cells from a multiple sclerosis patient cross-recognize Epstein–Barr virus and myelin basic protein. J. Neurovirol. 10, 278–283 (2004).
Markovic-Plese, S. et al. High level of cross-reactivity in influenza virus hemagglutinin-specific CD4+ T-cell response: implications for the initiation of autoimmune response in multiple sclerosis. J. Neuroimmunol. 169, 31–38 (2005).
Goverman, J. et al. Transgenic mice that express a myelin basic protein-specific T cell receptor develop spontaneous autoimmunity. Cell 72, 551–560 (1993). This paper is the first to show that T cells specific for some epitopes of MBP are not subject to deletion by central tolerance in vivo and that the incidence of spontaneous autoimmunity mediated by these T cells is influenced by environmental factors.
Goverman, J. Tolerance and autoimmunity in TCR transgenic mice specific for myelin basic protein. Immunol. Rev. 169, 147–159 (1999).
Krishnamoorthy, G. Cumulative autoimmunity: Myelin oligodendrocyte glycoprotein-specific T cells co-recognize neurofilament-M in a spontaneous experimental autoimmune encephalomyelitis of the C57BL/6 mouse. Nature Med. (in the press).
Gutcher, I. & Becher, B. APC-derived cytokines and T cell polarization in autoimmune inflammation. J. Clin. Invest. 117, 1119–1127 (2007).
Panitch, H. S., Hirsch, R. L., Haley, A. S. & Johnson, K. P. Exacerbations of multiple sclerosis in patients treated with gamma interferon. Lancet 1, 893–895 (1987).
Baron, J. L., Madri, J. A., Ruddle, N. H., Hashim, G. & Janeway, C. A. Jr. Surface expression of alpha 4 integrin by CD4 T cells is required for their entry into brain parenchyma. J. Exp. Med. 177, 57–68 (1993).
Segal, B. M. & Shevach, E. M. IL-12 unmasks latent autoimmune disease in resistant mice. J. Exp. Med. 184, 771–775 (1996).
Steinman, L. A brief history of TH17, the first major revision in the T H 1/T H 2 hypothesis of T cell-mediated tissue damage. Nature Med. 13, 139–145 (2007).
Cua, D. J. et al. Interleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature 421, 744–748 (2003).
McGeachy, M. J. et al. The interleukin 23 receptor is essential for the terminal differentiation of interleukin 17-producing effector T helper cells in vivo. Nature Immunol. 10, 314–324 (2009).
Korn, T., Bettelli, E., Oukka, M. & Kuchroo, V. K. IL-17 and Th17 Cells. Annu. Rev. Immunol. 27, 485–517 (2009).
Lock, C. et al. Gene-microarray analysis of multiple sclerosis lesions yields new targets validated in autoimmune encephalomyelitis. Nature Med. 8, 500–508 (2002).
Langrish, C. L. et al. IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J. Exp. Med. 201, 233–240 (2005). This paper is the first to show that myelin-specific T H 17 cells are more pathogenic following adoptive transfer into naive mice than T H 1 cells.
Park, H. et al. A distinct lineage of CD4 T cells regulates tissue inflammation by producing interleukin 17. Nature Immunol. 6, 1133–1141 (2005).
Hofstetter, H. H. et al. Therapeutic efficacy of IL-17 neutralization in murine experimental autoimmune encephalomyelitis. Cell. Immunol. 237, 123–130 (2005).
Komiyama, Y. et al. IL-17 plays an important role in the development of experimental autoimmune encephalomyelitis. J. Immunol. 177, 566–573 (2006).
Axtell, R. C., Xu, L., Barnum, S. R. & Raman, C. CD5–CK2 binding/activation-deficient mice are resistant to experimental autoimmune encephalomyelitis: protection is associated with diminished populations of IL-17-expressing T cells in the central nervous system. J. Immunol. 177, 8542–8549 (2006).
Ivanov, II. et al. The orphan nuclear receptor RORγt directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell 126, 1121–1133 (2006).
Haak, S. et al. IL-17A and IL-17F do not contribute vitally to autoimmune neuro-inflammation in mice. J. Clin. Invest. 119, 61–69 (2009). This paper questions the role of IL-17A and IL-17F by showing that the lack of these cytokines in vivo does not significantly affect the manifestation of EAE mediated by MOG 35–55 -specific T cells in C57BL/6 mice.
Rohn, T. A. et al. Vaccination against IL-17 suppresses autoimmune arthritis and encephalomyelitis. Eur. J. Immunol. 36, 2857–2867 (2006).
Luger, D. et al. Either a Th17 or a Th1 effector response can drive autoimmunity: conditions of disease induction affect dominant effector category. J. Exp. Med. 205, 799–810 (2008).
Stromnes, I. M., Cerretti, L. M., Liggitt, D., Harris, R. A. & Goverman, J. M. Differential regulation of central nervous system autoimmunity by TH1 and TH17 cells. Nature Med. 14, 337–342 (2008). This paper shows that inflammation is regulated differently in the brain compared with the spinal cord and provides evidence that the relative abundance of T H 17 and T H 1 cells in the infiltrating T cell population is a crucial factor in determining where inflammation localizes within the CNS.
Kroenke, M. A., Carlson, T. J., Andjelkovic, A. V. & Segal, B. M. IL-12- and IL-23-modulated T cells induce distinct types of EAE based on histology, CNS chemokine profile, and response to cytokine inhibition. J. Exp. Med. 205, 1535–1541 (2008).
O'Connor, R. A. et al. Cutting edge: Th1 cells facilitate the entry of Th17 cells to the central nervous system during experimental autoimmune encephalomyelitis. J. Immunol. 181, 3750–3754 (2008).
Storch, M. K. et al. Autoimmunity to myelin oligodendrocyte glycoprotein in rats mimics the spectrum of multiple sclerosis pathology. Brain Pathol. 8, 681–694 (1998).
Muller, D. M., Pender, M. P. & Greer, J. M. A neuropathological analysis of experimental autoimmune encephalomyelitis with predominant brain stem and cerebellar involvement and differences between active and passive induction. Acta Neuropathol. (Berl.) 100, 174–182 (2000).
Wensky, A. K. et al. IFN-γ determines distinct clinical outcomes in autoimmune encephalomyelitis. J. Immunol. 174, 1416–1423 (2005).
Lees, J. R., Golumbek, P. T., Sim, J., Dorsey, D. & Russell, J. H. Regional CNS responses to IFN-γ determine lesion localization patterns during EAE pathogenesis. J. Exp. Med. 205, 2633–2642 (2008). This paper shows that IFNγ signalling in CNS resident cells is required for inflammation in the spinal cord but inhibits inflammation in the brain.
Tran, E. H., Hoekstra, K., van Rooijen, N., Dijkstra, C. D. & Owens, T. Immune invasion of the central nervous system parenchyma and experimental allergic encephalomyelitis, but not leukocyte extravasation from blood, are prevented in macrophage-depleted mice. J. Immunol. 161, 3767–3775 (1998).
Greter, M. et al. Dendritic cells permit immune invasion of the CNS in an animal model of multiple sclerosis. Nature Med. 11, 328–334 (2005). This paper shows that DCs, which were previously considered to be scarce or absent from the non-inflamed CNS, are present in the CNS and are sufficient to reactivate primed T cells in the CNS and induce EAE.
Bailey, S. L., Schreiner, B., McMahon, E. J. & Miller, S. D. CNS myeloid DCs presenting endogenous myelin peptides 'preferentially' polarize CD4+ T H-17 cells in relapsing EAE. Nature Immunol. 8, 172–180 (2007).
Deshpande, P., King, I. L. & Segal, B. M. Cutting edge: CNS CD11c+ cells from mice with encephalomyelitis polarize Th17 cells and support CD25+CD4+ T cell-mediated immunosuppression, suggesting dual roles in the disease process. J. Immunol. 178, 6695–6699 (2007).
Bailey-Bucktrout, S. L. et al. Cutting edge: central nervous system plasmacytoid dendritic cells regulate the severity of relapsing experimental autoimmune encephalomyelitis. J. Immunol. 180, 6457–6461 (2008).
Aloisi, F. Immune function of microglia. Glia 36, 165–179 (2001).
Becher, B., Blain, M. & Antel, J. P. CD40 engagement stimulates IL-12 p70 production by human microglial cells: basis for Th1 polarization in the CNS. J. Neuroimmunol. 102, 44–50 (2000).
Ford, A. L., Foulcher, E., Lemckert, F. A. & Sedgwick, J. D. Microglia induce CD4 T lymphocyte final effector function and death. J. Exp. Med. 184, 1737–1745 (1996).
Juedes, A. E. & Ruddle, N. H. Resident and infiltrating central nervous system APCs regulate the emergence and resolution of experimental autoimmune encephalomyelitis. J. Immunol. 166, 5168–5175 (2001).
Becher, B., Durell, B. G., Miga, A. V., Hickey, W. F. & Noelle, R. J. The clinical course of experimental autoimmune encephalomyelitis and inflammation is controlled by the expression of CD40 within the central nervous system. J. Exp. Med. 193, 967–974 (2001).
Heppner, F. L. et al. Experimental autoimmune encephalomyelitis repressed by microglial paralysis. Nature Med. 11, 146–152 (2005).
Nikcevich, K. M. et al. IFN-gamma-activated primary murine astrocytes express B7 costimulatory molecules and prime naive antigen-specific T cells. J. Immunol. 158, 614–621 (1997).
Anderson, A. C. et al. Promotion of tissue inflammation by the immune receptor Tim-3 expressed on innate immune cells. Science 318, 1141–1143 (2007).
Goverman, J., Perchellet, A. & Huseby, E. S. The role of CD8+ T cells in multiple sclerosis and its animal models. Curr. Drug Targets Inflamm. Allergy 4, 239–245 (2005).
Friese, M. A. & Fugger, L. Autoreactive CD8+ T cells in multiple sclerosis: a new target for therapy? Brain 128, 1747–1763 (2005).
Coles, A. J. et al. The window of therapeutic opportunity in multiple sclerosis: evidence from monoclonal antibody therapy. J. Neurol. 253, 98–108 (2006).
Junker, A. et al. Multiple sclerosis: T-cell receptor expression in distinct brain regions. Brain 130, 2789–2799 (2007).
Crawford, M. P. et al. High prevalence of autoreactive, neuroantigen-specific CD8+ T cells in multiple sclerosis revealed by novel flow cytometric assay. Blood 103, 4222–4231 (2004).
Brynedal, B. et al. HLA-A confers an HLA-DRB1 independent influence on the risk of multiple sclerosis. PLoS ONE 2, e664 (2007).
Burfoot, R. K. et al. SNP mapping and candidate gene sequencing in the class I region of the HLA complex: searching for multiple sclerosis susceptibility genes in Tasmanians. Tissue Antigens 71, 42–50 (2008).
Koh, D. R. et al. Less mortality but more relapses in experimental allergic encephalomyelitis in CD8−/− mice. Science 256, 1210–1213 (1992).
Jiang, H., Zhang, S.-l. & Pernis, B. Role of CD8+ T cells in murine experimental allergic encephalomyelitis. Science 256, 1213–1215 (1992).
Huseby, E. S. et al. A pathogenic role for myelin-specific CD8+ T cells in a model for multiple sclerosis. J. Exp. Med. 194, 669–676 (2001). This paper shows that CD8+ T cells specific for MBP can induce a distinct form of EAE that recapitulates some aspects of multiple sclerosis not seen in CD4+ T cell-mediated EAE.
Sun, D. et al. Myelin antigen-specific CD8+ T cells are encephalitogenic and produce severe disease in C57BL/6 mice. J. Immunol. 166, 7579–7587 (2001). This paper shows that CD8+ T cells specific for MOG can induce EAE pathology.
Friese, M. A. et al. Opposing effects of HLA class I molecules in tuning autoreactive CD8+ T cells in multiple sclerosis. Nature Med. 14, 1227–1235 (2008). This paper uses humanized mice to show that one HLA allele promotes induction of EAE mediated by CD8+ PLP-specific T cells and a different HLA allele protects from disease, thereby identifying mechanisms by which MHC class I alleles can determine susceptibility to multiple sclerosis.
Calzascia, T. et al. Homing phenotypes of tumor-specific CD8 T cells are predetermined at the tumor site by crosspresenting APCs. Immunity 22, 175–184 (2005).
Perchellet, A., Brabb, T. & Goverman, J. M. Crosspresentation by nonhematopoietic and direct presentation by hematopoietic cells induce central tolerance to myelin basic protein. Proc. Natl Acad. Sci. USA 105, 14040–14045 (2008).
Galea, I. et al. An antigen-specific pathway for CD8 T cells across the blood–brain barrier. J. Exp. Med. 204, 2023–2030 (2007).
Na, S. Y. et al. Naive CD8 T-cells initiate spontaneous autoimmunity to a sequestered model antigen of the central nervous system. Brain 131, 2353–2365 (2008).
Saxena, A. et al. Cutting edge: Multiple sclerosis-like lesions induced by effector CD8 T cells recognizing a sequestered antigen on oligodendrocytes. J. Immunol. 181, 1617–1621 (2008).
Serafini, B. et al. Dysregulated Epstein–Barr virus infection in the multiple sclerosis brain. J. Exp. Med. 204, 2899–2912 (2007).
Zang, Y. C. et al. Increased CD8+ cytotoxic T cell responses to myelin basic protein in multiple sclerosis. J. Immunol. 172, 5120–5127 (2004).
Tzartos, J. S. et al. Interleukin-17 production in central nervous system-infiltrating T cells and glial cells is associated with active disease in multiple sclerosis. Am. J. Pathol. 172, 146–155 (2008).
Lafaille, J. J., Nagashima, K., Katsuki, M. & Tonegawa, S. High incidence of spontaneous autoimmune encephalomyelitis in immunodeficient anti-myelin basic protein T cell receptor transgenic mice. Cell 78, 399–408 (1994).
McGeachy, M. J., Stephens, L. A. & Anderton, S. M. Natural recovery and protection from autoimmune encephalomyelitis: contribution of CD4+CD25+ regulatory cells within the central nervous system. J. Immunol. 175, 3025–3032 (2005).
Korn, T. et al. Myelin-specific regulatory T cells accumulate in the CNS but fail to control autoimmune inflammation. Nature Med. 13, 423–431 (2007).
Pender, M. P. Treating autoimmune demyelination by augmenting lymphocyte apoptosis in the central nervous system. J. Neuroimmunol. 191, 26–38 (2007).
O'Connor, R. A. & Anderton, S. M. Foxp3+ regulatory T cells in the control of experimental CNS autoimmune disease. J. Neuroimmunol. 193, 1–11 (2008).
Malek, T. R. The biology of interleukin-2. Annu. Rev. Immunol. 26, 453–479 (2008).
Zozulya, A. L. & Wiendl, H. The role of CD8 suppressors versus destructors in autoimmune central nervous system inflammation. Hum. Immunol. 69, 797–804 (2008).
Rifa'i, M. et al. CD8+CD122+ regulatory T cells recognize activated T cells via conventional MHC class I–αβTCR interaction and become IL-10-producing active regulatory cells. Int. Immunol. 20, 937–947 (2008).
Feger, U. et al. HLA-G. expression defines a novel regulatory T-cell subset present in human peripheral blood and sites of inflammation. Blood 110, 568–577 (2007).
Najafian, N. et al. Regulatory functions of CD8+CD28− T cells in an autoimmune disease model. J. Clin. Invest. 112, 1037–1048 (2003).
Vlad, G., Cortesini, R. & Suciu-Foca, N. License to heal: bidirectional interaction of antigen-specific regulatory T cells and tolerogenic APC. J. Immunol. 174, 5907–5914 (2005).
Jiang, H. et al. Regulatory CD8+ T cells fine-tune the myelin basic protein-reactive T cell receptor Vβ repertoire during experimental autoimmune encephalomyelitis. Proc. Natl Acad. Sci. USA 100, 8378–8383 (2003).
Lu, L., Kim, H. J., Werneck, M. B. & Cantor, H. Regulation of CD8+ regulatory T cells: interruption of the NKG2A–Qa-1 interaction allows robust suppressive activity and resolution of autoimmune disease. Proc. Natl Acad. Sci. USA 105, 19420–19425 (2008).
Zhang, J., Medaer, R., Stinissen, P., Hafler, D. & Raus, J. MHC-restricted depletion of human myelin basic protein-reactive T cells by T cell vaccination. Science 261, 1451–1454 (1993).
Correale, J. et al. T cell vaccination in secondary progressive multiple sclerosis. J. Neuroimmunol. 107, 130–139 (2000).
Tennakoon, D. K. et al. Therapeutic induction of regulatory, cytotoxic CD8+ T cells in multiple sclerosis. J. Immunol. 176, 7119–7129 (2006).
Wyss-Coray, T., Borrow, P., Brooker, M. J. & Mucke, L. Astroglial overproduction of TGF-β1 enhances inflammatory central nervous system disease in transgenic mice. J. Neuroimmunol. 77, 45–50 (1997).
Luo, J. et al. Glia-dependent TGF-β signaling, acting independently of the TH17 pathway, is critical for initiation of murine autoimmune encephalomyelitis. J. Clin. Invest. 117, 3306–3315 (2007).
Bettelli, E. et al. IL-10 is critical in the regulation of autoimmune encephalomyelitis as demonstrated by studies of IL-10- and IL-4-deficient and transgenic mice. J. Immunol. 161, 3299–3306 (1998).
Stumhofer, J. S. et al. Interleukin 27 negatively regulates the development of interleukin 17-producing T helper cells during chronic inflammation of the central nervous system. Nature Immunol. 7, 937–945 (2006).
Fitzgerald, D. C. et al. Suppressive effect of IL-27 on encephalitogenic Th17 cells and the effector phase of experimental autoimmune encephalomyelitis. J. Immunol. 179, 3268–3275 (2007).
Pflanz, S. et al. IL-27, a heterodimeric cytokine composed of EBI3 and p28 protein, induces proliferation of naive CD4+ T cells. Immunity 16, 779–790 (2002).
Batten, M. et al. Interleukin 27 limits autoimmune encephalomyelitis by suppressing the development of interleukin 17-producing T cells. Nature Immunol. 7, 929–936 (2006).
Kleinschek, M. A. et al. IL-25 regulates Th17 function in autoimmune inflammation. J. Exp. Med. 204, 161–170 (2007).
Ousman, S. S. et al. Protective and therapeutic role for αB-crystallin in autoimmune demyelination. Nature 448, 474–479 (2007).
Beriou, G. et al. IL-17 producing human peripheral regulatory T cells retain suppressive function. Blood 26 Jan 2009 (doi:10.1182/blood-2008-10-183251).
Voo, K. S. et al. Identification of IL-17-producing FOXP3+ regulatory T cells in humans. Proc. Natl Acad. Sci. USA 106, 4793–4798 (2009).
Blink, S. E. & Miller, S. D. The contribution of γδ T cells to the pathogenesis of EAE and MS. Curr. Mol. Med. 9, 15–22 (2009).
Ponomarev, E. D. & Dittel, B. N. γδ T cells regulate the extent and duration of inflammation in the central nervous system by a Fas ligand-dependent mechanism. J. Immunol. 174, 4678–4687 (2005).
Lees, J. R., Iwakura, Y. & Russell, J. H. Host T cells are the main producers of IL-17 within the central nervous system during initiation of experimental autoimmune encephalomyelitis induced by adoptive transfer of Th1 cell lines. J. Immunol. 180, 8066–8072 (2008).
Hauser, S. L. et al. B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N. Engl. J. Med. 358, 676–688 (2008). This paper reports the findings of a Phase II clinical trial that indicate depletion of B cells mediated by rituximab is beneficial in patients with multiple sclerosis.
McLaughlin, K. A. & Wucherpfennig, K. W. B cells and autoantibodies in the pathogenesis of multiple sclerosis and related inflammatory demyelinating diseases. Adv. Immunol. 98, 121–149 (2008).
Colombo, M. et al. Accumulation of clonally related B lymphocytes in the cerebrospinal fluid of multiple sclerosis patients. J. Immunol. 164, 2782–2789 (2000).
Serafini, B., Rosicarelli, B., Magliozzi, R., Stigliano, E. & Aloisi, F. Detection of ectopic B-cell follicles with germinal centers in the meninges of patients with secondary progressive multiple sclerosis. Brain Pathol. 14, 164–174 (2004).
Magliozzi, R. et al. Meningeal B-cell follicles in secondary progressive multiple sclerosis associate with early onset of disease and severe cortical pathology. Brain 130, 1089–1104 (2007).
Iglesias, A., Bauer, J., Litzenburger, T., Schubart, A. & Linington, C. T- and B-cell responses to myelin oligodendrocyte glycoprotein in experimental autoimmune encephalomyelitis and multiple sclerosis. Glia 36, 220–234 (2001).
Mathey, E. K. et al. Neurofascin as a novel target for autoantibody-mediated axonal injury. J. Exp. Med. 204, 2363–2372 (2007).
Bettelli, E., Baeten, D., Jager, A., Sobel, R. A. & Kuchroo, V. K. Myelin oligodendrocyte glycoprotein-specific T and B cells cooperate to induce a Devic-like disease in mice. J. Clin. Invest. 116, 2393–2402 (2006).
Krishnamoorthy, G., Lassmann, H., Wekerle, H. & Holz, A. Spontaneous opticospinal encephalomyelitis in a double-transgenic mouse model of autoimmune T cell/B cell cooperation. J. Clin. Invest. 116, 2385–2392 (2006).
Mann, M. K., Maresz, K., Shriver, L. P., Tan, Y. & Dittel, B. N. B cell regulation of CD4+CD25+ T regulatory cells and IL-10 via B7 is essential for recovery from experimental autoimmune encephalomyelitis. J. Immunol. 178, 3447–3456 (2007).
Fillatreau, S., Sweenie, C. H., McGeachy, M. J., Gray, D. & Anderton, S. M. B cells regulate autoimmunity by provision of IL-10. Nature Immunol. 3, 944–950 (2002).
Matsushita, T., Yanaba, K., Bouaziz, J. D., Fujimoto, M. & Tedder, T. F. Regulatory B cells inhibit EAE initiation in mice while other B cells promote disease progression. J. Clin. Invest. 118, 3420–3430 (2008).
Duddy, M. et al. Distinct effector cytokine profiles of memory and naive human B cell subsets and implication in multiple sclerosis. J. Immunol. 178, 6092–6099 (2007).
Chung, Y. et al. Critical regulation of early TH17 cell differentiation by interleukin-1 signalling. Immunity 30, 576–587 (2009).
Acknowledgements
J. Goverman's research is supported by grants from the National Multiple Sclerosis Society (RG3851-A-5) and from the National Institutes of Health (AI073726, AI072737)
Author information
Authors and Affiliations
Related links
Glossary
- Multiple sclerosis
-
An inflammatory neurodegenerative disorder characterized by demyelination of bundles of nerves in the central nervous system. Symptoms depend on the site of the lesion but can include sensory loss, weakness in leg muscles, speech difficulties, loss of coordination and dizziness. Multiple sclerosis is thought to be an autoimmune response against components of myelin.
- Neuromyelitis optica
-
A relapsing, demyelinating inflammatory disorder that affects predominantly the optic nerves and spinal cord. Pathogenesis of neuromyelitis optica seems to depend on the generation of antibodies that are specific for aquaporin 4, an abundant water channel in the central nervous system.
- Acute disseminated encephalomyelitis
-
A monophasic, inflammatory, demyelinating disease of the central nervous system, frequently affecting children.
- Blood–brain barrier
-
A physiological barrier between blood vessels and brain parenchyma. It is formed by specialized, tight junctions between endothelial cells of the blood vessel wall, which is surrounded by a basement membrane, and an additional membrane formed from astrocyte feet and microglial cells.
- Demyelination
-
Damage to the myelin sheath surrounding nerves in the central nervous system, which affects the function of the nerves involved.
- Tight junction
-
An intercellular junction that joins the plasma membranes of adjacent epithelial or endothelial cells that regulate paracellular flux. Tight junction proteins include the integral membrane proteins occludin and claudin, in association with cytoplasmic zonula occludens proteins.
- Oligodendrocyte
-
The myelin-forming cell of the central nervous system.
- Mimicry
-
Structural similarity between epitopes contained within microbial and host proteins, leading to crossreactivity of T cells in the host.
- Wallerian degeneration
-
The degeneration of an axon distal to a site of injury, which begins to occur about 1.5 days after a lesion is formed.
- Degenerate TCR
-
A T cell receptor (TCR) that can bind to multiple distinct peptide–MHC complexes.
- Meninges
-
The membraneous region surrounding the brain and spinal cord. There are three membranes contained within the meninges: the dura mater (outer), the arachnoid membrane (middle) and the pia mater (inner). The subarachnoid space lies between the arachnoid and pial membranes and is the region in which cerebrospinal fluid flows.
- Epitope spreading
-
This term is used to describe how an immune response generated against a single peptide (or epitope) could spread to include T cell specificities for other peptides (or epitopes) not only on the same autoantigen (intramolecular spreading) but also on other self molecules that are released during the inflammatory response in the target organ.
- Plasmacytoid DC
-
A dendritic cell (DC) that lacks myeloid markers such as CD11c and CD33 but expresses high levels of HLA-DR and CD123. These cells produce high levels of type I interferons (IFNα and IFNβ) after activation.
- Perforin
-
A component of cytolytic granules that participates in the permeabilization of plasma membranes, allowing granzymes and other cytotoxic components to enter target cells.
Rights and permissions
About this article
Cite this article
Goverman, J. Autoimmune T cell responses in the central nervous system. Nat Rev Immunol 9, 393–407 (2009). https://doi.org/10.1038/nri2550
Issue Date:
DOI: https://doi.org/10.1038/nri2550