Abstract
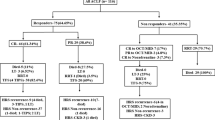
Hepatorenal syndrome (HRS) is a serious complication of advanced cirrhosis with ascites. HRS develops as a result of abnormal haemodynamics, leading to splanchnic and systemic vasodilatation, but renal vasoconstriction. Increased bacterial translocation, various cytokines and mesenteric angiogenesis also contribute to splanchnic vasodilatation, and altered renal autoregulation is involved in the renal vasoconstriction. Type 1 HRS is usually initiated by a precipitating event associated with an exaggerated systemic inflammatory response that perturbs haemodynamics, resulting in multiorgan failure. An inadequate cardiac output with systolic incompetence increases the risk of renal failure. Vasoconstrictors are the main treatment in patients with type 1 HRS; terlipressin is the superior agent. Norepinephrine is similar to terlipressin in efficacy and can be used as an alternative. Transjugular intrahepatic portosystemic stent shunt might be applicable in a small number of patients with type 1 HRS and in most patients with type 2 HRS. Liver transplantation is the definitive treatment for HRS, and should be performed after reversal of HRS. In nonresponders to vasoconstrictor therapy, much controversy still exists as to whether to do simultaneous or sequential liver and kidney transplant. In general, patients who have had >8–12 weeks of pretransplant dialysis should be considered for combined liver–kidney transplantation.
Key Points
-
Hepatorenal syndrome (HRS) in patients with cirrhosis is the result of haemodynamic derangement, which is initiated by portal hypertension and ultimately leads to renal vasoconstriction
-
The diagnosis of HRS has been simplified to enable earlier and easier diagnosis, so that treatment can be started early in the course of the illness
-
Vasoconstrictors are the primary treatment to improve systemic and splanchnic haemodynamics in HRS; terlipressin is superior to midodrine, but norepinephrine is also efficacious and is cheaper than terlipressin
-
Patients with cirrhosis, ascites and HRS who do not respond to vasoconstrictor therapy should be offered liver transplantation early; bridging dialysis is often required until liver transplantation
-
Patients who have had >8–12 weeks of pretransplant dialysis should be considered for combined liver–kidney transplantation to improve patient outcomes
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Garcia-Tsao, G., Parikh, C. R. & Viola A. Acute kidney injury in cirrhosis. Hepatology 48, 2064–2077 (2008).
Wong, F. in Schiff's Diseases of the Liver 11th edn (eds Schiff, E. R., Maddrey, W. C. & Sorrell, M. F.) 354–371 (Wiley-Blackwell, 2011).
Schrier, R. et al. Peripheral arterial vasodilatation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology 8, 1151–1157 (1988).
Salerno, F., Gerbes, A., Ginès, P., Wong, F. & Arroyo, V. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut 56, 1310–1318 (2007).
Montoliu, S. et al. Incidence and prognosis of different types of functional renal failure in cirrhotic patients with ascites. Clin. Gastroenterol. Hepatol. 8, 616–622 (2010).
Ginès, P., Guevara, M., Arroyo, V. & Rodés, J. Hepatorenal syndrome. Lancet 362, 1819–1827 (2003).
Martin, P. Y., Ginès, P. & Schrier, R. W. Nitric oxide as a mediator of hemodynamic abnormalities and sodium and water retention in cirrhosis. N. Engl. J. Med. 339, 533–541 (1998).
Van Landeghem, L. et al. Carbon monoxide produced by intrasinusoidally located haem-oxygenase-1 regulates the vascular tone in cirrhotic rat liver. Liver Int. 29, 650–660 (2009).
Ros, J. et al. Endogenous cannabinoids: a new system involved in the homeostasis of arterial pressure in experimental cirrhosis in the rat. Gastroenterology 122, 85–93 (2002).
Bátkai, S. et al. Endocannabinoids acting at vascular CB1 receptors mediate the vasodilated state in advanced liver cirrhosis. Nat. Med. 7, 827–832 (2001).
Castro, A. et al. Intracellular calcium concentration in vascular smooth muscle cells of rats with cirrhosis. J. Hepatol. 21, 521–526 (1994).
Møller, S., Hobolth, L., Winkler, C., Bendtsen, F. & Christensen, E. Determinants of the hyperdynamic circulation and central hypovolaemia in cirrhosis. Gut 60, 1254–1259 (2011).
Follo, A. et al. Renal impairment after spontaneous bacterial peritonitis in cirrhosis: incidence, clinical course, predictive factors and prognosis. Hepatology 20, 1495–1501 (1994).
Fasolato, S. et al. Renal failure and bacterial infections in patients with cirrhosis: epidemiology and clinical features. Hepatology 45, 223–229 (2007).
Sugano, S. Endotoxin levels in cirrhotic rats with sterile and infected ascites. Gastroenterol. Jpn 27, 348–353 (1992).
Heller, J. et al. Effects of lipopolysaccharide on TNF-α production, hepatic NOS2 activity, and hepatic toxicity in rats with cirrhosis. J. Hepatol. 33, 376–381 (2000).
Wiest, R. et al. Bacterial translocation in cirrhotic rats stimulates eNOS-derived NO production and impairs mesenteric vascular contractility. J. Clin. Invest. 104, 1223–1233 (1999).
Albillos, A. et al. Increased lipopolysaccharide binding protein in cirrhotic patients with marked immune and hemodynamic derangement. Hepatology 37, 208–217 (2003).
Tazi, K. A. et al. Norfloxacin reduces aortic NO synthases and proinflammatory cytokine up-regulation in cirrhotic rats: role of Akt signaling. Gastroenterology 129, 303–314 (2005).
Cejudo-Martín, P. et al. Increased production of vascular endothelial growth factor in peritoneal macrophages of cirrhotic patients with spontaneous bacterial peritonitis. Hepatology 34, 487–493 (2001).
Fernandez, M. et al. Reversal of portal hypertension and hyperdynamic splanchnic circulation by combined vascular endothelial growth factor and platelet-derived growth factor blockade in rats. Hepatology 46, 1208–1217 (2007).
Bosch, J., Abraldes, J. G., Fernández, M. & García-Pagán, J. C. Hepatic endothelial dysfunction and abnormal angiogenesis: new targets in the treatment of portal hypertension. J. Hepatol. 53, 558–567 (2010).
Wong, F. Cirrhotic cardiomyopathy. Hepatol. Int. 3, 294–304 (2009).
Ruiz-del-Arbol, L. et al. Circulatory function and hepatorenal syndrome in cirrhosis. Hepatology 42, 439–447 (2005).
Krag, A., Bendtsen, F., Henriksen, J. H. & Møller, S. Low cardiac output predicts development of hepatorenal syndrome and survival in patients with cirrhosis and ascites. Gut 59, 105–110 (2010).
Ruiz-del-Arbol, L. et al. Systemic, renal, and hepatic hemodynamic derangement in cirrhotic patients with spontaneous bacterial peritonitis. Hepatology 38, 1210–1218 (2003).
Stadlbauer, V. et al. Relationship between activation of the sympathetic nervous system and renal blood flow autoregulation in cirrhosis. Gastroenterology 134, 111–119 (2008).
Salerno, F. et al. Diagnosis, treatment and survival of patients with hepatorenal syndrome: A survey on daily medical practice. J. Hepatol. 55, 1241–1248 (2011).
Mandal, A. K., Lansing, M. & Fahmy, A. Acute tubular necrosis in hepatorenal syndrome: an electron microscopy study. Am. J. Kidney Dis. 2, 363–374 (1982).
Trawalé, J. M. et al. The spectrum of renal lesions in patients with cirrhosis: a clinicopathological study. Liver Int. 30, 725–732 (2010).
Guevara, M. & Arroyo, V. Hepatorenal syndrome. Expert Opin. Pharmacother. 12, 1405–1417 (2011).
Cabrera, J. et al. Aminoglycoside nephrotoxicity in cirrhosis. Value of urinary β2-microglobulin to discriminate functional renal failure from acute tubular damage. Gastroenterology 82, 97–105 (1982).
Meyrier, A., Hill, G. S. & Simon, P. Ischemic renal diseases: new insights into old entities. Kidney Int. 54, 2–13 (1998).
Sersté, T., Lebrec, D., Valla, D. & Moreau, R. Incidence and characteristics of type 2 hepatorenal syndrome in patients with cirrhosis and refractory ascites. Acta Gastroenterol. Belg. 71, 9–14 (2008).
Jalan, R. Acute-on-chronic liver failure: from concept to a new syndrome. Curr. Opin. Crit. Care 17, 152 (2011).
Olsen, J. C. & Kamath, P. S. Acute-on-chronic liver failure: concept, natural history, and prognosis. Curr. Opin. Crit. Care 17, 165–169 (2011).
Gustot, T., Durand, F., Lebrec, D., Vincent, J. L. & Moreau, R. Severe sepsis in cirrhosis. Hepatology 50, 2022–2033 (2009).
Arroyo, V., Fernandez, J. & Ginès, P. Pathogenesis and treatment of hepatorenal syndrome. Semin. Liver Dis. 28, 81–95 (2008).
Leung, W., Al Beshir, M., Marquez, M., Renner, E. & Wong, F. Is type 1 hepatorenal syndrome reversible after liver transplantation? [abstract 653]. J. Hepatol. 56 (Suppl. 2), S258–S259 (2012).
Terg, R. et al. Serum creatinine and bilirubin predict renal failure and mortality in patients with spontaneous bacterial peritonitis: a retrospective study. Liver Int. 29, 415–419 (2009).
Sigal, S. H., Stanca, C. M., Fernández, J., Arroyo, V. & Navasa, M. Restricted use of albumin for spontaneous bacterial peritonitis. Gut 56, 597–599 (2007).
Poca, M. et al. Role of albumin in the treatment in patients with spontaneous bacterial peritonitis. Clin. Gastroenterol. Hepatol. 10, 309–315 (2012).
Sort, P. et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N. Engl. J. Med. 341, 403–409 (1999).
Chavez-Tapia, N. C. et al. Meta-analysis: antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding—an updated Cochrane review. Aliment. Pharmacol. Ther. 34, 509–518 (2011).
Saner, F. H., Canbay, A., Gerken, G. & Broelsch, C. E. Pharmacology, clinical efficacy and safety of terlipressin in esophageal varices bleeding, septic shock and hepatorenal syndrome. Expert Rev. Gastroenterol. Hepatol. 1, 207–217 (2007).
Chiu, K. W., Sheen, I. S. & Liaw, Y. F. A controlled study of glypressin versus vasopressin in the control of bleeding from oesophageal varices. J. Gastroenterol. Hepatol. 5, 549–553 (1990).
Sanyal, A. J. et al. A randomized, prospective, double-blind, placebo-controlled trial of terlipressin for type 1 hepatorenal syndrome. Gastroenterology 134, 1360–1368 (2008).
Martín-Llahí, M. et al. Terlipressin and albumin vs albumin in patients with cirrhosis and hepatorenal syndrome: a randomized study. Gastroenterology 134, 1352–1359 (2008).
Boyer, T. D. et al. Predictors of response to terlipressin plus albumin in hepatorenal syndrome (HRS) type 1: relationship of serum creatinine to hemodynamics. J. Hepatol. 55, 315–321 (2011).
Nazar, A. et al. Predictors of response to therapy with terlipressin and albumin in patients with cirrhosis and type 1 hepatorenal syndrome. Hepatology 51, 219–226 (2010).
Wong, F. Drug insight: the role of albumin in the management of chronic liver disease. Nat. Clin. Pract. Gastroenterol. Hepatol. 4, 43–51 (2007).
Nilsson, G., Lindblom, P., Ohlin, M., Berling, R. & Vernersson, E. Pharmacokinetics of terlipressin after single i.v. doses to healthy volunteers. Drugs Exp. Clin. Res. 16, 307–314 (1990).
Angeli, P. et al. Terlipressin given as continuous intravenous infusion is the more suitable schedule for the treatment of type 1 hepatorenal syndrome (HRS) in patients with cirrhosis: results of a controlled clinical trial [abstract LB3]. Hepatology 48 (Suppl.), 378A (2008).
Gerbes, A. L., Huber, E. & Gülberg, V. Terlipressin for hepatorenal syndrome: continuous infusion as an alternative to i.v. bolus administration. Gastroenterology 137, 1179–1181 (2009).
Escorsell, A. et al. Time profile of the haemodynamic effects of terlipressin in portal hypertension. J. Hepatol. 26, 621–627 (1997).
Piano, S. et al. Continuous recurrence of type 1 hepatorenal syndrome and long-term treatment with terlipressin and albumin: a new exception to MELD score in the allocation system to liver transplantation? J. Hepatol. 55, 491–496 (2011).
Angeli, P. et al. Reversal of type 1 hepatorenal syndrome with the administration of midodrine and octreotide. Hepatology 29, 1690–1697 (1999).
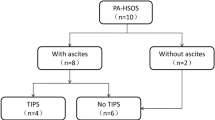
Wong, F., Pantea, L. & Sniderman, K. Midodrine, octreotide, albumin and TIPS in selected patients with cirrhosis and type 1 hepatorenal syndrome. Hepatology 40, 55–64 (2004).
Esrailian, E., Pantangco, E. R., Kyulo, N. L., Hu, K. Q. & Runyon, B. A. Octreotide/midodrine therapy significantly improves renal function and 30-day survival in patients with type 1 hepatorenal syndrome. Dig. Dis. Sci. 52, 742–748 (2007).
Cavallin, M. et al. Terlipressin and albumin vs. midodrine plus octreotide and albumin in the treatment of hepatorenal syndrome in patients with cirrhosis: results of a controlled clinical trial by the Italian Association for the Study of the Liver [abstract LB-2]. Hepatology 54 (Suppl. 1), 1426A (2011).
Rice, J. P., Skagen, C. & Said, A. Liver transplant outcomes for patients with hepatorenal syndrome treated with pretransplant vasoconstrictors and albumin. Transplantation 91, 1141–1147 (2011).
Sharma, P., Kumar, A., Shrama, B. C. & Sarin, S. K. An open label, pilot, randomized controlled trial of noradrenaline versus terlipressin in the treatment of type 1 hepatorenal syndrome and predictors of response. Am. J. Gastroenterol. 103, 1689–1697 (2008).
Alessandria, C. et al. Noradrenalin vs terlipressin in patients with hepatorenal syndrome: a prospective, randomized, unblinded, pilot study. J. Hepatol. 47, 499–505 (2007).
Singh, V. et al. Noradrenaline versus terlipressin in the treatment of hepatorenal syndrome: a randomized study. J. Hepatol. http://dx.doi.org/10.1016/j.jhep.2012.01.012.
Gluud, L. L., Christensen, K., Christensen, E. & Krag, A. Systematic review of randomized trials on vasoconstrictor drugs for hepatorenal syndrome. Hepatology 51, 576–584 (2010).
Sagi, S. V., Mittal, S., Kasturi, K. S. & Sood, G. K. Terlipressin therapy for reversal of type 1 hepatorenal syndrome: a meta-analysis of randomized controlled trials. J. Gastroenterol. Hepatol. 25, 880–885 (2010).
Guevara, M. et al. Transjugular intrahepatic portosystemic shunt in hepatorenal syndrome: effects on renal function and vasoactive systems. Hepatology 28, 416–422 (1998).
Brensing, K. A. et al. Transjugular intrahepatic portosystemic stent-shunt for hepatorenal syndrome. Lancet 349, 697–698 (1997).
Brensing, K. A. et al. Long term outcome after transjugular intrahepatic portosystemic stent-shunt in non-transplant cirrhotics with hepatorenal syndrome: a phase II study. Gut 47, 288–295 (2000).
Jalan, R. et al. Extracorporeal liver support with molecular adsorbents recirculating system in patients with severe acute alcoholic hepatitis. J. Hepatol. 38, 24–31 (2003).
Di Campli, C. et al. Catholic university experience with molecular adsorbent recycling system in patients with severe liver failure. Transplant. Proc. 37, 2547–2550 (2005).
Mitzner, S. R. et al. Improvement of hepatorenal syndrome with extracorporeal albumin dialysis MARS: Results of a prospective, randomized, controlled clinical trial. Liver Transpl. 6, 277–286 (2000).
Wong, F., Raina, N. & Richardson, R. Molecular adsorbent recirculating system is ineffective in the management of type 1 hepatorenal syndrome in patients with cirrhosis with ascites who have failed vasoconstrictor treatment. Gut 59, 381–386 (2010).
Ruiz-del-Arbol, L. et al. Paracentesis-induced circulatory dysfunction: mechanism and effect on hepatic hemodynamics in cirrhosis. Gastroenterology 113, 579–586 (1997).
Ortega, R. et al. Terlipressin therapy with and without albumin for patients with hepatorenal syndrome: results of a prospective, nonrandomized study. Hepatology 36, 941–948 (2002).
Testino, G. et al. Type-2 hepatorenal syndrome and refractory ascites: role of transjugular intrahepatic portosystemic stent-shunt in eighteen patients with advanced cirrhosis awaiting orthotopic liver transplantation. Hepatogastroenterology 50, 1753–1755 (2003).
Alessandria, C., Venon, W. & Marzano, A. Renal failure in cirrhotic patients: role of terlipressin in clinical approach to hepatorenal syndrome type 2. Eur. J. Gastroenterol. Hepatol. 14, 1363–1368 (2002).
Cassinello, C. et al. Effects of orthotopic liver transplantation on vasoactive systems and renal function in patients with advanced liver cirrhosis. Dig. Dis. Sci. 48, 179–186 (2003).
Wiesner, R. et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 124, 91–96 (2003).
Memon, I. & Klein, C. L. Impact of hepatorenal syndrome and liver transplantation. Curr. Opin. Organ. Transplant. 16, 301–305 (2011).
Restuccia, T. et al. Effects of treatment of hepatorenal syndrome before transplantation on posttransplantation outcome. A case-control study. J. Hepatol. 40, 140–146 (2004).
Ginès, P. Hepatorenal syndrome, pharmacological therapy, and liver transplantation. Liver Transpl. 17, 1244–1246 (2011).
Wong, L. P. et al. Survival of liver transplant candidates with acute renal failure receiving renal replacement therapy. Kidney Int. 68, 362–370 (2005).
Marik, P. E., Wood, K. & Starzl, T. E. The course of type 1 hepatorenal syndrome post liver transplantation. Nephrol. Dial. Transplant. 21, 478–482 (2006).
Hadengue, A. et al. Persistence of systemic and splanchnic hyperkinetic circulation in liver transplant patients. Hepatology 17, 175–178 (1993).
Davis, C. L. et al. Simultaneous liver–kidney transplantation: evaluation to decision making. Am. J. Transplant. 7, 1702–1709 (2007).
Papafragkakis, H., Martin, P. & Akalin, E. Combined liver and kidney transplantation. Curr. Opin. Organ. Transplant. 15, 263–268 (2010).
Locke, J. E. et al. Declining outcomes in simultaneous liver-kidney transplantation in the MELD era: ineffective usage of renal allografts. Transplantation 85, 935–942 (2008).
Ruiz, R. et al. Hepatorenal syndrome: a proposal for kidney after liver transplantation (KALT). Liver Transpl. 13, 838–843 (2007).
Somsouk, M. et al. Ascites improves upon serum sodium plus model for end-stage liver disease (MELD) for predicting mortality in patients with advanced liver disease. Aliment. Pharmacol. Ther. 30, 741–748 (2009).
Somsouk, M., Kornfield, R., Vittinghoff, E., Inadomi, J. M. & Biggins, S. W. Moderate ascites identifies patients with low model for end-stage liver disease scores awaiting liver transplantation who have a high mortality risk. Liver Transpl. 17, 129–136 (2011).
Fernández, J. et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology 133, 818–824 (2007).
Lebrec, D. et al. Pentoxifylline does not decrease short-term mortality but does reduce complications in patients with advanced cirrhosis. Gastroenterology 138, 1755–1762 (2010).
Akriviadis, E. et al. Pentoxifylline improves short-term survival in severe acute alcoholic hepatitis: a double-blind, placebo-controlled trial. Gastroenterology 119, 1637–1648 (2000).
Whitfield, K., Rambaldi, A., Wetterslev, J. & Gluud, C. Pentoxifylline for alcoholic hepatitis. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD007339. http://dx.doi.org/10.1002/14651858.CD007339.pub2.
Lake, J. R. et al. Transjugular intrahepatic portacaval stent shunts in patients with renal insufficiency. Transplant. Proc. 25, 1766–1767 (1993).
Spahr, L. et al. Improvement of hepatorenal syndrome by transjugular intrahepatic portosystemic shunt. Am. J. Gastroenterol. 90, 1169–1171 (1995).
Author information
Authors and Affiliations
Ethics declarations
Competing interests
F. Wong has received grant/research support from Ikaria.
Rights and permissions
About this article
Cite this article
Wong, F. Recent advances in our understanding of hepatorenal syndrome. Nat Rev Gastroenterol Hepatol 9, 382–391 (2012). https://doi.org/10.1038/nrgastro.2012.96
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2012.96
This article is cited by
-
VWF/ADAMTS13 Ratio as a Potential Predictive Biomarker for Acute Kidney Injury Onset in Cirrhosis
Digestive Diseases and Sciences (2024)
-
Urine neutrophil gelatinase-associated lipocalin as a biomarker of acute kidney injury and prognosis in decompensated chronic liver disease: A prospective study
Indian Journal of Gastroenterology (2023)
-
Austrian consensus on the diagnosis and management of portal hypertension in advanced chronic liver disease (Billroth IV)
Wiener klinische Wochenschrift (2023)
-
Do old urinary biomarkers have a place in the new definition of hepatorenal syndrome in the Egyptian cirrhotic patients? A single-center experience
Egyptian Liver Journal (2022)
-
Acute kidney injury: prediction, prognostication and optimisation for liver transplant
Hepatology International (2020)