Abstract
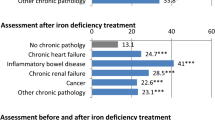
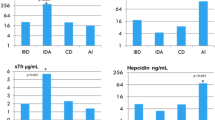
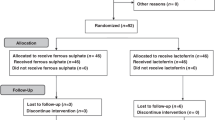
Anemia is the most prevalent extraintestinal complication of IBD. It can affect quality of life and ability to work, and can also increase the hospitalization rate in patients with IBD. Although the causes of anemia in IBD are multifactorial, iron deficiency anemia (IDA) is the most common. Assessment of the iron status of patients who have a condition associated with inflammation, such as IBD, by using common biochemical values is insufficient. However, new indices of iron metabolism (for instance ferritin:transferrin receptor ratio, reticulocyte hemoglobin content or percentage of hypochromic red blood cells) may help to improve the assessment of iron status in patients with IBD. The treatment of IDA traditionally involves oral iron supplementation. However, because of extensive gastrointestinal adverse effects, and data showing that the use of oral iron in IBD may be associated with disease exacerbation, current guidelines suggest that iron supplementation in IBD should be administered intravenously. This Review provides an overview of iron homeostasis in health before discussing diagnostic and therapeutic strategies for IDA in patients with IBD.
Key Points
-
Anemia is the most prevalent extraintestinal complication of IBD
-
Although there are several causes of anemia in IBD, iron deficiency anemia (IDA) is the most common
-
Common biochemical values are insufficient for assessing the iron status of patients who have an inflammatory condition, such as IBD
-
The major goal of therapy for IDA is to supply sufficient iron to increase hemoglobin levels by >2 g/dl or increase them to normal values within 4 weeks, and to replenish iron stores
-
Iron supplementation should be administered intravenously to patients with IBD, even though many will respond to oral administration of iron
-
Compared with oral iron therapy, in patients with IBD intravenous iron replenishes iron stores more effectively and overcomes the block to intestinal iron absorption induced by hepcidin
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Gasche, C., Lomer, M. C., Cavill, I. & Weiss, G. Iron, anaemia, and inflammatory bowel diseases. Gut 53, 1190–1197 (2004).
Vijverman, A., Piront, P., Belaiche, J. & Louis, E. Evolution of the prevalence and characteristics of anemia in inflammatory bowel diseases between 1993 and 2003. Acta Gastroenterol. Belg. 69, 1–4 (2006).
Wilson, A., Reyes, E. & Ofman, J. Prevalence and outcomes of anemia in inflammatory bowel disease: a systematic review of the literature. Am. J. Med. 116 (Suppl. 7A), 44S–49S (2004).
Gisbert, J. P. & Gomollon, F. Common misconceptions in the diagnosis and management of anemia in inflammatory bowel disease. Am. J. Gastroenterol. 103, 1299–1307 (2008).
Kullnigg, S. & Gasche, C. Systemic review: managing anaemia in Crohn's disease. Aliment. Pharmacol. Ther. 24, 1507–1523 (2006).
Wells, C. W., Lewis, S., Barton, J. R. & Corbett, S. Effects of changes in hemoglobin level on quality of life and cognitive function in inflammatory bowel disease patients. Inflamm. Bowel Dis. 12, 123–130 (2006).
Munoz, M., Villar, I. & Garcia-Erce, J. A. An update on iron physiology. World J. Gastroenterol. 15, 4617–4626 (2009).
Hurrell, R. & Egli, I. Iron bioavailability and dietary reference values. Am. J. Clin. Nutr. 91, 1461S–1467S (2010).
Geisser, P. Safety and efficacy of iron(III)-hydroxide polymaltose complex/a review of over 25 years experience. Arzneimittelforschung 57, 439–452 (2007).
Barrett, J. F., Witthaker, P. G., Williams, J. G. & Lind, T. Absorption of non-haem iron from food during normal pregnancy. BMJ 309, 79–82 (1994).
Schade, S. G., Cohen, R. J. & Conrad, M. E. Effect of hydrochloric acid on iron absorption. N. Engl. J. Med. 279, 672–674 (1968).
McColl, K. E. Effect of proton pump inhibitors on vitamins and iron. Am. J. Gastroenterol. 104 (Suppl. 2), S5–S9 (2009).
Frazer, D. M. & Anderson, G. J. Iron imports. I. Intestinal iron absorption and its regulation. Am. J. Physiol. Gastrointest. Liver Physiol. 289, G631–G635 (2005).
Shayeghi, M. et al. Identification of an intestinal heme transporter. Cell 122, 789–801 (2005).
Qiu, A. et al. Identification of an intestinal folate transporter and the molecular basis for hereditary folate malabsorption. Cell 127, 917–928 (2006).
Lopez, M. A. & Martos, F. C. Iron availability: an update review. Int. J. Food Sci. Nutr. 55, 597–606 (2004).
Geisser, P. In vitro studies on interactions of iron salts and complexes with food-stuffs and medicaments. Arzneimittelforschung 40, 754–760 (1990).
Crichton, R. R., Danielson, B. G. & Geisser, P. Iron Therapy with Special Emphasis on Intravenous Administration (Uni-Med Verlag, Bremen, 2006).
Anderson, G. J., Frazer, D. M. & McLaren, G. D. Iron absorption and metabolism. Curr. Opin. Gastroenterol. 25, 129–135 (2009).
Collins, J. F., Wessling-Resnick, M. & Knutson, M. D. Hepcidin regulation of iron transport. J. Nutr. 138, 2284–2288 (2008).
Ganz, T. Molecular control of iron transport. J. Am. Soc. Nephrol. 18, 394–400 (2007).
Nemeth, E. et al. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science 306, 2090–2093 (2004).
De Domenico, I. et al. The molecular mechanism of hepcidin-mediated ferroportin down-regulation. Mol. Biol. Cell 18, 2569–2578 (2007).
De Domenico, I., Lo, E., Ward, D. M. & Kaplan, J. Hepcidin-induced internalization of ferroportin requires binding and cooperative interaction with Jak2. Proc. Natl Acad. Sci. USA 106, 3800–3805 (2009).
Yamaji, S., Sharp, P., Ramesh, B. & Srai, S. K. Inhibition of iron transport across human intestinal epithelial cells by hepcidin. Blood 104, 2178–2180 (2004).
Mena, N. P., Esparza, A., Tapia, V., Valdes, P. & Nunez, M. T. Hepcidin inhibits apical iron uptake in intestinal cells. Am. J. Physiol. Gastrointest. Liver Physiol. 294, G192–G198 (2008).
Theurl, I. et al. Autocrine formation of hepcidin induces iron retention in human monocytes. Blood 111, 2392–2399 (2008).
Wrighting, D. M. & Andrews, N. C. Interleukin-6 induces hepcidin expression through STAT3. Blood 108, 3204–3209 (2006).
Verga Falzacappa, M. V. et al. STAT3 mediates hepatic hepcidin expression and its inflammatory stimulation. Blood 109, 353–358 (2007).
Arndt, S. et al. Iron-induced expression of bone morphogenic protein 6 in intestinal cells is the main regulator of hepatic hepcidin expression in vivo. Gastroenterology 138, 372–382 (2010).
Knutson, M. D. Iron-sensing proteins that regulate hepcidin and enteric iron absorption. Annu. Rev. Nutr. 30, 149–171 (2010).
Gasche, C. et al. Guidelines on the diagnosis and management of iron deficiency and anemia in inflammatory bowel diseases. Inflamm. Bowel Dis. 13, 1545–1553 (2007).
Hodges, P., Gee, M., Grace, M. & Thomson, A. B. Vitamin and iron intake in patients with Crohn's disease. J. Am. Diet. Assoc. 84, 52–58 (1984).
Lomer, M. C. et al. Intake of dietary iron is low in patients with Crohn's disease: a case–control study. Br. J. Nutr. 91, 141–148 (2004).
Cartwright, G. E. The anemia of chronic disorders. Semin. Hematol. 3, 351–375 (1966).
Weiss, G. & Gasche, C. Pathogenesis and treatment of anemia in inflammatory bowel disease. Haematologica 95, 175–178 (2010).
Andrews, N. C. Forging a field: the golden age of iron biology. Blood 112, 219–230 (2008).
Clark, S. F. Iron deficiency anemia: diagnosis and management. Curr. Opin. Gastroenterol. 25, 122–128 (2009).
Guagnozzi, D. et al. Ferritin as a simple indicator of iron deficiency in anemic IBD patients. Inflamm. Bowel Dis. 12, 150–151 (2006).
Das, S. & Philip, K. J. Evaluation of iron status: zinc protoporphyrin vis-a-vis bone marrow iron stores. Indian J. Pathol. Microbiol. 51, 105–107 (2008).
Metzgeroth, G. & Hastka, J. Diagnostic work-up of iron deficiency. J. Lab. Med. 28, 391–399 (2004).
Scrimgeour, A. G. & Condlin, M. L. Zinc and micronutrient combinations to combat gastrointestinal inflammation. Curr. Opin. Clin. Nutr. Metab. Care 12, 653–660 (2009).
Beguin, Y. Soluble transferrin receptor for the evaluation of erythropoiesis and iron status. Clin. Chim. Acta 329, 9–22 (2003).
Thomas, L. & Thomas, C. Anemia in iron deficiency and disorders of iron metabolism. Dtsch. Med. Wochenschr. 127, 1591–1594 (2002).
Punnonen, K., Irjala, K. & Rajamaki, A. Serum transferrin receptor and its ratio to serum ferritin in the diagnosis of iron deficiency. Blood 89, 1052–1057 (1997).
Mast, A. E., Blinder, M. A., Gronowski, A. M., Chumley, C. & Scott, M. G. Clinical utility of the soluble transferrin receptor and comparison with serum ferritin in several populations. Clin. Chem. 44, 45–51 (1998).
Wish, J. B. Assessing iron status: beyond serum ferritin and transferrin saturation. Clin. J. Am. Soc. Nephrol. 1 (Suppl. 1), S4–S8 (2006).
Fernández-Rodríguez, A. M. et al. Diagnosis of iron deficiency in chronic renal failure. Am. J. Kidney Dis. 34, 508–513 (1999).
Thomas, C. & Thomas, L. Biochemical markers and hematologic indices in the diagnosis of functional iron deficiency. Clin. Chem. 48, 1066–1076 (2002).
Mast, A. E., Blinder, M. A. & Dietzen, D. J. Reticulocyte hemoglobin content. Am. J. Hematol. 83, 307–310 (2008).
Brugnara, C. Iron deficiency and erythropoiesis: new diagnostic approaches. Clin. Chem. 49, 1573–1578 (2003).
Ganzoni, A. M. Intravenous iron-dextran: therapeutic and experimental possibilities [German]. Schweiz. Med. Wochenschr. 100, 301–303 (1970).
Zhu, A., Kaneshiro, M. & Kaunitz, J. D. Evaluation and treatment of iron deficiency anemia: a gastroenterological perspective. Dig. Dis. Sci. 55, 548–559 (2010).
Rimon, E. et al. Are we giving too much iron? Low-dose iron therapy is effective in octogenarians. Am. J. Med. 118, 1142–1147 (2005).
Zhou, S. J., Gibson, R. A., Crowther, C. A. & Makrides, M. Should we lower the dose of iron when treating anaemia in pregnancy? A randomized dose-response trial. Eur. J. Clin. Nutr. 63, 183–190 (2009).
Semrin, G. et al. Impaired intestinal iron absorption in Crohn's disease correlates with disease activity and markers of inflammation. Inflamm. Bowel Dis. 12, 1101–1106 (2006).
Schroder, O. et al. Intravenous iron sucrose versus oral iron supplementation for the treatment of iron deficiency anemia in patients with inflammatory bowel disease—a randomized, controlled, open-label, multicenter study. Am. J. Gastroenterol. 100, 2503–2509 (2005).
Haig, A. & Driman, D. K. Iron-induced mucosal injury to the upper gastrointestinal tract. Histopathology 48, 808–812 (2006).
Kaye, P. et al. Iron-induced mucosal pathology of the upper gastrointestinal tract: a common finding in patients on oral iron therapy. Histopathology 53, 311–317 (2008).
Carrier, J., Aghdassi, E., Platt, I., Cullen, J. & Allard, J. P. Effect of oral iron supplementation on oxidative stress and colonic inflammation in rats with induced colitis. Aliment. Pharmacol. Ther. 15, 1989–1999 (2001).
Carrier, J., Aghdassi, E., Cullen, J. & Allard, J. P. Iron supplementation increases disease activity and vitamin E ameliorates the effect in rats with dextran sulfate sodium-induced colitis. J. Nutr. 132, 3146–3150 (2002).
Klopcic, B., Chua, A., Loh, L. L., Trinder, D. & Lawrance, I. C. Increased dietary iron increases the level of chronic intestine inflammation and the development of colonic tumorgenesis in the mouse. Gastroenterology 136, A90 (2009).
Erichsen, K. et al. Oral ferrous fumarate or intravenous iron sucrose for patients with inflammatory bowel disease. Scand. J. Gastroenterol. 40, 1058–1065 (2005).
Aghdassi, E., Carrier, J., Cullen, J., Tischler, M. & Allard, J. P. Effect of iron supplementation on oxidative stress and intestinal inflammation in rats with acute colitis. Dig. Dis. Sci. 46, 1088–1094 (2001).
Seril, D. N. et al. Dietary iron supplementation enhances DSS-induced colitis and associated colorectal carcinoma development in mice. Dig. Dis. Sci. 47, 1266–1278 (2002).
Seril, D. N., Liao, J., Yang, C. S. & Yang, G. Y. Systemic iron supplementation replenishes iron stores without enhancing colon carcinogenesis in murine models of ulcerative colitis: comparison with iron-enriched diet. Dig. Dis. Sci. 50, 696–707 (2005).
Troost, F. J. et al. Iron supplements inhibit zinc but not copper absorption in vivo in ileostomy subjects. Am. J. Clin. Nutr. 78, 1018–1023 (2003).
Sharma, J. B. et al. A prospective, partially randomized study of pregnancy outcomes and hematologic responses to oral and intramuscular iron treatment in moderately anemic pregnant women. Am. J. Clin. Nutr. 79, 116–122 (2004).
Bork, K. Localized cutaneous siderosis following intramuscular iron injections [German]. Hautarzt 35, 598–599 (1984).
MacKinnon, A. E. & Bancewicz, J. Sarcoma after injection of intramuscular iron. Br. Med. J. 2, 277–279 (1973).
Greenberg, G. Sarcoma after intramuscular iron injection. Br. Med. J. 1, 1508–1509 (1976).
Fielding, J. Does sarcoma occur in man after intramuscular iron? Scand. J. Haematol. Suppl. 32, 100–104 (1977).
Kaushansky, K. & Kipps, T. in Goodman & Gilman's The Pharmacological Basis of Therapeutics (eds Hardman, J. G., Limbird, L. E. & Gilman, A. G.) 1433–1466 (McGraw-Hill Professional, Maidenhead, 2005).
Auerbach, M., Ballard, H. & Glaspy, J. Clinical update: intravenous iron for anaemia. Lancet 369, 1502–1504 (2007).
Auerbach, M., Goodnough, L. T., Picard, D. & Maniatis, A. The role of intravenous iron in anemia management and transfusion avoidance. Transfusion 48, 988–1000 (2008).
Fletes, R., Lazarus, J. M., Gage, J. & Chertow, G. M. Suspected iron dextran-related adverse drug events in hemodialysis patients. Am. J. Kidney Dis. 37, 743–749 (2001).
Chertow, G. M., Mason, P. D., Vaage-Nilsen, O. & Ahlmen, J. On the relative safety of parenteral iron formulations. Nephrol. Dial. Transplant. 19, 1571–1575 (2004).
Chertow, G. M., Mason, P. D., Vaage-Nilsen, O. & Ahlmen, J. Update on adverse drug events associated with parenteral iron. Nephrol. Dial. Transplant. 21, 378–382 (2006).
Pharmacovigilance Working Party. May 2010 plenary meeting. European Medicines Agency [online], (2010).
Macdougall, I. C. Strategies for iron supplementation: oral versus intravenous. Kidney Int. Suppl. 69, S61–S66 (1999).
Ferriclet® (ferric gluconate injection) package insert (Sanofi-Aventis, 2010).
Geisser, P., Baer, M. & Schaub, E. Structure/histotoxicity relationship of parenteral iron preparations. Arzneimittelforschung 42, 1439–1452 (1992).
Schroder, O. et al. A study for the evaluation of safety and tolerability of intravenous high-dose iron sucrose in patients with iron deficiency anemia due to gastrointestinal bleeding. Z. Gastroenterol. 42, 663–667 (2004).
Venofer 20 mg/ml Solution for Injection. Electronic Medicines Compendium [online], (2006).
Szczech, L. A. et al. Randomized Evaluation of efficacy and safety of ferric carboxymaltose in Patients with iron deficiency Anaemia and Impaired Renal function (REPAIR-IDA): rationale and study design. Nephrol. Dial. Transplant. 25, 2368–2375 (2010).
Covic, A. & Mircescu, G. The safety and efficacy of intravenous ferric carboxymaltose in anaemic patients undergoing haemodialysis: a multi-centre, open-label, clinical study. Nephrol. Dial. Transplant. 25, 2722–2730 (2010).
Grimmelt, A. C., Cohen, C. D., Fehr, T., Serra, A. L. & Wuethrich, R. P. Safety and tolerability of ferric carboxymaltose (FCM) for treatment of iron deficiency in patients with chronic kidney disease and in kidney transplant recipients. Clin. Nephrol. 71, 125–129 (2009).
Tagboto, S., Cropper, L., Turner, J. & Pugh-Clarke, K. The efficacy of a single dose of intravenous ferric carboxymaltose (Ferinject) on anaemia in a pre-dialysis population of chronic kidney disease patients. J. Ren. Care 35, 18–23 (2009).
Anker, S. D. et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N. Engl. J. Med. 361, 2436–2448 (2009).
Breymann, C., Gliga, F., Bejenariu, C. & Strizhova, N. Comparative efficacy and safety of intravenous ferric carboxymaltose in the treatment of postpartum iron deficiency anemia. Int. J. Gynaecol. Obstet. 101, 67–73 (2008).
Van Wyck, D. B. et al. Large-dose intravenous ferric carboxymaltose injection for iron deficiency anemia in heavy uterine bleeding: a randomized, controlled trial. Transfusion 49, 2719–2728 (2009).
Seid, M. H. et al. Ferric carboxymaltose injection in the treatment of postpartum iron deficiency anemia: a randomized controlled clinical trial. Am. J. Obstet. Gynecol. 199, 435 e1–e7 (2008).
Kulnigg, S. et al. A novel intravenous iron formulation for treatment of anemia in inflammatory bowel disease: the ferric carboxymaltose (FERINJECT) randomized controlled trial. Am. J. Gastroenterol. 103, 1182–1192 (2008).
Evstatiev, R. et al. Efficacy and safety of standardised ferric carboxymaltose doses vs. individually calculated iron sucrose doses for IBD-associated iron deficiency anemia: a multicentre, randomised controlled trial. Presented at the 18th United European Gastroenterology Week (Barcelona, 2010).
Balakrishnan, V. S. et al. Physicochemical properties of ferumoxytol, a new intravenous iron preparation. Eur. J. Clin. Invest. 39, 489–496 (2009).
Lu, M., Cohen, M. H., Rieves, D. & Pazdur, R. FDA report: ferumoxytol for intravenous iron therapy in adult patients with chronic kidney disease. Am. J. Hematol. 85, 315–319 (2010).
Coyne, D. W. Ferumoxytol for treatment of iron deficiency anemia in patients with chronic kidney disease. Expert Opin. Pharmacother. 10, 2563–2568 (2009).
Bruining, D. H. & Loftus, E. V. Jr. Technology insight: new techniques for imaging the gut in patients with IBD. Nat. Clin. Pract. Gastroenterol. Hepatol. 5, 154–161 (2008).
Sinha, R. et al. Role of MRI in Crohn's disease. Clin. Radiol. 64, 341–352 (2009).
Gasche, C. et al. Intravenous iron and erythropoietin for anemia associated with Crohn disease. A randomized, controlled trial. Ann. Intern. Med. 126, 782–787 (1997).
Gasche, C. et al. Sequential treatment of anemia in ulcerative colitis with intravenous iron and erythropoietin. Digestion 60, 262–267 (1999).
Dohil, R., Hassall, E., Wadsworth, L. D. & Israel, D. M. Recombinant human erythropoietin for treatment of anemia of chronic disease in children with Crohn's disease. J. Pediatr. 132, 155–159 (1998).
Schreiber, S. et al. Recombinant erythropoietin for the treatment of anemia in inflammatory bowel disease. N. Engl. J. Med. 334, 619–623 (1996).
Koutroubakis, I. E. et al. Effectiveness of darbepoetin-alfa in combination with intravenous iron sucrose in patients with inflammatory bowel disease and refractory anaemia: a pilot study. Eur. J. Gastroenterol. Hepatol. 18, 421–425 (2006).
Kulnigg, S., Teischinger, L., Dejaco, C., Waldhor, T. & Gasche, C. Rapid recurrence of IBD-associated anemia and iron deficiency after intravenous iron sucrose and erythropoietin treatment. Am. J. Gastroenterol. 104, 1460–1467 (2009).
Kosch, M., Schaefer, R. M. & Bahner, U. Supplementation with minerals and trace elements. Iron, zinc and selenium [German]. Internist (Berl.) 43, 1299–1307 (2002).
Unger, E. F., Thompson, A. M., Blank, M. J. & Temple, R. Erythropoiesis-stimulating agents—time for a reevaluation. N. Engl. J. Med. 362, 189–192 (2010).
Bergamaschi, G. et al. Prevalence and pathogenesis of anemia in inflammatory bowel disease. Influence of anti-tumor necrosis factor-alpha treatment. Haematologica 95, 199–205 (2010).
de Vizia, B., Poggi, V., Conenna, R., Fiorillo, A. & Scippa, L. Iron absorption and iron deficiency in infants and children with gastrointestinal diseases. J. Pediatr. Gastroenterol. Nutr. 14, 21–26 (1992).
Gasche, C. et al. Anemia in Crohn's disease. Importance of inadequate erythropoietin production and iron deficiency. Dig. Dis. Sci. 39, 1930–1934 (1994).
Lakatos, L. et al. Association of extraintestinal manifestations of inflammatory bowel disease in a province of western Hungary with disease phenotype: results of a 25-year follow-up study. World J. Gastroenterol. 9, 2300–2307 (2003).
Ormerod, T. P. Observations on the incidence and cause of anaemia in ulcerative colitis. Gut 8, 107–114 (1967).
Revel-Vilk, S. et al. Serum transferrin receptor in children and adolescents with inflammatory bowel disease. Eur. J. Pediatr. 159, 585–589 (2000).
Bodemar, G., Kechagias, S., Almer, S. & Danielson, B. G. Treatment of anaemia in inflammatory bowel disease with iron sucrose. Scand. J. Gastroenterol. 39, 454–458 (2004).
Gasche, C. et al. Prediction of response to iron sucrose in inflammatory bowel disease-associated anemia. Am. J. Gastroenterol. 96, 2382–2387 (2001).
Gisbert, J. P. et al. Oral and intravenous iron treatment in inflammatory bowel disease: hematological response and quality of life improvement. Inflamm. Bowel Dis. 15, 1485–1491 (2009).
Katsanos, K. et al. Intravenous iron therapy restores functional iron deficiency induced by infliximab. J. Crohn's Colitis 1, 97–105 (2007).
Koutroubakis, I. E., Oustamanolakis, P., Karakoidas, C., Mantzaris, G. J. & Kouroumalis, E. A. Safety and efficacy of total-dose infusion of low molecular weight iron dextran for iron deficiency anemia in patients with inflammatory bowel disease. Dig. Dis. Sci. 55, 2327–2331 (2009).
Lindgren, S. et al. Intravenous iron sucrose is superior to oral iron sulphate for correcting anaemia and restoring iron stores in IBD patients: A randomized, controlled, evaluator-blind, multicentre study. Scand. J. Gastroenterol. 44, 838–845 (2009).
Mamula, P., Piccoli, D. A., Peck, S. N., Markowitz, J. E. & Baldassano, R. N. Total dose intravenous infusion of iron dextran for iron-deficiency anemia in children with inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 34, 286–290 (2002).
Zhu, Y. I. & Haas, J. D. Iron depletion without anemia and physical performance in young women. Am. J. Clin. Nutr. 66, 334–341 (1997).
Hinton, P. S., Giordano, C., Brownlie, T. & Haas, J. D. Iron supplementation improves endurance after training in iron-depleted, nonanemic women. J. Appl. Physiol. 88, 1103–1111 (2000).
Brownlie, T. 4th, Utermohlen, V., Hinton, P. S. & Haas, J. D. Tissue iron deficiency without anemia impairs adaptation in endurance capacity after aerobic training in previously untrained women. Am. J. Clin. Nutr. 79, 437–443 (2004).
Hinton, P. S. & Sinclair, L. M. Iron supplementation maintains ventilatory threshold and improves energetic efficiency in iron-deficient nonanemic athletes. Eur. J. Clin. Nutr. 61, 30–39 (2007).
Wilson, C. & Brothers, M. Iron deficiency in women and its potential impact on military effectiveness. Nurs. Clin. North Am. 45, 95–108 (2010).
McCann, J. C. & Ames, B. N. An overview of evidence for a causal relation between iron deficiency during development and deficits in cognitive or behavioral function. Am. J. Clin. Nutr. 85, 931–945 (2007).
Kordas, K. Iron, lead, and children's behavior and cognition. Annu. Rev. Nutr. 30, 123–148 (2010).
Verdon, F. et al. Iron supplementation for unexplained fatigue in non-anaemic women: double blind randomised placebo controlled trial. BMJ 326, 1124 (2003).
Patterson, A. J., Brown, W. J., Powers, J. R. & Roberts, D. C. Iron deficiency, general health and fatigue: results from the Australian Longitudinal Study on Women's Health. Qual. Life Res. 9, 491–497 (2000).
Allen, R. P., Barker, P. B., Wehrl, F., Song, H. K. & Earley, C. J. MRI measurement of brain iron in patients with restless legs syndrome. Neurology 56, 263–265 (2001).
Berger, K. et al. Iron metabolism and the risk of restless legs syndrome in an elderly general population—the MEMO-Study. J. Neurol. 249, 1195–1199 (2002).
Sloand, J. A., Shelly, M. A., Feigin, A., Bernstein, P. & Monk, R. D. A double-blind, placebo-controlled trial of intravenous iron dextran therapy in patients with ESRD and restless legs syndrome. Am. J. Kidney Dis. 43, 663–670 (2004).
Ondo, W. G. Intravenous iron dextran for severe refractory restless legs syndrome. Sleep Med. 11, 494–496 (2010).
Martinez-Torres, C. et al. Effect of exposure to low temperature on normal and iron-deficient subjects. Am. J. Physiol. 246, R380–R383 (1984).
Beard, J. L., Borel, M. J. & Derr, J. Impaired thermoregulation and thyroid function in iron-deficiency anemia. Am. J. Clin. Nutr. 52, 813–819 (1990).
Beard, J. L. Iron biology in immune function, muscle metabolism and neuronal functioning. J. Nutr. 131, 568S–579S (2001).
Ahluwalia, N., Sun, J., Krause, D., Mastro, A. & Handte, G. Immune function is impaired in iron-deficient, homebound, older women. Am. J. Clin. Nutr. 79, 516–521 (2004).
Moeinvaziri, M., Mansoori, P., Holakooee, K., Safaee Naraghi, Z. & Abbasi, A. Iron status in diffuse telogen hair loss among women. Acta Dermatovenerol. Croat. 17, 279–284 (2009).
Trost, L. B., Bergfeld, W. F. & Calogeras, E. The diagnosis and treatment of iron deficiency and its potential relationship to hair loss. J. Am. Acad. Dermatol. 54, 824–844 (2006).
Baird, I. M., Dodge, O. G., Palmer, F. J. & Wawman, R. J. The tongue and oesophagus in iron-deficiency anaemia and the effect of iron therapy. J. Clin. Pathol. 14, 603–609 (1961).
Novacek, G. Plummer-Vinson syndrome. Orphanet J. Rare Dis. 1, 36 (2006).
Khan, Y. & Tisman, G. Pica in iron deficiency: a case series. J. Med. Case Reports 4, 86 (2010).
Christian, P. Micronutrients, birth weight, and survival. Annu. Rev. Nutr. 30, 83–104 (2010).
Lizarraga, A. et al. Atrophy of the intestinal villi in a post-gastrectomy patient with severe iron deficiency anemia. Nutr. Hosp. 24, 618–621 (2009).
Author information
Authors and Affiliations
Contributions
J. Stein contributed to the research, discussion, writing and reviewing of the manuscript. F. Hartmann and A. Dignass contributed to the research, discussion and reviewing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Stein, J., Hartmann, F. & Dignass, A. Diagnosis and management of iron deficiency anemia in patients with IBD. Nat Rev Gastroenterol Hepatol 7, 599–610 (2010). https://doi.org/10.1038/nrgastro.2010.151
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2010.151
This article is cited by
-
Microbiota-assisted iron uptake promotes immune tolerance in the intestine
Nature Communications (2023)
-
Iron deficiency and soil-transmitted helminth infection: classic and neglected connections
Parasitology Research (2022)
-
Iron Deficiency in Patients with Inflammatory Bowel Diseases: A Prospective Multicenter Cross-Sectional Study
Digestive Diseases and Sciences (2022)
-
Eisenmangel ohne Anämie
Wiener klinisches Magazin (2021)
-
The burden and management of anemia in Greek patients with inflammatory bowel disease: a retrospective, multicenter, observational study
BMC Gastroenterology (2021)