Key Points
-
Studies published during the past decade have enabled researchers to gain new insights into the diagnosis, physiology and treatment of thyroid disease during pregnancy.
-
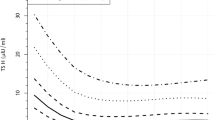
The previously recommended TSH cut-offs of 2.5 mU/l or 3.0 mU/l are too low and are likely to lead to overdiagnosis and overtreatment of thyroid disease during pregnancy.
-
The combination of thyroid peroxidase-antibody positivity and a high concentration of TSH seems to synergistically increase the risk of adverse pregnancy outcomes.
-
Substantial new evidence supports the important role of thyroid hormone for fetal neurodevelopment.
-
New studies indicate that in patients treated with levothyroxine, titration to thyroid hormone concentrations in the higher end of the normal range might carry a risk of overtreatment.
-
Particularly during early pregnancy, treatment with methimazole (thiamazole) or propylthiouracil might increase the risk of fetal anomalies, and clinicians should consider the cessation of low-dose regimens.
Abstract
Adequate thyroid hormone availability is important for an uncomplicated pregnancy and optimal fetal growth and development. Overt thyroid disease is associated with a wide range of adverse obstetric and child development outcomes. An increasing number of studies now indicate that milder forms of thyroid dysfunction are also associated with these adverse pregnancy outcomes. The definitions of both overt and subclinical thyroid dysfunction have changed considerably over the past few years, as new data indicate that the commonly used fixed upper limits of 2.5 mU/l or 3.0 mU/l for thyroid-stimulating hormone (TSH) are too low to define an abnormal thyroid function. Furthermore, some studies now show that the reference ranges are not necessarily the best cut-off for identifying pregnancies at high risk of adverse outcomes. In addition, data suggest that thyroid peroxidase autoantibody positivity and high or low concentrations of human chorionic gonadotropin seem to have a more prominent role in the interpretation of thyroid dysfunction than previously thought. Data on the effects of thyroid disease treatment are lacking, but some studies indicate that clinicians should be aware of the potential for overtreatment with levothyroxine. Here, we put studies from the past decade on reference ranges for TSH, determinants of thyroid dysfunction, risks of adverse outcomes and options for treatment into perspective. In addition, we provide an overview of the current views on thyroid physiology during pregnancy and discuss strategies to identify high-risk individuals who might benefit from levothyroxine treatment.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Krassas, G. E., Poppe, K. & Glinoer, D. Thyroid function and human reproductive health. Endocr. Rev. 31, 702–755 (2010).
Hershman, J. M. The role of human chorionic gonadotropin as a thyroid stimulator in normal pregnancy. J. Clin. Endocrinol. Metab. 93, 3305–3306 (2008).
Medici, M., Korevaar, T. I., Visser, W. E., Visser, T. J. & Peeters, R. P. Thyroid function in pregnancy: what is normal? Clin. Chem. 61, 704–713 (2015).
Pop, V., Broeren, M. & Wiersinga, W. The attitude toward hypothyroidism during early gestation: time for a change of mind? Thyroid 24, 1541–1546 (2014).
Abalovich, M. et al. Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 92, S1–S47 (2007).
Lazarus, J. et al. 2014 European thyroid association guidelines for the management of subclinical hypothyroidism in pregnancy and in children. Eur. Thyroid J. 3, 76–94 (2014).
Lazarus, J. H. et al. Antenatal thyroid screening and childhood cognitive function. N. Engl. J. Med. 366, 493–501 (2012).
Stagnaro-Green, A. et al. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid 21, 1081–1125 (2011).
Blatt, A. J., Nakamoto, J. M. & Kaufman, H. W. National status of testing for hypothyroidism during pregnancy and postpartum. J. Clin. Endocrinol. Metab. 97, 777–784 (2012).
Casey, B. M. et al. Subclinical hyperthyroidism and pregnancy outcomes. Obstet. Gynecol. 107, 337–341 (2006).
Korevaar, T. et al. Stimulation of thyroid function by hCG during pregnancy: a risk factor for thyroid disease and a mechanism for known risk factors. Thyroid 27, 440–450 (2017).
Cooper, D. S. & Laurberg, P. Hyperthyroidism in pregnancy. Lancet Diabetes Endocrinol. 1, 238–249 (2013).
Korevaar, T. I. et al. Association of maternal thyroid function during early pregnancy with offspring IQ and brain morphology in childhood: a population-based prospective cohort study. Lancet Diabetes Endocrinol. 4, 35–43 (2016).
Cooper, D. S. & Rivkees, S. A. Putting propylthiouracil in perspective. J. Clin. Endocrinol. Metab. 94, 1881–1882 (2009).
Laurberg, P. & Andersen, S. L. Antithyroid drug use in pregnancy and birth defects: why some studies find clear associations, and some studies report none. Thyroid 25, 1185–1190 (2015).
Andersen, S. L., Olsen, J., Wu, C. S. & Laurberg, P. Birth defects after early pregnancy use of antithyroid drugs: a Danish nationwide study. J. Clin. Endocrinol. Metab. 98, 4373–4381 (2013).
Takata, K. et al. Methimazole-induced agranulocytosis in patients with Graves' disease is more frequent with an initial dose of 30 mg daily than with 15 mg daily. Thyroid 19, 559–563 (2009).
Taylor, P. N. & Vaidya, B. Side effects of anti-thyroid drugs and their impact on the choice of treatment for thyrotoxicosis in pregnancy. Eur. Thyroid J. 1, 176–185 (2012).
De Groot, L. et al. Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 97, 2543–2565 (2012).
Dashe, J. S. et al. Thyroid-stimulating hormone in singleton and twin pregnancy: importance of gestational age-specific reference ranges. Obstet. Gynecol. 106, 753–757 (2005).
Lambert-Messerlian, G. et al. First- and second-trimester thyroid hormone reference data in pregnant women: a FaSTER (First- and Second-Trimester Evaluation of Risk for aneuploidy) Research Consortium study. Am. J. Obstet. Gynecol. 199, 62e1–62e6 (2008).
Harris, E. K. & Boyd, J. C. Statistical Bases of Reference Values in Laboratory Medicine (Marcel Dekker, 1995).
Geffre, A. et al. Reference values: a review. Vet. Clin. Pathol. 38, 288–298 (2009).
Medici, M. et al. Maternal early pregnancy and newborn thyroid hormone parameters: the Generation R study. J. Clin. Endocrinol. Metab. 97, 646–652 (2012).
Li, C. et al. Assessment of thyroid function during first-trimester pregnancy: what is the rational upper limit of serum TSH during the first trimester in Chinese pregnant women? J. Clin. Endocrinol. Metab. 99, 73–79 (2014).
Alexander, E. K. et al. 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease during Pregnancy and the Postpartum. Thyroid 27, 315–389 (2017).
Anckaert, E. et al. FT4 immunoassays may display a pattern during pregnancy similar to the equilibrium dialysis ID-LC/tandem MS candidate reference measurement procedure in spite of susceptibility towards binding protein alterations. Clin. Chim. Acta 411, 1348–1353 (2010).
Berta, E. et al. Evaluation of the thyroid function of healthy pregnant women by five different hormone assays. Pharmazie 65, 436–439 (2010).
Lee, R. H. et al. Free T4 immunoassays are flawed during pregnancy. Am. J. Obstet. Gynecol. 200, 260e1–260e6 (2009).
Kahric-Janicic, N. et al. Tandem mass spectrometry improves the accuracy of free thyroxine measurements during pregnancy. Thyroid 17, 303–311 (2007).
Christofides, N. D., Wilkinson, E., Stoddart, M., Ray, D. C. & Beckett, G. J. Assessment of serum thyroxine binding capacity-dependent biases in free thyroxine assays. Clin. Chem. 45, 520–525 (1999).
Sapin, R. & d'Herbomez, M. Free thyroxine measured by equilibrium dialysis and nine immunoassays in sera with various serum thyroxine-binding capacities. Clin. Chem. 49, 1531–1535 (2003).
Bliddal, S. et al. Gestational age-specific reference ranges from different laboratories misclassify pregnant women's thyroid status: comparison of two longitudinal prospective cohort studies. Eur. J. Endocrinol. 170, 329–339 (2014).
Glinoer, D. et al. Regulation of maternal thyroid during pregnancy. J. Clin. Endocrinol. Metab. 71, 276–287 (1990).
Korevaar, T. I. et al. Maternal total T4 during the first half of pregnancy: physiologic aspects and the risk of adverse outcomes in comparison with free T4. Clin. Endocrinol. (Oxf.) 85, 757–763 (2016).
Oken, E. et al. Neonatal thyroxine, maternal thyroid function, and child cognition. J. Clin. Endocrinol. Metab. 94, 497–503 (2009).
Zimmermann, M. B. The effects of iodine deficiency in pregnancy and infancy. Paediatr. Perinat Epidemiol. 26 (Suppl. 1), 108–117 (2012).
Shi, X. et al. Optimal and safe upper limits of iodine intake for early pregnancy in iodine-sufficient regions: a cross-sectional study of 7190 pregnant women in China. J. Clin. Endocrinol. Metab. 100, 1630–1638 (2015).
Benhadi, N. et al. Ethnic differences in TSH but not in free T4 concentrations or TPO antibodies during pregnancy. Clin. Endocrinol. (Oxf.) 66, 765–770 (2007).
La'ulu, S. L. & Roberts, W. L. Second-trimester reference intervals for thyroid tests: the role of ethnicity. Clin. Chem. 53, 1658–1664 (2007).
La'ulu, S. L. & Roberts, W. L. Ethnic differences in first-trimester thyroid reference intervals. Clin. Chem. 57, 913–915 (2011).
Walker, J. A., Illions, E. H., Huddleston, J. F. & Smallridge, R. C. Racial comparisons of thyroid function and autoimmunity during pregnancy and the postpartum period. Obstet. Gynecol. 106, 1365–1371 (2005).
Dhatt, G. S. et al. Thyrotrophin and free thyroxine trimester-specific reference intervals in a mixed ethnic pregnant population in the United Arab Emirates. Clin. Chim. Acta 370, 147–151 (2006).
Korevaar, T. I. et al. Hypothyroxinemia and TPO-antibody positivity are risk factors for premature delivery: the generation R study. J. Clin. Endocrinol. Metab. 98, 4382–4390 (2013).
Pop, V. J., Biondi, B., Wijnen, H. A., Kuppens, S. M. & L. Vader, H. Maternal thyroid parameters, body mass index and subsequent weight gain during pregnancy in healthy euthyroid women. Clin. Endocrinol. 79, 577–583 (2013).
Knight, B. A., Shields, B. M., Hattersley, A. T. & Vaidya, B. Maternal hypothyroxinaemia in pregnancy is associated with obesity and adverse maternal metabolic parameters. Eur. J. Endocrinol. 174, 51–57 (2016).
Han, C. et al. High body mass index is an indicator of maternal hypothyroidism, hypothyroxinemia, and thyroid-peroxidase antibody positivity during early pregnancy. Biomed. Res. Int. 2015, 321831 (2015).
Mannisto, T. et al. Early pregnancy reference intervals of thyroid hormone concentrations in a thyroid antibody-negative pregnant population. Thyroid 21, 291–298 (2011).
Laurberg, P., Andersen, S. L., Hindersson, P., Nohr, E. A. & Olsen, J. Dynamics and predictors of serum TSH and fT4 reference limits in early pregnancy: a study within the Danish national birth cohort. J. Clin. Endocrinol. Metab. 101, 2484–2492 (2016).
Mosso, L. et al. Early pregnancy thyroid hormone reference ranges in Chilean women: the influence of body mass index. Clin. Endocrinol. (Oxf.) 85, 942–948 (2016).
Korevaar, T. I. et al. Risk factors and a clinical prediction model for low maternal thyroid function during early pregnancy: two population-based prospective cohort studies. Clin. Endocrinol. (Oxf.) 85, 902–909 (2016).
Haddow, J. E. et al. Variability in thyroid-stimulating hormone suppression by human chorionic [corrected] gonadotropin during early pregnancy. J. Clin. Endocrinol. Metab. 93, 3341–3347 (2008).
Korevaar, T. I. et al. Thyroid autoimmunity impairs the thyroidal response to human chorionic gonadotropin: two population-based prospective cohort studies. J. Clin. Endocrinol. Metab. 102, 69–77 (2017).
Romero, R. et al. A longitudinal study of angiogenic (placental growth factor) and anti-angiogenic (soluble endoglin and soluble vascular endothelial growth factor receptor-1) factors in normal pregnancy and patients destined to develop preeclampsia and deliver a small for gestational age neonate. J. Matern Fetal Neonatal Med. 21, 9–23 (2008).
Kamba, T. et al. VEGF-dependent plasticity of fenestrated capillaries in the normal adult microvasculature. Am. J. Physiol. Heart Circ. Physiol. 290, H560–H576 (2006).
Yang, Y. et al. Anti-VEGF- and anti-VEGF receptor-induced vascular alteration in mouse healthy tissues. Proc. Natl Acad. Sci. USA 110, 12018–12023 (2013).
Korevaar, T. I. et al. Placental angiogenic factors are associated with maternal thyroid function and modify hCG-mediated FT4 stimulation. J. Clin. Endocrinol. Metab. 100, E1328–E2334 (2015).
van den Boogaard, E. et al. Significance of (sub)clinical thyroid dysfunction and thyroid autoimmunity before conception and in early pregnancy: a systematic review. Hum. Reprod. Update 17, 605–619 (2011).
Haddow, J. E. et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N. Engl. J. Med. 341, 549–555 (1999).
de Escobar, G. M., Obregon, M. J. & del Rey, F. E. Role of thyroid hormone during early brain development. Eur. J. Endocrinol. 151, U25–U37 (2004).
Calvo, R., Obregon, M. J., Deona, C. R., Delrey, F. E. & Deescobar, G. M. Congenital hypothyroidism, as studied in rats - crucial role of maternal thyroxine but not of 3,5,3′-Triiodothyronine in the protection of the fetal brain. J. Clin. Invest. 86, 889–899 (1990).
Sheehan, P. M., Nankervis, A., Araujo Junior, E. & Da Silva Costa, F. Maternal thyroid disease and preterm birth: systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 100, 4325–4331 (2015).
Maraka, S. et al. Subclinical hypothyroidism in pregnancy: a systematic review and meta-analysis. Thyroid 26, 580–590 (2016).
Negro, R. & Stagnaro-Green, A. Diagnosis and management of subclinical hypothyroidism in pregnancy. BMJ 349, g4929 (2014).
Henrichs, J. et al. Maternal thyroid function during early pregnancy and cognitive functioning in early childhood: the generation R study. J. Clin. Endocrinol. Metab. 95, 4227–4234 (2010).
Henrichs, J., Ghassabian, A., Peeters, R. P. & Tiemeier, H. Maternal hypothyroxinemia and effects on cognitive functioning in childhood: how and why? Clin. Endocrinol. (Oxf.) 79, 152–162 (2013).
Julvez, J. et al. Thyroxine levels during pregnancy in healthy women and early child neurodevelopment. Epidemiology 24, 150–157 (2013).
Karakosta, P. et al. Thyroid dysfunction and autoantibodies in early pregnancy are associated with increased risk of gestational diabetes and adverse birth outcomes. J. Clin. Endocrinol. Metab. 97, 4464–4472 (2012).
Liu, H. et al. Maternal subclinical hypothyroidism, thyroid autoimmunity, and the risk of miscarriage: a prospective cohort study. Thyroid 24, 1642–1649 (2014).
Ying, H. et al. Maternal TSH level and TPOAb status in early pregnancy and their relationship to the risk of gestational diabetes mellitus. Endocr 54, 742–750 (2016).
Maraka, S. et al. Thyroid hormone treatment among pregnant women with subclinical hypothyroidism: US national assessment. BMJ 356, i6865 (2017).
Thangaratinam, S. et al. Association between thyroid autoantibodies and miscarriage and preterm birth: meta-analysis of evidence. BMJ 342, d2616 (2011).
He, X. et al. Thyroid antibodies and risk of preterm delivery: a meta-analysis of prospective cohort studies. Eur. J. Endocrinol. 167, 455–464 (2012).
Biro, E. et al. Association of systemic and thyroid autoimmune diseases. Clin. Rheumatol 25, 240–245 (2006).
Nakamura, H. et al. Prevalence of interrelated autoantibodies in thyroid diseases and autoimmune disorders. J. Endocrinol. Invest. 31, 861–865 (2008).
Negro, R. et al. Levothyroxine treatment in euthyroid pregnant women with autoimmune thyroid disease: effects on obstetrical complications. J. Clin. Endocrinol. Metab. 91, 2587–2591 (2006).
Nazarpour, S. et al. Effects of levothyroxine treatment on pregnancy outcomes in pregnant women with autoimmune thyroid disease. Eur. J. Endocrinol. 176, 253–265 (2016).
ISRCTNregistry Thyroid AntiBodies and LEvoThyroxine study (TABLET) trial registration. ISRCTNregistry http://www.isrctn.com/ISRCTN15948785 (2017).
Nederlands Trialregister T4LIFE trial registration. Trialregister http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=3364 (2017).
Berbel, P. et al. Delayed neurobehavioral development in children born to pregnant women with mild hypothyroxinemia during the first month of gestation: the importance of early iodine supplementation. Thyroid 19, 511–519 (2009).
Pop, V. J. & Vulsma, T. Maternal hypothyroxinaemia during (early) gestation. Lancet 365, 1604–1606 (2005).
Zimmermann, M. B. The adverse effects of mild-to-moderate iodine deficiency during pregnancy and childhood: a review. Thyroid 17, 829–835 (2007).
Zimmermann, M. B. & Boelaert, K. Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 3, 286–295 (2015).
Pedersen, K. M. et al. Amelioration of some pregnancy-associated variations in thyroid function by iodine supplementation. J. Clin. Endocrinol. Metab. 77, 1078–1083 (1993).
Negro, R., Soldin, O. P., Obregon, M. J. & Stagnaro-Green, A. Hypothyroxinemia and pregnancy. Endocr. Pract. 17, 422–429 (2011).
Yu, X. et al. Iron deficiency, an independent risk factor for isolated hypothyroxinemia in pregnant and nonpregnant women of childbearing age in China. J. Clin. Endocrinol. Metab. 100, 1594–1601 (2015).
Medici, M. et al. Maternal thyroid hormone parameters during early pregnancy and birth weight: the Generation R Study. J. Clin. Endocrinol. Metab. 98, 59–66 (2013).
Ghassabian, A. et al. Downstream effects of maternal hypothyroxinemia in early pregnancy: nonverbal IQ and brain morphology in school-age children. J. Clin. Endocrinol. Metab. 99, 2383–2390 (2014).
Roman, G. C. et al. Association of gestational maternal hypothyroxinemia and increased autism risk. Ann. Neurol. 74, 733–742 (2013).
Gyllenberg, D. et al. Hypothyroxinemia during gestation and offspring schizophrenia in a national birth cohort. Biol. Psychiatry 79, 962–970 (2016).
Finken, M. J., van Eijsden, M., Loomans, E. M., Vrijkotte, T. G. & Rotteveel, J. Maternal hypothyroxinemia in early pregnancy predicts reduced performance in reaction time tests in 5- to 6-year-old offspring. J. Clin. Endocrinol. Metab. 98, 1417–1426 (2013).
Modesto, T. et al. Maternal mild thyroid hormone insufficiency in early pregnancy and attention-deficit/Hyperactivity disorder symptoms in children. JAMA Pediatr. 169, 838–845 (2015).
Pakkila, F. et al. Maternal and child's thyroid function and child's intellect and scholastic performance. Thyroid 25, 1363–1374 (2015).
European Thyroid Association Abstracts: Hales, C. et al. (p59) and Taylor, P. et al. (p128) Eur. Thyroid J. 5 (Suppl. 1), 57–176 (2016).
Hales, C. et al. The second wave of the Controlled Antenatal Thyroid Screening (CATS II) study: the cognitive assessment protocol. BMC Endocr. Disord. 14, 95 (2014).
Casey, B. M. et al. Treatment of subclinical hypothyroidism or hypothyroxinemia in pregnancy. N. Engl. J. Med. 376, 815–825 (2017).
ClinicalTrials Thyroid therapy for mild thyroid deficiency in pregnancy (TSH). ClinicalTrials https://clinicaltrials.gov/ct2/show/NCT00388297 (2017).
Attina, T. M. et al. Exposure to endocrine-disrupting chemicals in the USA: a population-based disease burden and cost analysis. Lancet Diabetes Endocrinol. 4, 996–1003 (2016).
Power, C., Kuh, D. & Morton, S. From developmental origins of adult disease to life course research on adult disease and aging: insights from birth cohort studies. Annu. Rev. Publ. Health 34, 7–28 (2013).
Casey, B. M. et al. Perinatal significance of isolated maternal hypothyroxinemia identified in the first half of pregnancy. Obstet. Gynecol. 109, 1129–1135 (2007).
Mannisto, T. et al. Thyroid dysfunction and autoantibodies during pregnancy as predictive factors of pregnancy complications and maternal morbidity in later life. J. Clin. Endocrinol. Metab. 95, 1084–1094 (2010).
Haddow, J. E. et al. Implications of High Free Thyroxine (FT4) concentrations in euthyroid pregnancies: the FaSTER trial. J. Clin. Endocrinol. Metab. 99, 2038–2044 (2014).
Pakkila, F. et al. The impact of gestational thyroid hormone concentrations on ADHD symptoms of the child. J. Clin. Endocrinol. Metab. 99, E1–E8 (2014).
Dosiou, C. & Medici, M. Isolated maternal hypothyroxinemia during pregnancy: knowns and unknowns. Eur. J. Endocrinol. 176, R21–R38 (2016).
Medici, M. et al. Maternal early-pregnancy thyroid function is associated with subsequent hypertensive disorders of pregnancy: the generation R study. J. Clin. Endocrinol. Metab. 99, E2591–2598 (2014).
Tudela, C. M., Casey, B. M., McIntire, D. D. & Cunningham, F. G. Relationship of subclinical thyroid disease to the incidence of gestational diabetes. Obstet. Gynecol. 119, 983–988 (2012).
Tong, Z. et al. The effect of subclinical maternal thyroid dysfunction and autoimmunity on intrauterine growth restriction: a systematic review and meta-analysis. Med. (Baltimore) 95, e3677 (2016).
Carle, A. et al. Epidemiology of subtypes of hyperthyroidism in Denmark: a population-based study. Eur. J. Endocrinol. 164, 801–809 (2011).
Springer, D., Zima, T. & Limanova, Z. Reference intervals in evaluation of maternal thyroid function during the first trimester of pregnancy. Eur. J. Endocrinol. 160, 791–797 (2009).
Sheffield, J. S. & Cunningham, F. G. Thyrotoxicosis and heart failure that complicate pregnancy. Am. J. Obstet. Gynecol. 190, 211–217 (2004).
Sahu, M. T., Das, V., Mittal, S., Agarwal, A. & Sahu, M. Overt and subclinical thyroid dysfunction among Indian pregnant women and its effect on maternal and fetal outcome. Arch. Gynecol. Obstet. 281, 215–220 (2010).
Luewan, S., Chakkabut, P. & Tongsong, T. Outcomes of pregnancy complicated with hyperthyroidism: a cohort study. Arch. Gynecol. Obstet. 283, 243–247 (2011).
Millar, L. K. et al. Low birth weight and preeclampsia in pregnancies complicated by hyperthyroidism. Obstet. Gynecol. 84, 946–949 (1994).
Davis, L. E., Lucas, M. J., Hankins, G. D., Roark, M. L. & Cunningham, F. G. Thyrotoxicosis complicating pregnancy. Am. J. Obstet. Gynecol. 160, 63–70 (1989).
Pillar, N., Levy, A., Holcberg, G. & Sheiner, E. Pregnancy and perinatal outcome in women with hyperthyroidism. Int. J. Gynaecol. Obstet. 108, 61–64 (2010).
Aggarawal, N. et al. Pregnancy outcome in hyperthyroidism: a case control study. Gynecol. Obstet. Invest. 77, 94–99 (2014).
Mannisto, T. et al. Thyroid diseases and adverse pregnancy outcomes in a contemporary US cohort. J. Clin. Endocrinol. Metab. 98, 2725–2733 (2013).
Andersen, S. L., Laurberg, P., Wu, C. S. & Olsen, J. Attention deficit hyperactivity disorder and autism spectrum disorder in children born to mothers with thyroid dysfunction: a Danish nationwide cohort study. BJOG 121, 1365–1374 (2014).
Andersen, S. L., Olsen, J., Wu, C. S. & Laurberg, P. Low birth weight in children born to mothers with hyperthyroidism and high birth weight in hypothyroidism, whereas preterm birth is common in both conditions: A danish national hospital register study. Eur. Thyroid J. 2, 135–144 (2013).
Andersen, S. L., Olsen, J., Wu, C. S. & Laurberg, P. Spontaneous abortion, stillbirth and hyperthyroidism: a danish population-based study. Eur. Thyroid J. 3, 164–172 (2014).
Laurberg, P. et al. TSH-receptor autoimmunity in Graves' disease after therapy with anti-thyroid drugs, surgery, or radioiodine: a 5-year prospective randomized study. Eur. J. Endocrinol. 158, 69–75 (2008).
Zakarija, M. & McKenzie, J. M. Pregnancy-associated changes in the thyroid-stimulating antibody of Graves' disease and the relationship to neonatal hyperthyroidism. J. Clin. Endocrinol. Metab. 57, 1036–1040 (1983).
Barbesino, G. & Tomer, Y. Clinical review: Clinical utility of TSH receptor antibodies. J. Clin. Endocrinol. Metab. 98, 2247–2255 (2013).
Yoshihara, A. et al. Substituting potassium iodide for methimazole as the treatment for graves' disease during the first trimester may reduce the incidence of congenital anomalies: a retrospective study at a single medical institution in Japan. Thyroid 25, 1155–1161 (2015).
Nedrebo, B. G. et al. Predictors of outcome and comparison of different drug regimens for the prevention of relapse in patients with Graves' disease. Eur. J. Endocrinol. 147, 583–589 (2002).
Momotani, N., Noh, J., Oyanagi, H., Ishikawa, N. & Ito, K. Antithyroid drug therapy for Graves' disease during pregnancy. Optimal regimen for fetal thyroid status. N. Engl. J. Med. 315, 24–28 (1986).
Korevaar, T. I. et al. Maternal and birth characteristics are determinants of offspring thyroid function. J. Clin. Endocrinol. Metab. 101, 206–213 (2016).
Korevaar, T. I. et al. The risk of pre-eclampsia according to high thyroid function in pregnancy differs by hCG concentration. J. Clin. Endocrinol. Metab. 101, 5037–5043 (2016).
Ashoor, G., Maiz, N., Rotas, M., Kametas, N. A. & Nicolaides, K. H. Maternal thyroid function at 11 to 13 weeks of gestation and subsequent development of preeclampsia. Prenat Diagn. 30, 1032–1038 (2010).
Wilson, K. L., Casey, B. M., McIntire, D. D., Halvorson, L. M. & Cunningham, F. G. Subclinical thyroid disease and the incidence of hypertension in pregnancy. Obstet. Gynecol. 119, 315–320 (2012).
Korevaar, T. I., Taylor, P. N., Dayan, C. M. & Peeters, R. P. An invitation to join the consortium on thyroid and pregnancy. Obstet. Gynecol. 128, 913 (2016).
Acknowledgements
The authors' research work was supported by a clinical fellowship from The Netherlands Organisation for Health Research and Development (ZonMw), project number 90700412 to R.P. Peeters.
Author information
Authors and Affiliations
Contributions
T.I.M.K. and R.P.P. wrote the first draft of the manuscript, after which all authors contributed equally to researching the data for the article, discussion of content, writing the article and reviewing and/or editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
T.I.M.K. has received lecture fees from Berlin-Chemie, Goodlife Healthcare and Excemed. R.P.P. has received lecture fees from Goodlife Healthcare. The other authors declare no competing interests.
Supplementary information
Supplementary information S1 (table)
Reference ranges for TSH and FT4 during early pregnancy worldwide. (PDF 148 kb)
Glossary
- Subclinical hypothyroidism
-
Defined as a high TSH concentration (>97.5th percentile) with a normal free T4 concentration (2.5th to 97.5th percentiles).
- Hypothyroxinaemia
-
Defined as a normal TSH concentration (2.5th to 97.5th percentiles) with a low free T4 (<2.5th percentile; but in some cases <5th percentile).
- Mental score
-
Determined by the outcome of standardized neurodevelopment tests, such as the WISC, and is a reflection of child IQ.
- Psychomotor score
-
The outcome of standardized neurodevelopment tests, such as the WISC, and reflects the psychomotor development of the child, including the child's achievement of developmental milestones.
Rights and permissions
About this article
Cite this article
Korevaar, T., Medici, M., Visser, T. et al. Thyroid disease in pregnancy: new insights in diagnosis and clinical management. Nat Rev Endocrinol 13, 610–622 (2017). https://doi.org/10.1038/nrendo.2017.93
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrendo.2017.93
This article is cited by
-
Effects of altitude on thyroid disorders according to Chinese three-rung, ladder-like topography: national cross-sectional study
BMC Public Health (2024)
-
Mediation by Thyroid Hormone in the Relationships Between Gestational Exposure to Methylmercury and Birth Size
Exposure and Health (2024)
-
Verhoog de levothyroxinedosering bij zwangeren met hypothyreoïdie
Huisarts en wetenschap (2024)
-
EndoBridge 2023: highlights and pearls
Hormones (2024)
-
Maternal preconception thyroid autoimmunity is associated with neonatal birth weight conceived by PCOS women undergoing their first in vitro fertilization/intracytoplasmic sperm injection
Journal of Ovarian Research (2023)