Abstract
Endocrine glands are among the organs that most frequently harbor incidentally discovered lesions. Pituitary, thyroid, parathyroid and adrenal incidentalomas are increasingly encountered in everyday practice with variable clinical implications. The major concerns are the risks of malignancy and hormonal hypersecretion mostly in the form of subclinically functioning tumors. Pituitary incidentalomas are usually microadenomas and most of the time clinically unimportant; however, incidentally discovered larger lesions require a more careful diagnostic and therapeutic approach. Thyroid incidentalomas are extremely common; exclusion of malignancy is the main concern in this clinical setting. Although parathyroid adenomas are not uncommon, these lesions are frequently missed owing to their small size and due to clinical unawareness. Adrenal incidentalomas carry a small but finite risk of malignancy. An intriguing challenge regarding incidentally discovered adrenal lesions is that a substantial proportion is associated with hormonal alterations, mainly in the form of subtle cortisol excess. Although still largely controversial, evidence is emerging that so-called subclinical hypercortisolism may not be completely harmless. The best biochemical criterion of subtle cortisol excess remains elusive. Surgical intervention in selected cases results in some beneficial effects, but more data are required in order to routinely support surgery in this clinical setting. This Review provides a brief overview of the prevalence, clinical effect and management of endocrine incidentalomas with a focus on data regarding the diagnostic and therapeutic challenges imposed by incidentally discovered adrenal lesions.
Key Points
-
Most pituitary microincidentalomas are clinically unimportant, whereas macroincidentalomas require a more cautious approach
-
Thyroid incidentalomas carry a substantial risk of malignancy; fine-needle aspiration is the procedure of choice for the management of a substantial number of these patients
-
Parathyroid incidentalomas are not frequently seen
-
In patients with adrenal incidentalomas, hormonal assessment for exclusion of cortisol, aldosterone and catecholamine excess is mandatory
-
Subtle autonomous cortisol secretion is the most common abnormality, and increasing evidence shows that subclinical hypercortisolism is not completely harmless
-
Although surgical removal of cortisol-secreting, incidentally detected adrenal lesions may have some beneficial effects, more studies are required in order to routinely recommend surgery in this clinical setting
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Black, W. C. & Welch, H. G. Advances in diagnostic imaging and overestimations of disease prevalence and the benefits of therapy. N. Engl. J. Med. 328, 1237–1243 (1993).
Bailey, R. H. & Aron, D. C. The diagnostic dilemma of incidentalomas. Working through uncertainty. Endocrinol. Metab. Clin. North Am. 29, 91–105 (2000).
Chidiac, R. M. & Aron, D. C. Incidentalomas. A disease of modern technology. Endocrinol. Metab. Clin. North Am. 26, 233–253 (1997).
Turner, H. E., Moore, N. R., Byrne, J. V. & Wass, J. A. H. Pituitary, adrenal and thyroid incidentalomas. Endocr. Relat. Cancer 5, 131–150 (1998).
Aron, D. C. & Howlett, T. A. Pituitary incidentalomas. Endocrinol. Metab. Clin. North Am. 29, 205–221 (2000).
Koenig, K. & Kleerekoper, M. How common are functional incidentalomas of the parathyroid gland? Nat. Clin. Pract. Endocrinol. Metab. 2, 316–317 (2006).
Griffing, G. T. A-I-D-S: the new endocrine epidemic. J. Clin. Endocrinol. Metab. 79, 1530–1531 (1994).
Dean, D. S. & Gharib, H. Epidemiology of thyroid nodules. Best Pract. Res. Clin. Endocrinol. Metab. 22, 901–911 (2008).
Ezzat, S. et al. The prevalence of pituitary adenomas: a systematic review. Cancer 101, 613–619 (2004).
Ezzat, S., Sarti, D. A., Cain, D. R. & Braunstein, G. D. Thyroid incidentalomas. Prevalence by palpation and ultrasonography. Arch. Intern. Med. 154, 1838–1840 (1994).
Young, W. F. Jr. Management approaches to adrenal incidentalomas. A view from Rochester, Minnesota. Endocrinol. Metab. Clin. North Am. 29, 159–185 (2000).
Molitch, M. E. Pituitary tumours: pituitary incidentalomas. Best Pract. Res. Clin. Endocrinol. Metab. 23, 667–675 (2009).
Chambers, E. F., Turski, P. A., LaMasters, D. & Newton, T. H. Regions of low density in the contrast-enhanced pituitary gland: normal and pathologic processes. Radiology 144, 109–113 (1982).
Krikorian, A. & Aron, D. Evaluation and management of pituitary incidentalomas—revisiting an acquaintance. Nat. Clin. Pract. Endocrinol. Metab. 2, 138–145 (2006).
Connor, S. E. & Penney, C. C. MRI in the differential diagnosis of a sellar mass. Clin. Radiol. 58, 20–31 (2003).
Nammour, G. M., Ybarra, J., Naheedy, M. H., Romeo, J. H. & Aron, D. C. Incidental pituitary macroadenoma: a population-based study. Am. J. Med. Sci. 314, 287–291 (1997).
Yue, N. C. et al. Clinically serious abnormalities found incidentally at MR imaging of the brain: data from the Cardiovascular Health Study. Radiology 202, 41–46 (1997).
Chacko, A. G. & Chandy, M. J. Incidental pituitary macroadenomas. Br. J. Neurosurg. 6, 233–236 (1992).
Buurman, H. & Saeger, W. Subclinical adenomas in postmortem pituitaries: classification and correlations to clinical data. Eur. J. Endocrinol. 154, 753–758 (2006).
Kontogeorgos, G., Kovacs, K., Horvath, E. & Scheithauer, B. W. Multiple adenomas of the human pituitary. A retrospective autopsy study with clinical implications. J. Neurosurg. 74, 243–247 (1991).
Chong, B. W., Kucharczyk, W., Singer, W. & George, S. Pituitary gland MR: a comparative study of healthy volunteers and patients with microadenomas. AJNR Am. J. Neuroradiol. 15, 675–679 (1994).
Hall, W. A., Luciano, M. G., Doppman, J. L., Patronas, N. J. & Oldfield, E. H. Pituitary magnetic resonance imaging in normal human volunteers: occult adenomas in the general population. Ann. Intern. Med. 120, 817–820 (1994).
Jeong, S. Y. et al. Incidental pituitary uptake on whole-body 18F-FDG PET/CT: a multicentre study. Eur. J. Nucl. Med. Mol. Imaging 37, 2334–2343 (2010).
Molitch, M. E. Clinical review 65. Evaluation and treatment of the patient with a pituitary incidentaloma. J. Clin. Endocrinol. Metab. 80, 3–6 (1995).
Feldkamp, J. et al. Incidentally discovered pituitary lesions: high frequency of macroadenomas and hormone-secreting adenomas—results of a prospective study. Clin. Endocrinol. (Oxf.) 51, 109–113 (1999).
Oyama, K., Sanno, N., Tahara, S. & Teramoto, A. Management of pituitary incidentalomas: according to a survey of pituitary incidentalomas in Japan. Semin. Ultrasound CT MR 26, 47–50 (2005).
Daems, T. et al. Modification of hormonal secretion in clinically silent pituitary adenomas. Pituitary 12, 80–86 (2009).
Fainstein Day, P. et al. Retrospective multicentric study of pituitary incidentalomas. Pituitary 7, 145–148 (2004).
Reincke, M., Allolio, B., Saeger, W., Menzel, J. & Winkelmann, W. The 'incidentaloma' of the pituitary gland. Is neurosurgery required? JAMA 263, 2772–2776 (1990).
King, J. T. Jr, Justice, A. C. & Aron, D. C. Management of incidental pituitary microadenomas: a cost-effectiveness analysis. J. Clin. Endocrinol. Metab. 82, 3625–3632 (1997).
Donovan, L. E. & Corenblum, B. The natural history of the pituitary incidentaloma. Arch. Intern. Med. 155, 181–183 (1995).
Yuen, K. C. et al. Prevalence of GH and other anterior pituitary hormone deficiencies in adults with nonsecreting pituitary microadenomas and normal serum IGF-1 levels. Clin. Endocrinol. (Oxf.) 69, 292–298 (2008).
Arita, K. et al. Natural course of incidentally found nonfunctioning pituitary adenoma, with special reference to pituitary apoplexy during follow-up examination. J. Neurosurg. 104, 884–891 (2006).
Karavitaki, N. et al. What is the natural history of nonoperated nonfunctioning pituitary adenomas? Clin. Endocrinol. (Oxf.) 67, 938–943 (2007).
Dekkers, O. M. et al. The natural course of non-functioning pituitary macroadenomas. Eur. J. Endocrinol. 156, 217–224 (2007).
Kay, J. & Czirják, L. Gadolinium and systemic fibrosis: guilt by association. Ann. Rheum. Dis. 69, 1895–1897 (2010).
Molitch, M. E. Nonfunctioning pituitary tumors and pituitary incidentalomas. Endocrinol. Metab. Clin. North. Am. 37, 151–171, xi (2008).
Tomimori, E., Pedrinola, F., Cavaliere, H., Knobel, M. & Medeiros-Neto, G. Prevalence of incidental thyroid disease in a relatively low iodine intake area. Thyroid 5, 273–276 (1995).
Mortensen, J. D., Woolner, L. B. & Bennett, W. A. Gross and microscopic findings in clinically normal thyroid glands. J. Clin. Endocrinol. Metab. 15, 1270–1280 (1955).
Wang, C. & Crapo, L. M. The epidemiology of thyroid disease and implications for screening. Endocrinol. Metab. Clin. North Am. 26, 189–218 (1997).
Reiners, C. et al. Prevalence of thyroid disorders in the working population of Germany: ultrasonography screening in 96,278 unselected employees. Thyroid 14, 926–932 (2004).
Chu, Q. D. et al. Positron emission tomography (PET) positive thyroid incidentaloma: the risk of malignancy observed in a tertiary referral center. Am. Surg. 72, 272–275 (2006).
Are, C. et al. FDG-PET detected thyroid incidentalomas: need for further investigation? Ann. Surg. Oncol. 14, 239–247 (2007).
Kang, K. W. et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for metastasis evaluation and cancer screening in healthy subjects. J. Clin. Endocrinol. Metab. 88, 4100–4104 (2003).
Minamimoto, R. et al. Performance profile of FDG-PET and PET/CT for cancer screening on the basis of a Japanese Nationwide Survey. Ann. Nucl. Med. 21, 481–498 (2007).
Van den Bruel, A. et al. Clinical relevance of thyroid fluorodeoxyglucose-whole body positron emission tomography incidentaloma. J. Clin. Endocrinol. Metab. 87, 1517–1520 (2002).
Kim, T. Y. et al. 18F-fluorodeoxyglucose uptake in thyroid from positron emission tomogram (PET) for evaluation in cancer patients: high prevalence of malignancy in thyroid PET incidentaloma. Laryngoscope 115, 1074–1078 (2005).
Gharib, H. & Papini, E. Thyroid nodules: clinical importance, assessment, and treatment. Endocrinol. Metab. Clin. North Am. 36, 707–735 (2007).
Kang, H. W. et al. Prevalence, clinical and ultrasonographic characteristics of thyroid incidentalomas. Thyroid 14, 29–33 (2004).
Davies, L. & Welch, H. G. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295, 2164–2167 (2006).
Bernet, V. Approach to the patient with incidental papillary microcarcinoma. J. Clin. Endocrinol. Metab. 95, 3586–3592 (2010).
Hay, I. D. et al. Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery 144, 980–987 (2008).
Gharib, H. et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. Endocr. Pract. 16 (Suppl. 1), 1–43 (2010).
Cosgrove, D. Future prospects for SonoVue and CPS. Eur. Radiol. 14 (Suppl. 8), P116–P124 (2004).
Asteria, C. et al. US-elastography in the differential diagnosis of benign and malignant thyroid nodules. Thyroid 18, 523–531 (2008).
Cooper, D. S. et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19, 1167–1214 (2009).
Kim, S. W. et al. BRAFV600E mutation analysis in fine-needle aspiration cytology specimens for evaluation of thyroid nodule: a large series in a BRAFV600E-prevalent population. J. Clin. Endocrinol. Metab. 95, 3693–3700 (2010).
Boelaert, K. The association between serum TSH concentration and thyroid cancer. Endocr. Relat. Cancer 16, 1065–1072 (2009).
Boelaert, K. et al. Serum thyrotropin concentration as a novel predictor of malignancy in thyroid nodules investigated by fine-needle aspiration. J. Clin. Endocrinol. Metab. 91, 4295–4301 (2006).
Fiore, E. et al. Lower levels of TSH are associated with a lower risk of papillary thyroid cancer in patients with thyroid nodular disease: thyroid autonomy may play a protective role. Endocr. Relat. Cancer 16, 1251–1260 (2009).
Valle, L. A. & Kloos, R. T. The prevalence of occult medullary thyroid carcinoma at autopsy. J. Clin. Endocrinol. Metab. 96, E109–E113 (2011).
Wilhelm, S. M., Robinson, A. V., Krishnamurthi, S. S. & Reynolds, H. L. Evaluation and management of incidental thyroid nodules in patients with another primary malignancy. Surgery 142, 581–586 (2007).
Ohba, K. et al. High incidence of thyroid cancer in focal thyroid incidentaloma detected by 18F-fluorodexyglucose positron emission tomography in relatively young healthy subjects: results of 3-year follow-up. Endocr. J. 57, 395–401 (2010).
Shroff, P., McGrath, G. A. & Pezzi, C. M. Incidentalomas of the parathyroid gland: multiple presentations, variable function, and review of the literature. Endocr. Pract. 11, 363–369 (2005).
Katz, A. D. & Kong, L. B. Incidental preclinical hyperparathyroidism identified during thyroid operations. Am. Surg. 58, 747–749 (1992).
Kwak, J. Y. et al. Parathyroid incidentalomas detected on routine ultrasound-directed fine-needle aspiration biopsy in patients referred for thyroid nodules and the role of parathyroid hormone analysis in the samples. Thyroid 19, 743–748 (2009).
Akerström, G. et al. Histologic parathyroid abnormalities in an autopsy series. Hum. Pathol. 17, 520–527 (1986).
Yu, N., Donnan, P. T. & Leese, G. P. A record linkage study of outcomes in patients with mild primary hyperparathyroidism: The Parathyroid Epidemiology and Audit Research Study (PEARS). Clin. Endocrinol. (Oxf.) doi:10.1111/j.1365–2265.2010.03958.x.
Bilezikian, J. P., Khan, A. A. & Potts, J. T. Jr. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J. Clin. Endocrinol. Metab. 94, 335–339 (2009).
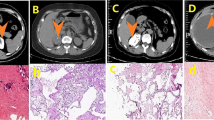
Barzon, L., Sonino, N., Fallo, F., Palu, G. & Boscaro, M. Prevalence and natural history of adrenal incidentalomas. Eur. J. Endocrinol. 149, 273–285 (2003).
Kloos, R. T., Gross, M. D., Francis, I. R., Korobkin, M. & Shapiro, B. Incidentally discovered adrenal masses. Endocr. Rev. 16, 460–484 (1995).
Spain, D. M. & Weinsaft, P. Solitary adrenal cortical adenoma in elderly female; frequency. Arch. Pathol. 78, 231–233 (1964).
Dévényi, I. Possibility of normokalaemic primary aldosteronism as reflected in the frequency of adrenal cortical adenomas. J. Clin. Pathol. 20, 49–51 (1967).
Dobbie, J. W. Adrenocortical nodular hyperplasia: the ageing adrenal. J. Pathol. 99, 1–18 (1969).
Bovio, S. et al. Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J. Endocrinol. Invest. 29, 298–302 (2006).
Bülow, B. et al. Adrenal incidentaloma—follow-up results from a Swedish prospective study. Eur. J. Endocrinol. 154, 419–423 (2006).
Kasperlik-Zeluska, A. A. et al. Incidentally discovered adrenal mass (incidentaloma): investigation and management of 208 patients. Clin. Endocrinol. (Oxf.) 46, 29–37 (1997).
Barzon, L. et al. Incidentally discovered adrenal tumors: endocrine and scintigraphic correlates. J. Clin. Endocrinol. Metab. 83, 55–62 (1998).
Caplan, R. H., Strutt, P. J. & Wickus, G. G. Subclinical hormone secretion by incidentally discovered adrenal masses. Arch. Surg. 129, 291–296 (1994).
Herrera, M. F., Grant, C. S., van Heerden, J. A., Sheedy, P. F. & Ilstrup, D. M. Incidentally discovered adrenal tumors: an institutional perspective. Surgery 110, 1014–1021 (1991).
Cawood, T. J., Hunt, P. J., O'Shea, D., Cole, D. & Soule, S. Recommended evaluation of adrenal incidentalomas is costly, has high false-positive rates and confers a risk of fatal cancer that is similar to the risk of the adrenal lesion becoming malignant; time for a rethink? Eur. J. Endocrinol. 161, 513–527 (2009).
Buurman, H. & Saeger, W. Abnormalities in incidentally removed adrenal glands. Endocr. Pathol. 17, 277–282 (2006).
Funder, J. W. et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 93, 3266–3281 (2008).
Mantero, F. et al. A survey on adrenal incidentaloma in Italy. Study Group on Adrenal Tumors of the Italian Society of Endocrinology. J. Clin. Endocrinol. Metab. 85, 637–644 (2000).
Bernini, G. P. et al. Frequency of pheochromocytoma in adrenal incidentalomas and utility of the glucagon test for the diagnosis. J. Endocrinol. Invest. 20, 65–71 (1997).
Tsagarakis, S., Vassiliadi, D. & Thalassinos, N. Endogenous subclinical hypercortisolism: Diagnostic uncertainties and clinical implications. J. Endocrinol. Invest. 29, 471–482 (2006).
Vassilatou, E. et al. Hormonal activity of adrenal incidentalomas: results from a long-term follow-up study. Clin. Endocrinol. (Oxf.) 70, 674–679 (2009).
Nieman, L. K. Approach to the patient with an adrenal incidentaloma. J. Clin. Endocrinol. Metab. 95, 4106–4113 (2010).
Pantalone, K. M. et al. Change in adrenal mass size as a predictor of a malignant tumor. Endocr. Pract. 16, 577–587 (2010).
Johnson, P. T., Horton, K. M. & Fishman, E. K. Adrenal mass imaging with multidetector CT: pathologic conditions, pearls, and pitfalls. Radiographics 29, 1333–1351 (2009).
Ilias, I., Sahdev, A., Reznek, R. H., Grossman, A. B. & Pacak, K. The optimal imaging of adrenal tumours: a comparison of different methods. Endocr. Relat. Cancer 14, 587–599 (2007).
Yun, M. et al. 18F-FDG PET in characterizing adrenal lesions detected on CT or MRI. J. Nucl. Med. 42, 1795–1799 (2001).
Kopetschke, R. et al. Frequent incidental discovery of phaeochromocytoma: data from a German cohort of 201 phaeochromocytoma. Eur. J. Endocrinol. 161, 355–361 (2009).
Pacak, K. et al. Pheochromocytoma: recommendations for clinical practice from the First International Symposium. October 2005. Nat. Clin. Pract. Endocrinol. Metab. 3, 92–102 (2007).
Vierhapper, H. Determination of the aldosterone/renin ratio in 269 patients with adrenal incidentaloma. Exp. Clin. Endocrinol. Diabetes 115, 518–521 (2007).
Nieman, L. K. et al. The diagnosis of Cushing's syndrome: an Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 93, 1526–1540 (2008).
Tsagarakis, S. et al. Elevated post-dexamethasone suppression cortisol concentrations correlate with hormonal alterations of the hypothalamo-pituitary adrenal axis in patients with adrenal incidentalomas. Clin. Endocrinol. (Oxf.) 49, 165–171 (1998).
Terzolo, M. et al. Midnight serum cortisol as a marker of increased cardiovascular risk in patients with a clinically inapparent adrenal adenoma. Eur. J. Endocrinol. 153, 307–315 (2005).
Fernández-Real, J. M., Engel, W. R., Simó, R., Salinas, I. & Webb, S. M. Study of glucose tolerance in consecutive patients harbouring incidental adrenal tumours. Study Group of Incidental Adrenal Adenoma. Clin. Endocrinol. (Oxf.) 49, 53–61 (1998).
Young, W. F. Jr. Clinical practice. The incidentally discovered adrenal mass. N. Engl. J. Med. 356, 601–610 (2007).
Zeiger, M. A. et al. American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons Medical Guidelines for the Management of Adrenal Incidentalomas: executive summary of recommendations. Endocr. Pract. 15, 450–453 (2009).
Nunes, M. L. et al. Late-night salivary cortisol for diagnosis of overt and subclinical Cushing's syndrome in hospitalized and ambulatory patients. J. Clin. Endocrinol. Metab. 94, 456–462 (2009).
Fagour, C. et al. Usefulness of adrenal scintigraphy in the follow-up of adrenocortical incidentalomas: a prospective multicenter study. Eur. J. Endocrinol. 160, 257–264 (2009).
Bardet, S. et al. 131I-6 beta-iodomethylnorcholesterol scintigraphy: an assessment of its role in the investigation of adrenocortical incidentalomas. Clin. Endocrinol. (Oxf.) 44, 587–596 (1996).
Radiation dose to patients from radiopharmaceuticals (addendum 2 to ICRP publication 53). Ann. ICRP 28, 1–126 (1998).
Chiodini, I. et al. Beneficial metabolic effects of prompt surgical treatment in patients with an adrenal incidentaloma causing biochemical hypercortisolism. J. Clin. Endocrinol. Metab. 95, 2736–2745 (2010).
Stewart, P. M. Is subclinical Cushing's syndrome an entity or a statistical fallout from diagnostic testing? Consensus surrounding the diagnosis is required before optimal treatment can be defined. J. Clin. Endocrinol. Metab. 95, 2618–2620 (2010).
Rossi, R. et al. Subclinical Cushing's syndrome in patients with adrenal incidentaloma: clinical and biochemical features. J. Clin. Endocrinol. Metab. 85, 1440–1448 (2000).
Tauchmanovà, L. et al. Patients with subclinical Cushing's syndrome due to adrenal adenoma have increased cardiovascular risk. J. Clin. Endocrinol. Metab. 87, 4872–4878 (2002).
Bernini, G. et al. Anthropometric, haemodynamic, humoral and hormonal evaluation in patients with incidental adrenocortical adenomas before and after surgery. Eur. J. Endocrinol. 148, 213–219 (2003).
Toniato, A. et al. Surgical versus conservative management for subclinical Cushing syndrome in adrenal incidentalomas: a prospective randomized study. Ann. Surg. 249, 388–391 (2009).
Tsuiki, M., Tanabe, A., Takagi, S., Naruse, M. & Takano, K. Cardiovascular risks and their long-term clinical outcome in patients with subclinical Cushing's syndrome. Endocr. J. 55, 737–745 (2008).
Eller-Vainicher, C. et al. Post-surgical hypocortisolism after removal of an adrenal incidentaloma: is it predictable by an accurate endocrinological work-up before surgery? Eur. J. Endocrinol. 162, 91–99 (2010).
Kasperlik-Zaluska, A. A. et al. Incidentally discovered adrenal tumors: a lesson from observation of 1,444 patients. Horm. Metab. Res. 40, 338–341 (2008).
Reincke, M. et al. Preclinical Cushing's syndrome in adrenal “incidentalomas”: comparison with adrenal Cushing's syndrome. J. Clin. Endocrinol. Metab. 75, 826–832 (1992).
Emral, R. et al. Prevalence of subclinical Cushing's syndrome in 70 patients with adrenal incidentaloma: clinical, biochemical and surgical outcomes. Endocr. J. 50, 399–408 (2003).
Comlekci, A. et al. Adrenal incidentaloma, clinical, metabolic, follow-up aspects: single centre experience. Endocrine 37, 40–46 (2010).
Morelli, V. et al. Subclinical hypercortisolism: correlation between biochemical diagnostic criteria and clinical aspects. Clin. Endocrinol. (Oxf.) 73, 161–166 (2010).
Giordano, R. et al. Long-term morphological, hormonal, and clinical follow-up in a single unit on 118 patients with adrenal incidentalomas. Eur. J. Endocrinol. 162, 779–785 (2010).
Fernández-Real, J. M., Gonzalbez, J. & Ricart, W. Metabolic abnormalities in patients with adrenal incidentaloma. J. Clin. Endocrinol. Metab. 86, 950–952 (2001).
Tauchmanovà, L. et al. Bone loss determined by quantitative ultrasonometry correlates inversely with disease activity in patients with endogenous glucocorticoid excess due to adrenal mass. Eur. J. Endocrinol. 145, 241–247 (2001).
Chiodini, I. et al. Spinal volumetric bone mineral density and vertebral fractures in female patients with adrenal incidentalomas: the effects of subclinical hypercortisolism and gonadal status. J. Clin. Endocrinol. Metab. 89, 2237–2241 (2004).
Chiodini, I. et al. Subclinical hypercortisolism among outpatients referred for osteoporosis. Ann. Intern. Med. 147, 541–548 (2007).
Chiodini, I. et al. Bone mineral density, prevalence of vertebral fractures, and bone quality in patients with adrenal incidentalomas with and without subclinical hypercortisolism: an Italian multicenter study. J. Clin. Endocrinol. Metab. 94, 3207–3214 (2009).
Chiodini, I. et al. Bone involvement in eugonadal male patients with adrenal incidentaloma and subclinical hypercortisolism. J. Clin. Endocrinol. Metab. 87, 5491–5494 (2002).
Chiodini, I. et al. Eugonadal male patients with adrenal incidentalomas and subclinical hypercortisolism have increased rate of vertebral fractures. Clin. Endocrinol. (Oxf.) 70, 208–213 (2009).
Osella, G. et al. Serum markers of bone and collagen turnover in patients with Cushing's syndrome and in subjects with adrenal incidentalomas. J. Clin. Endocrinol. Metab. 82, 3303–3307 (1997).
Bardet, S. et al. Bone mineral density and biological markers of bone repair in patients with adrenal incidentaloma: effect of subclinical hypercortisolism [French]. Rev. Med. Interne 23, 508–517 (2002).
Hadjidakis, D. et al. Does subclinical hypercortisolism adversely affect the bone mineral density of patients with adrenal incidentalomas? Clin. Endocrinol. (Oxf.) 58, 72–77 (2003).
Torlontano, M. et al. Altered bone mass and turnover in female patients with adrenal incidentaloma: the effect of subclinical hypercortisolism. J. Clin. Endocrinol. Metab. 84, 2381–2385 (1999).
Sereg, M. et al. Atherosclerotic risk factors and complications in patients with non-functioning adrenal adenomas treated with or without adrenalectomy: a long-term follow-up study. Eur. J. Endocrinol. 160, 647–655 (2009).
Erbil, Y. et al. Cardiovascular risk in patients with nonfunctional adrenal incidentaloma: myth or reality? World J. Surg. 33, 2099–2105 (2009).
Yilmaz, H., Tütüncü, N. B. & Sahin, M. Two-year follow-up of thirty-two non-functional benign adrenal incidentalomas. J. Endocrinol. Invest. 32, 913–916 (2009).
Erbil, Y. et al. Evaluation of the cardiovascular risk in patients with subclinical Cushing syndrome before and after surgery. World J. Surg. 30, 1665–1671 (2006).
Vasiliadi, D. et al. Glucocortidoid sensitivity assessed in peripheral blood cells do not correlate with the feedback sensitivity of the hypothalamo-pituitary adrenal axis. Hormones (Athens) 1, 233–238 (2002).
Huizenga, N. A. et al. Interperson variability but intraperson stability of baseline plasma cortisol concentrations, and its relation to feedback sensitivity of the hypothalamo-pituitary-adrenal axis to a low dose of dexamethasone in elderly individuals. J. Clin. Endocrinol. Metab. 83, 47–54 (1998).
Mitchell, I. C. et al. “Subclinical Cushing's syndrome” is not subclinical: improvement after adrenalectomy in 9 patients. Surgery 142, 900–905 (2007).
Lindholm, J. et al. Incidence and late prognosis of cushing's syndrome: a population-based study. J. Clin. Endocrinol. Metab. 86, 117–123 (2001).
Midorikawa, S., Sanada, H., Hashimoto, S., Suzuki, T. & Watanabe, T. The improvement of insulin resistance in patients with adrenal incidentaloma by surgical resection. Clin. Endocrinol. (Oxf.) 54, 797–804 (2001).
Guerrieri, M. et al. Primary adrenal hypercortisolism: minimally invasive surgical treatment or medical therapy? A retrospective study with long-term follow-up evaluation. Surg. Endosc. 24, 2542–2546 (2010).
Acknowledgements
C. P. Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the Medscape, LLC-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Contributions
Both authors researched the data for the article, provided a substantial contribution to discussions of the content, contributed equally to writing the article and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Vassiliadi, D., Tsagarakis, S. Endocrine incidentalomas—challenges imposed by incidentally discovered lesions. Nat Rev Endocrinol 7, 668–680 (2011). https://doi.org/10.1038/nrendo.2011.92
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrendo.2011.92
This article is cited by
-
Nebennierenvenensampling bei primärem Hyperaldosteronismus machbar?
Journal für Klinische Endokrinologie und Stoffwechsel (2021)
-
The prevalence and characteristics of non-functioning and autonomous cortisol secreting adrenal incidentaloma after patients’ stratification by body mass index and age
BMC Endocrine Disorders (2020)
-
Prevalence of incidental thyroid malignancy on routine 18F-fluorodeoxyglucose PET-CT in a large teaching hospital
European Journal of Hybrid Imaging (2020)
-
Management of adrenocortical carcinoma: a consensus statement of the Italian Society of Endocrinology (SIE)
Journal of Endocrinological Investigation (2016)
-
Risk Estimator for Adrenal Tumor Functionality
World Journal of Surgery (2014)