Abstract
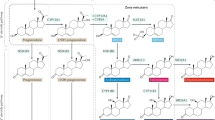
Aromatase, an enzyme located in the endoplasmic reticulum of estrogen-producing cells, catalyzes the rate-limiting step in the conversion of androgens to estrogens in many tissues. The clinical features of patients with defects in CYP19A1, the gene encoding aromatase, have revealed a major role for this enzyme in epiphyseal plate closure, which has promoted interest in the use of inhibitors of aromatase to improve adult height. The availability of the selective aromatase inhibitors letrozole and anastrozole—currently approved as adjuvant therapy for breast cancer—have stimulated off-label use of aromatase inhibitors in pediatrics for the following conditions: hyperestrogenism, such as aromatase excess syndrome, Peutz–Jeghers syndrome, McCune–Albright syndrome and functional follicular ovarian cysts; hyperandrogenism, for example, testotoxicosis (also known as familial male-limited precocious puberty) and congenital adrenal hyperplasia; pubertal gynecomastia; and short stature and/or pubertal delay in boys. Current data suggest that aromatase inhibitors are probably effective in the treatment of patients with aromatase excess syndrome or testotoxicosis, partially effective in Peutz–Jeghers and McCune–Albright syndrome, but probably ineffective in gynecomastia. Insufficient data are available in patients with congenital adrenal hyperplasia or functional ovarian cysts. Although aromatase inhibitors appear effective in increasing adult height of boys with short stature and/or pubertal delay, safety concerns, including vertebral deformities, a decrease in serum HDL cholesterol levels and increase of erythrocytosis, are reasons for caution.
Key Points
-
Aromatase is expressed in many tissues and converts androgens to estrogens in a tissue-specific fashion
-
The third-generation aromatase inhibitors anastrozole and letrozole suppress estrogen production by 97–99% and are highly selective
-
Animal experiments have shown that the role of estrogen in growth regulation is different from that in humans, but have highlighted possible adverse effects of aromatase inhibitor use
-
Contrary to theoretical expectations, aromatase inhibitors appear ineffective in the treatment of pubertal gynecomastia
-
Evidence from controlled and uncontrolled studies in boys with short stature and/or pubertal delay suggests a positive effect of aromatase inhibitors on adult height, but more follow-up data are needed
-
The use of aromatase inhibitors in prepubertal boys is not advised because of an association with vertebral deformities
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Santen, R. J., Brodie, H., Simpson, E. R., Siiteri, P. K. & Brodie, A. History of aromatase: Saga of an important biological mediator and therapeutic target. Endocr. Rev. 30, 343–375 (2009).
Smith, E. P. et al. Estrogen resistance caused by a mutation in the estrogen-receptor gene in a man. N. Engl. J. Med. 331, 1056–1061 (1994).
Conte, F. A., Grumbach, M. M., Ito, Y., Fisher, C. R. & Simpson, E. R. A syndrome of female pseudohermaphrodism, hypergonadotropic hypogonadism, and multicystic ovaries associated with missense mutations in the gene encoding aromatase (P450arom). J. Clin. Endocrinol. Metab. 78, 1287–1292 (1994).
Morishima, A., Grumbach, M. M., Simpson, E. R., Fisher, C. & Qin, K. Aromatase deficiency in male and female siblings caused by a novel mutation and the physiological role of estrogens. J. Clin. Endocrinol. Metab. 80, 3689–3698 (1995).
Carani, C. et al. Effect of testosterone and estradiol in a man with aromatase deficiency. N. Engl. J. Med. 337, 91–95 (1997).
Bilezikian, J. P., Morishima, A., Bell, J. & Grumbach, M. M. Increased bone mass as a result of estrogen therapy in a man with aromatase deficiency. N. Engl. J. Med. 339, 599–603 (1998).
Herrmann, B. L. et al. Impact of estrogen replacement therapy in a male with congenital aromatase deficiency caused by a novel mutation in the CYP19 gene. J. Clin. Endocrinol. Metab. 87, 5476–5484 (2002).
Wickman, S., Sipilä, I., Ankarberg-Lindgren, C., Norjavaara, E. & Dunkel, L. A specific aromatase inhibitor and potential increase in adult height in boys with delayed puberty: a randomised controlled trial. Lancet 357, 1743–1748 (2001).
Hero, M., Norjavaara, E. & Dunkel, L. Inhibition of estrogen biosynthesis with a potent aromatase inhibitor increases predicted adult height in boys with idiopathic short stature: a randomized controlled trial. J. Clin. Endocrinol. Metab. 90, 6396–6402 (2005).
Mauras, N. et al. Anastrozole increases predicted adult height of short adolescent males treated with growth hormone: a randomized, placebo-controlled, multicenter trial for one to three years. J. Clin. Endocrinol. Metab. 93, 823–831 (2008).
Salehpour, S. et al. A double-blind, placebo-controlled comparison of letrozole to oxandrolone effects upon growth and puberty of children with constitutional delay of puberty and idiopathic short stature. Horm. Res. Paediatr. 74, 428–435 (2010).
Cernich, J., Jacobson, J. D., Moore, W. V. & Popovic, J. Use of aromatase inhibitors in children with short stature. Pediatr. Endocrinol. Rev. 2, 2–7 (2004).
Dunkel, L. Use of aromatase inhibitors to increase final height. Mol. Cell Endocrinol. 254–255, 207–216 (2006).
Shulman, D. I., Francis, G. L., Palmert, M. R. & Eugster, E. A. Use of aromatase inhibitors in children and adolescents with disorders of growth and adolescent development. Pediatrics 121, e975–e983 (2008).
Geffner, M. E. For debate: Aromatase inhibitors to augment height: have we lost our inhibitions? Pediatr. Endocrinol. Rev. 5, 756–759 (2008).
Dunkel, L. Update on the role of aromatase inhibitors in growth disorders. Horm. Res. 71 (Suppl. 1), 57–63 (2009).
Geffner, M. E. Aromatase inhibitors to augment height: continued caution and study required. J. Clin. Res. Pediatr. Endocrinol. 1, 256–261 (2009).
Diaz-Thomas, A. & Shulman, D. Use of aromatase inhibitors in children and adolescents: what's new? Curr. Opin. Pediatr. 22, 501–507 (2010).
Kish, M. A. Guide to development of practice guidelines. Clin. Infect. Dis. 32, 851–854 (2001).
AGREE Collaboration. Development and validation of an international appraisal instrument for assessing the quality of clinical practice guidelines: the AGREE project. Qual. Saf. Health Care 12, 18–23 (2003).
Cavalli, A. et al. Enantioselective nonsteroidal aromatase inhibitors identified through a multidisciplinary medicinal chemistry approach. J. Med. Chem. 48, 7282–7289 (2005).
Sebastian, S., Takayama, K., Shozu, M. & Bulun, S. E. Cloning and characterization of a novel endothelial promoter of the human CYP19 (aromatase P450) gene that is upregulated in breast cancer tissue. Mol. Endocrinol. 16, 2243–2254 (2002).
Bulun, S. E. et al. The human CYP19 (aromatase P450) gene: update on physiologic roles and genomic organization of promoters. J. Steroid Biochem. Mol. Biol. 86, 219–224 (2003).
Labrie, F., Bélanger, A., Cusan, L. & Candas, B. Physiological changes in dehydroepiandrosterone are not reflected by serum levels of active androgens and estrogens but of their metabolites: intracrinology. J. Clin. Endocrinol. Metab. 82, 2403–2409 (1997).
Corbin, C. J. et al. Isolation of a full-length cDNA insert encoding human aromatase system cytochrome P-450 and its expression in nonsteroidogenic cells. Proc. Natl Acad. Sci. USA 85, 8948–8952 (1988).
Grumbach, M. M. & Auchus, R. J. Estrogen: consequences and implications of human mutations in synthesis and action. J. Clin. Endocrinol. Metab. 84, 4677–4694 (1999).
Drop, S. L., De Waal, W. J. & De Muinck Keizer-Schrama, S. M. Sex steroid treatment of constitutionally tall stature. Endocr. Rev. 19, 540–558 (1998).
Juul, A. et al. Serum insulin-like growth factor-I in 1030 healthy children, adolescents, and adults: relation to age, sex, stage of puberty, testicular size, and body mass index. J. Clin. Endocrinol. Metab. 78, 744–752 (1994).
Mauras, N. et al. Pharmacokinetics and dose finding of a potent aromatase inhibitor, aromasin (exemestane), in young males. J. Clin. Endocrinol. Metab. 88, 5951–5956 (2003).
Bisagni, G. et al. Letrozole, a new oral non-steroidal aromastase inhibitor in treating postmenopausal patients with advanced breast cancer. A pilot study. Ann. Oncol. 7, 99–102 (1996).
Bajetta, E. et al. Double-blind, randomised, multicentre endocrine trial comparing two letrozole doses, in postmenopausal breast cancer patients. Eur. J. Cancer 35, 208–213 (1999).
Karmazin, A., Moore, W. V., Popovic, J. & Jacobson, J. D. The effect of letrozole on bone age progression, predicted adult height, and adrenal gland function. J. Pediatr. Endocrinol. Metab. 18, 285–293 (2005).
Mauras, N. et al. Pharmacokinetics and pharmacodynamics of anastrozole in pubertal boys with recent-onset gynecomastia. J. Clin. Endocrinol. Metab. 94, 2975–2978 (2009).
Mauras, N., O'Brien, K. O., Klein, K. O. & Hayes, V. Estrogen suppression in males: metabolic effects. J. Clin. Endocrinol. Metab. 85, 2370–2377 (2000).
Geisler, J., Haynes, B., Anker, G., Dowsett, M. & Lønning, P. E. Influence of letrozole and anastrozole on total body aromatization and plasma estrogen levels in postmenopausal breast cancer patients evaluated in a randomized, cross-over study. J. Clin. Oncol. 20, 751–757 (2002).
Chagin, A. S. & Sävendahl, L. Oestrogen receptors and linear bone growth. Acta Pædiatr. 96, 1275–1279 (2007).
Fisher, C. R., Graves, K. H., Parlow, A. F. & Simpson, E. R. Characterization of mice deficient in aromatase (ArKO) because of targeted disruption of the Cyp19 gene. Proc. Natl Acad. Sci. USA 95, 6965–6970 (1998).
Oz, O. K. et al. Bone has a sexually dimorphic response to aromatase deficiency. J. Bone Miner. Res. 15, 507–514 (2000).
Oz, O. K. et al. Bone phenotype of the aromatase deficient mouse. J. Steroid Biochem. Mol. Biol. 79, 49–59 (2001).
Britt, K. L. et al. The ovarian phenotype of the aromatase knockout (ArKO) mouse. J. Steroid Biochem. Mol. Biol. 79, 181–185 (2001).
Jones, M. E., McInnes, K. J., Boon, W. C. & Simpson, E. R. Estrogen and adiposity—utilizing models of aromatase deficiency to explore the relationship. J. Steroid Biochem. Mol. Biol. 106, 3–7 (2007).
Gevers, E. F., Wit, J. M. & Robinson, I. C. Effects of long-term gonadotrophin-releasing hormone analog treatment on growth, growth hormone (GH) secretion, GH receptors, and GH-binding protein in the rat. Pediatr. Res. 43, 111–120 (1998).
Vanderschueren, D. et al. Aromatase inhibition impairs skeletal modeling and decreases bone mineral density in growing male rats. Endocrinology 138, 2301–2307 (1997).
van Gool, S. A. et al. Impaired body weight and tail length gain and altered bone quality after treatment with the aromatase inhibitor exemestane in male rats. Horm. Res. Paediatr. 73, 376–385 (2010).
Bajpai, A. et al. Peripubertal aromatase inhibition in male rats has adverse long-term effects on bone strength and growth and induces prostatic hyperplasia. J. Endocrinol. 207, 27–34 (2010).
Eshet, R. et al. The aromatase inhibitor letrozole increases epiphyseal growth plate height and tibial length in peripubertal male mice. J. Endocrinol. 182, 165–172 (2004).
Turner, K. J., Morley, M., Atanassova, N., Swanston, I. D. & Sharpe, R. M. Effect of chronic administration of an aromatase inhibitor to adult male rats on pituitary and testicular function and fertility. J. Endocrinol. 164, 225–238 (2000).
van Gool, S. A. et al. Marginal growth increase, altered bone quality and polycystic ovaries in female prepubertal rats after treatment with the aromatase inhibitor exemestane. Horm. Res. Paediatr. 73, 49–60 (2010).
Mouridsen, H. et al. Letrozole therapy alone or in sequence with tamoxifen in women with breast cancer. N. Engl. J. Med. 361, 766–776 (2009).
Gibson, L., Lawrence, D., Dawson, C. & Bliss, J. Aromatase inhibitors for treatment of advanced breast cancer in postmenopausal women. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD003370 doi:10.1002/14651858.CD003370.pub3 (2009).
Casper, R. F. & Mitwally, M. F. Review: aromatase inhibitors for ovulation induction. J. Clin. Endocrinol. Metab. 91, 760–771 (2006).
Bohlmann, M. K. et al. Off-label use of aromatase inhibitors: an alternative in reproductive medicine and in other nonmammary diseases? [German]. Gynäkologische Endokrinologie 6, 221–228 (2008).
Raman, J. D. & Schlegel, P. N. Aromatase inhibitors for male infertility. J. Urol. 167, 624–629 (2002).
Shozu, M. et al. Estrogen excess associated with novel gain-of-function mutations affecting the aromatase gene. N. Engl. J. Med. 348, 1855–1865 (2003).
Demura, M. et al. Regional rearrangements in chromosome 15q21 cause formation of cryptic promoters for the CYP19 (aromatase) gene. Hum. Mol. Genet. 16, 2529–2541 (2007).
Stratakis, C. A. et al. The aromatase excess syndrome is associated with feminization of both sexes and autosomal dominant transmission of aberrant P450 aromatase gene transcription. J. Clin. Endocrinol. Metab. 83, 1348–1357 (1998).
Martin, R. M. et al. Familial hyperestrogenism in both sexes: clinical, hormonal, and molecular studies of two siblings. J. Clin. Endocrinol. Metab. 88, 3027–3034 (2003).
Binder, G. et al. Dominant transmission of prepubertal gynecomastia Binder, G. et al. Dominant transmission of prepubertal gynecomastia due to serum estrone excess: hormonal, biochemical, and genetic analysis in a large kindred. J. Clin. Endocrinol. Metab. 90, 484–492 (2005).
Kara, C., Kutlu, A. O., Tosun, M. S., Apaydin, S. & Senel, F. Sertoli cell tumor causing prepubertal gynecomastia in a boy with Peutz–Jeghers syndrome: the outcome of 1-year treatment with the aromatase inhibitor testolactone. Horm. Res. 63, 252–256 (2005).
Lefevre, H. et al. Prepubertal gynecomastia in Peutz–Jeghers syndrome: incomplete penetrance in a familial case and management with an aromatase inhibitor. Eur. J. Endocrinol. 154, 221–227 (2006).
Grandone, A. et al. Prepubertal gynecomastia in two monozygotic twins with Peutz–Jeghers syndrome: two years' treatment with anastrozole and genetic study. Horm. Res. Paediatr. 75, 374–379 (2011).
Weinstein, L. S. et al. Activating mutations of the stimulatory G protein in the McCune–Albright syndrome. N. Engl. J. Med. 325, 1688–1695 (1991).
Shenker, A. et al. Severe endocrine and nonendocrine manifestations of the McCune–Albright syndrome associated with activating mutations of stimulatory G protein GS. J. Pediatr. 123, 509–518 (1993).
Foster, C. M. et al. Ovarian function in girls with McCune–Albright syndrome. Pediatr. Res. 20, 859–863 (1986).
Feuillan, P. P. McCune–Albright syndrome. Curr. Ther. Endocrinol. Metab. 6, 235–239 (1997).
Feuillan, P. P. et al. Treatment of precocious puberty in the McCune–Albright syndrome with the aromatase inhibitor testolactone. N. Engl. J. Med. 315, 1115–1119 (1986).
Feuillan, P. P., Jones, J. & Cutler, G. B. Jr. Long-term testolactone therapy for precocious puberty in girls with the McCune–Albright syndrome. J. Clin. Endocrinol. Metab. 77, 647–651 (1993).
Nunez, S. B., Calis, K., Cutler, G. B. Jr, Jones, J. & Feuillan, P. P. Lack of efficacy of fadrozole in treating precocious puberty in girls with the McCune–Albright syndrome. J. Clin. Endocrinol. Metab. 88, 5730–5733 (2003).
Feuillan, P. et al. Letrozole treatment of precocious puberty in girls with the McCune–Albright syndrome: a pilot study. J. Clin. Endocrinol. Metab. 92, 2100–2106 (2007).
Mieszczak, J., Lowe, E. S., Plourde, P. & Eugster, E. A. The aromatase inhibitor anastrozole is ineffective in the treatment of precocious puberty in girls with McCune–Albright syndrome. J. Clin. Endocrinol. Metab. 93, 2751–2754 (2008).
Engiz, O., Berberoglu, M., Siklar, Z., Bilir, P. & Ocal, G. Treatment of autonomous ovarian follicular cyst with long-term anastrozole therapy. Indian J. Pediatr. 76, 950–951 (2009).
Eugster, E. A. Peripheral precocious puberty: causes and current management. Horm. Res. 71, 64–67 (2009).
Laue, L. et al. Treatment of familial male precocious puberty with spironolactone and testolactone. N. Engl. J. Med. 320, 496–502 (1989).
Laue, L., Jones, J., Barnes, K. M. & Cutler, G. B. Jr. Treatment of familial male precocious puberty with spironolactone, testolactone, and deslorelin. J. Clin. Endocrinol. Metab. 76, 151–155 (1993).
Leschek, E. W., Jones, J., Barnes, K. M., Hill, S. C. & Cutler, G. B. Jr. Six-year results of spironolactone and testolactone treatment of familial male-limited precocious puberty with addition of deslorelin after central puberty onset. J. Clin. Endocrinol. Metab. 84, 175–178 (1999).
Kreher, N. C., Pescovitz, O. H., Delameter, P., Tiulpakov, A. & Hochberg, Z. Treatment of familial male-limited precocious puberty with bicalutamide and anastrozole. J. Pediatr. 149, 416–420 (2006).
Lenz, A. M. et al. Bicalutamide and third-generation aromatase inhibitors in testotoxicosis. Pediatrics 126, e728–e733 (2010).
Eyssette-Guerreau, S. et al. Effectiveness of anastrozole and cyproterone acetate in two brothers with familial male precocious puberty. J. Pediatr. Endocrinol. Metab. 21, 995–1002 (2008).
Reiter, E. O. et al. Bicalutamide plus anastrozole for the treatment of gonadotropin-independent precocious puberty in boys with testotoxicosis: a phase II, open-label pilot study (BATT). J. Pediatr. Endocrinol. Metab. 23, 999–1009 (2010).
Eugster, E. A. et al. Height outcome in congenital adrenal hyperplasia caused by 21-hydroxylase deficiency: a meta-analysis. J. Pediatr. 138, 26–32 (2001).
Van der Kamp, H. J. et al. Longitudinal analysis of growth and puberty in 21-hydroxylase deficiency patients. Arch. Dis. Child. 87, 139–144 (2002).
Bonfig, W., Bechtold, S., Schmidt, H., Knorr, D. & Schwarz, H. P. Reduced final height outcome in congenital adrenal hyperplasia under prednisone treatment: deceleration of growth velocity during puberty. J. Clin. Endocrinol. Metab. 92, 1635–1639 (2007).
Merke, D. P. et al. Flutamide, testolactone, and reduced hydrocortisone dose maintain normal growth velocity and bone maturation despite elevated androgen levels in children with congenital adrenal hyperplasia. J. Clin. Endocrinol. Metab. 85, 1114–1120 (2000).
Warne, G. L., Grover, S. & Zajac, J. D. Hormonal therapies for individuals with intersex conditions: protocol for use. Treat. Endocrinology 4, 19–29 (2005).
Braunstein, G. D. Gynecomastia. N. Engl. J. Med. 328, 490–495 (1993).
Ma, N. S. & Geffner, M. E. Gynecomastia in prepubertal and pubertal men. Curr. Opin. Pediatr. 20, 465–470 (2008).
Nydick, M., Bustos, J., Dale, J. H. Jr & Rawson, R. W. Gynecomastia in adolescent boys. JAMA 178, 449–454 (1961).
Plourde, P. V. et al. Safety and efficacy of anastrozole for the treatment of pubertal gynecomastia: a randomized, double-blind, placebo-controlled trial. J. Clin. Endocrinol. Metab. 89, 4428–4433 (2004).
Lawrence, S. E., Faught, K. A., Vethamuthu, J. & Lawson, M. L. Beneficial effects of raloxifene and tamoxifen in the treatment of pubertal gynecomastia. J. Pediatr. 145, 71–76 (2004).
Grumbach, M. M. Estrogen, bone, growth and sex: a sea change in conventional wisdom. J. Pediatr. Endocrinol. Metab. 13 (Suppl. 6), 1439–1455 (2000).
Mauras, N. Strategies for maximizing growth in puberty in children with short stature. Endocrinol. Metab. Clin. North Am. 38, 613–624 (2009).
Carel, J. C. et al. Consensus statement on the use of gonadotropin-releasing hormone analogs in children. Pediatrics 123, e752–e762 (2009).
Carel, J. C. Management of short stature with GnRH agonist and co-treatment with growth hormone: a controversial issue. Mol. Cell Endocrinol. 254–255, 226–233 (2006).
van Gool, S. A. et al. Final height outcome after three years of growth hormone and gonadotropin-releasing hormone agonist treatment in short adolescents with relatively early puberty. J. Clin. Endocrinol. Metab. 92, 1402–1408 (2007).
Yanovski, J. A. et al. Treatment with a luteinizing hormone-releasing hormone agonist in adolescents with short stature. N. Engl. J. Med. 348, 908–917 (2003).
Kreher, N. C., Eugster, E. A. & Shankar, R. R. The use of tamoxifen to improve height potential in short pubertal boys. Pediatrics 116, 1513–1515 (2005).
Hero, M., Wickman, S. & Dunkel, L. Treatment with the aromatase inhibitor letrozole during adolescence increases near-final height in boys with constitutional delay of puberty. Clin. Endocrinol. (Oxf.) 64, 510–513 (2006).
Martin, M. M., Martin, A. L. A. & Mossman, K. L. Testosterone treatment of constitutional delay in growth and development: effect of dose on predicted versus definitive height. Acta Endocrinol. Suppl. (Copenh.) 279, 147–152 (1986).
Crowne, E. C., Shalet, S. M., Wallace, W. H., Eminson, D. M. & Price, D. A. Final height in boys with untreated constitutional delay in growth and puberty. Arch. Dis. Child. 65, 1109–1112 (1990).
LaFranchi, S., Hanna, C. E. & Mandel, S. H. Constitutional delay of growth: expected versus final adult height. Pediatrics 87, 82–87 (1991).
Albanese, A. & Stanhope, R. Does constitutional delayed puberty cause segmental disproportion and short stature. Eur. J. Pediatr. 152, 293–296 (1993).
Albanese, A. & Stanhope, R. Predictive factors in the determination of final height in boys with constitutional delay of growth and puberty. J. Pediatr. 126, 545–550 (1995).
Rekers-Mombarg, L. T. et al. Spontaneous growth in idiopathic short stature. European Study Group. Arch. Dis. Child. 75, 175–180 (1996).
Hero, M., Toiviainen-Salo, S., Wickman, S., Mäkitie, O. & Dunkel, L. Vertebral morphology in aromatase inhibitor-treated males with idiopathic short stature or constitutional delay of puberty. J. Bone Miner. Res. 25, 1536–1543 (2010).
Mauras, N., Welch, S., Rini, A. & Klein, K. O. An open label 12-month pilot trial on the effects of the aromatase inhibitor anastrozole in growth hormone (GH)-treated GH deficient adolescent boys. J. Pediatr. Endocrinol. Metab. 17, 1597–1606 (2004).
Hagenas, L. Growth rate can be manipulated. Estrogen production in pubertal boys can be blocked by an aromatase inhibitor [Swedish]. Lakartidningen. 99, 165–168 (2002).
Faglia, G., Arosio, M. & Porretti, S. Delayed closure of epiphyseal cartilages induced by the aromatase inhibitor anastrozole. Would it help short children grow up? J. Endocrinol. Invest. 23, 721–723 (2000).
Balestrieri, A., Faustini-Fustini, M., Rochira, V. & Carani, C. Clinical implications and management of oestrogen deficiency in the male. Clin. Endocrinol. (Oxf.) 54, 431–432 (2001).
Maffei, L. et al. Dysmetabolic syndrome in a man with a novel mutation of the aromatase gene: effects of testosterone, alendronate, and estradiol treatment. J. Clin. Endocrinol. Metab. 89, 61–70 (2004).
Jones, M. E., Boon, W. C., Proietto, J. & Simpson, E. R. Of mice and men: the evolving phenotype of aromatase deficiency. Trends Endocrinol. Metab. 17, 55–64 (2006).
Rochira, V., Zirilli, L., Madeo, B., Maffei, L. & Carani, C. Testosterone action on erythropoiesis does not require its aromatization to estrogen: Insights from the testosterone and estrogen treatment of two aromatase-deficient men. J. Steroid Biochem. Mol. Biol. 113, 189–194 (2009).
Rochira, V. et al. Tall stature without growth hormone: four male patients with aromatase deficiency. J. Clin. Endocrinol. Metab. 95, 1626–1633 (2010).
Gerardin, D. C. & Pereira, O. C. Reproductive changes in male rats treated perinatally with an aromatase inhibitor. Pharmacol. Biochem. Behav. 71, 301–305 (2002).
Wickman, S. & Dunkel, L. Inhibition of P450 aromatase enhances gonadotropin secretion in early and midpubertal boys: evidence for a pituitary site of action of endogenous E. J. Clin. Endocrinol. Metab. 86, 4887–4894 (2001).
Haynes, B. P., Dowsett, M., Miller, W. R., Dixon, J. M. & Bhatnagar, A. S. The pharmacology of letrozole. J. Steroid Biochem. Mol. Biol. 87, 35–45 (2003).
Seftel, A. Testosterone replacement therapy for male hypogonadism: part III. Pharmacologic and clinical profiles, monitoring, safety issues, and potential future agents. Int. J. Impot. Res. 19, 2–24 (2007).
Hero, M., Wickman, S., Hanhijärvi, R., Siimes, M. A. & Dunkel, L. Pubertal upregulation of erythropoiesis in boys is determined primarily by androgen. J. Pediatr. 146, 245–252 (2005).
Hero, M., Ankarberg-Lindgren, C., Taskinen, M. R. & Dunkel, L. Blockade of oestrogen biosynthesis in peripubertal boys: effects on lipid metabolism, insulin sensitivity, and body composition. Eur. J. Endocrinol. 155, 453–460 (2006).
Couse, J. F. & Korach, K. S. Estrogen receptor null mice: what have we learned and where will they lead us? Endocr. Rev. 20, 358–417 (1999).
Robertson, K. M. et al. Impairment of spermatogenesis in mice lacking a functional aromatase (Cyp19) gene. Proc. Natl Acad. Sci. USA 96, 7986–7991 (1999).
Pentikainen, V., Erkkilä, K., Suomalainen, L., Parvinen, M. & Dunkel, L. Estradiol acts as a germ cell survival factor in the human testis in vitro. J. Clin. Endocrinol. Metab. 85, 2057–2067 (2000).
Shetty, G., Krishnamurthy, H., Krishnamurthy, H. N., Bhatnagar, S. & Moudgal, R. N. Effect of estrogen deprivation on the reproductive physiology of male and female primates. J. Steroid Biochem. Mol. Biol. 61, 157–166 (1997).
Aquila, S. et al. Towards a physiological role for cytochrome P450 aromatase in ejaculated human sperm. Hum. Reprod. 18, 1650–1659 (2003).
Mauras, N., Bell, J., Snow, B. G. & Winslow, K. L. Sperm analysis in growth hormone-deficient adolescents previously treated with an aromatase inhibitor: comparison with normal controls. Fertil. Steril. 84, 239–242 (2005).
Ramasamy, R. et al. Successful fertility treatment for Klinefelter's syndrome. J. Urol. 182, 1108–1113 (2009).
Bonjour, J. P. & Chevalley, T. Pubertal timing, peak bone mass and fragility fracture risk. Bonekey Osteovision 4, 30–48 (2007).
McCloskey, E. V. Aromatase inhibitors and bone health. Bonekey Osteovision 3, 5–13 (2006).
Hero, M. et al. Impact of aromatase inhibitor therapy on bone turnover, cortical bone growth and vertebral morphology in pre- and peripubertal boys with idiopathic short stature. Horm. Res. 71, 290–297 (2009).
Lorentzon, M., Swanson, C., Andersson, N., Mellström, D. & Ohlsson, C. Free testosterone is a positive, whereas free estradiol is a negative, predictor of cortical bone size in young Swedish men: the GOOD study. J. Bone Miner. Res. 20, 1334–1341 (2005).
Seeman, E. Clinical review 137: Sexual dimorphism in skeletal size, density, and strength. J. Clin. Endocrinol. Metab. 86, 4576–4584 (2001).
Wickman, S., Kajantie, E. & Dunkel, L. Effects of suppression of estrogen action by the p450 aromatase inhibitor letrozole on bone mineral density and bone turnover in pubertal boys. J. Clin. Endocrinol. Metab. 88, 3785–3793 (2003).
Leder, B. Z., LeBlanc, K. M., Schoenfeld, D. A., Eastell, R. & Finkelstein, J. S. Differential effects of androgens and estrogens on bone turnover in normal men. J. Clin. Endocrinol. Metab. 88, 204–210 (2003).
Michael, H., Härkönen, P. L., Väänänen, H. K. & Hentunen, T. A. Estrogen and testosterone use different cellular pathways to inhibit osteoclastogenesis and bone resorption. J. Bone Miner. Res. 20, 2224–2232 (2005).
Seeman, E. & Delmas, P. D. Bone quality—the material and structural basis of bone strength and fragility. N. Engl. J. Med. 354, 2250–2261 (2006).
Ma, D. & Jones, G. The association between bone mineral density, metacarpal morphometry, and upper limb fractures in children: a population-based case-control study. J. Clin. Endocrinol. Metab. 88, 1486–1491 (2003).
Bouillon, R., Bex, M., Vanderschueren, D. & Boonen, S. Estrogens are essential for male pubertal periosteal bone expansion. J. Clin. Endocrinol. Metab. 89, 6025–6029 (2004).
Lee, K., Jessop, H., Suswillo, R., Zaman, G. & Lanyon, L. Endocrinology: bone adaptation requires oestrogen receptor α. Nature 424, 389 (2003).
Metzger, D. L. & Kerrigan, J. R. Estrogen receptor blockade with tamoxifen diminishes growth hormone secretion in boys: evidence for a stimulatory role of endogenous estrogens during male adolescence. J. Clin. Endocrinol. Metab. 79, 513–518 (1994).
Wickman, S., Saukkonen, T. & Dunkel, L. The role of sex steroids in the regulation of insulin sensitivity and serum lipid concentrations during male puberty: a prospective study with a P450-aromatase inhibitor. Eur. J. Endocrinol. 146, 339–346 (2002).
Tikkanen, M. J. & Nikkilä, E. A. Regulation of hepatic lipase and serum lipoproteins by sex steroids. Am. Heart J. 113, 562–567 (1987).
Sorva, R., Kuusi, T., Dunkel, L. & Taskinen, M. R. Effects of endogenous sex steroids on serum lipoproteins and postheparin plasma lipolytic enzymes. J. Clin. Endocrinol. Metab. 66, 408–413 (1988).
Moran, A. et al. Association between the insulin resistance of puberty and the insulin-like growth factor-I/growth hormone axis. J. Clin. Endocrinol. Metab. 87, 4817–4820 (2002).
Phillips, K. A., Ribi, K. & Fisher, R. Do aromatase inhibitors have adverse effects on cognitive function? Breast Cancer Res. 13, 203 (2011).
Osterlund, M. K., Gustafsson, J. A., Keller, E. & Hurd, Y. L. Estrogen receptor β (ERβ) messenger ribonucleic acid (mRNA) expression within the human forebrain: distinct distribution pattern to ERα mRNA. J. Clin. Endocrinol. Metab. 85, 3840–3846 (2000).
Cherrier, M. M. et al. The role of aromatization in testosterone supplementation: effects on cognition in older men. Neurology 64, 290–296 (2005).
Kil, K. E. et al. Synthesis and PET studies of [11C-cyano]letrozole (Femara), an aromatase inhibitor drug. Nucl. Med. Biol. 36, 215–223 (2009).
Jenkins, V. A. et al. Effects of anastrozole on cognitive performance in postmenopausal women: a randomised, double-blind chemoprevention trial (IBIS II). Lancet Oncol. 9, 953–961 (2008).
Young, L. A., Neiss, M. B., Samuels, M. H., Roselli, C. E. & Janowsky, J. S. Cognition is not modified by large but temporary changes in sex hormones in men. J. Clin. Endocrinol. Metab. 95, 280–288 (2010).
Hero, M., Maury, S., Luotoniemi, E., Service, E. & Dunkel, L. Cognitive effects of aromatase inhibitor therapy in peripubertal boys. Eur. J. Endocrinol. 163, 149–155 (2010).
Dixon, J. M. et al. Letrozole suppresses plasma estradiol and estrone sulphate more completely than anastrozole in postmenopausal women with breast cancer. J. Clin. Oncol. 26, 1671–1676 (2008).
de Jong, P. C. et al. Inhibition of breast cancer tissue aromatase activity and estrogen concentrations by the third-generation aromatase inhibitor vorozole. Cancer Res. 57, 2109–2111 (1997).
Author information
Authors and Affiliations
Contributions
All authors contributed equally to all aspects of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementry Information
Appendix 1. Literature search details (DOC 66 kb)
Rights and permissions
About this article
Cite this article
Wit, J., Hero, M. & Nunez, S. Aromatase inhibitors in pediatrics. Nat Rev Endocrinol 8, 135–147 (2012). https://doi.org/10.1038/nrendo.2011.161
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrendo.2011.161
This article is cited by
-
Aromatase Inhibitors May Increase the Risk of Cardiometabolic Complications in Adolescent Boys
Pediatric Cardiology (2024)
-
Paediatric and adult-onset male hypogonadism
Nature Reviews Disease Primers (2019)
-
Les Enjeux du Retard Pubertaire chez le Garçon
Journal für Gynäkologische Endokrinologie/Schweiz (2019)
-
Obesity’s role in secondary male hypogonadism: a review of pathophysiology and management issues
SN Comprehensive Clinical Medicine (2019)
-
Complications and Outcomes After Gynecomastia Surgery: Analysis of 204 Pediatric and 1583 Adult Cases from a National Multi-center Database
Aesthetic Plastic Surgery (2017)