Abstract
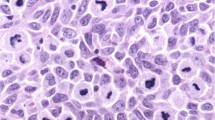
The number of melanoma cases in the elderly (>65 years) will rise over the coming decades, making it an important public health problem. Elderly white men are the demographic group who are at highest risk of being diagnosed with melanoma and of dying from this cancer. Among patients with melanoma, older age is recognized as an independent poor prognostic factor, but it remains unclear whether this relationship is due to a change in the biology of the disease with increasing patient age, declining host defenses, or both. Most elderly patients can have surgery to control locoregional disease, but might not be candidates for intensive biologic therapies for advanced melanoma because of comorbidities and inability to tolerate the adverse side effects of these treatments. Early detection remains an important strategy for the management of melanoma. Further research is needed to determine why older melanoma patients have a worse prognosis than their younger counterparts, even when matched for all other clinical and pathological predictors of survival outcomes.
Key Points
-
The number of melanoma cases among the elderly (>65 years) is expected to increase owing to the aging population
-
Older men are at higher risk of developing melanoma, and once diagnosed, are at higher risk of dying from this cancer compared with other demographic groups
-
Older men often present with thicker lesions and a truncal location compared with older women, making self-detection less likely
-
Melanomas in elderly patients often have poor prognostic features compared with younger patients, including ulceration, elevated mitotic rate, and head and neck location
-
Older age is an independent, adverse prognostic factor even after taking all other factors into account
-
Older patients are less likely to receive standard surgery for melanoma, although they usually tolerate these surgeries well
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
He, W., Sengupta, M., Velkoff, V. A. & DeBarros, K. A. 65+ in the United States. US Census Bureau [online], (2005).
Quaglia, A. et al. The cancer survival gap between elderly and middle-aged patients in Europe is widening. Eur. J. Cancer 45, 1006–1018 (2009).
Vercelli, M. et al. Relative survival in elderly European cancer patients: evidence for health care inequalities. The EUROCARE Working Group. Crit. Rev. Oncol. Hematol. 35, 161–179 (2000).
Horner, M. J. et al. SEER Cancer Statistics Review, 1975–2006 National Cancer Institute [online], (2009).
Linos, E., Swetter, S. M., Cockburn, M. G., Colditz, G. A. & Clarke, C. A. Increasing burden of melanoma in the United States. J. Invest. Dermatol. 129, 1666–1674 (2009).
Geller, A. C. et al. Strategies for improving melanoma education and screening for men age ≥50 years: findings from the American Academy of Dermatological National Skin Cancer Sreening Program. Cancer 95, 1554–1561 (2002).
Field, M. J. et al. Extending Medicare coverage for preventive and other services 38–62 (National Academy Press, Washington DC, 2000).
Berg, A. & US Preventive Services Task Force. Screening for skin cancer: Recommendations and rationale. Am. J. Prev. Med. 20 (Suppl. 1), 44–46 (2001).
Geller, A. C., Swetter, S. M., Brooks, K., Demierre, M. F. & Yaroch, A. L. Screening, early detection, and trends for melanoma: current status (2000–2006) and future directions. J. Am. Acad. Dermatol. 57, 555–572 (2007).
Jemal, A. et al. Cancer statistics, 2008. CA Cancer J. Clin. 58, 71–96 (2008).
Howe, H. L. et al. Annual report to the nation on the status of cancer (1973 through 1998), featuring cancers with recent increasing trends. J. Natl Cancer Inst. 93, 824–842 (2001).
Jemal, A., Devesa, S. S., Hartge, P. & Tucker, M. A. Recent trends in cutaneous melanoma incidence among whites in the United States. J. Natl Cancer Inst. 93, 678–683 (2001).
Balch, C. M. et al. Prognostic factors analysis of 17,600 melanoma patients: validation of the American Joint Committee on Cancer melanoma staging system. J. Clin. Oncol. 19, 3622–3634 (2001).
Balch, C. M. et al. Final version of the American Joint Committee on Cancer staging system for cutaneous melanoma. J. Clin. Oncol. 19, 3635–3648 (2001).
Schwartz, J. L. et al. Thin primary cutaneous melanomas: associated detection patterns, lesion characteristics, and patient characteristics. Cancer 95, 1562–1568 (2002).
Koh, H. K. et al. Who discovers melanoma? Patterns from a population-based survey. J. Am. Acad. Dermatol. 26, 914–919 (1992).
Brady, M. S. et al. Patterns of detection in patients with cutaneous melanoma. Cancer 89, 342–347 (2000).
Epstein, D. S., Lange, J. R., Gruber, S. B., Mofid, M. & Koch, S. E. Is physician detection associated with thinner melanomas? JAMA 2 81, 640–643 (1999).
de Vries, E. et al. Superior survival of females among 10,538 Dutch melanoma patients is independent of Breslow thickness, histologic type and tumor site. Ann. Oncol. 19, 583–589 (2008).
Murray, C. S., Stockton, D. L. & Doherty, V. R. Thick melanoma: the challenge persists. Br. J. Dermatol. 152, 104–109 (2005).
Demierre, M. F., Chung, C., Miller, D. R. & Geller, A. C. Early detection of thick melanomas in the United States: beware of the nodular subtype. Arch. Dermatol. 141, 745–750 (2005).
Chao, C. et al. Correlation between prognostic factors and increasing age in melanoma. Ann. Surg. Oncol. 11, 259–264 (2004).
Bergenmar, M., Hansson, J. & Brandberg, Y. Detection of nodular and superficial spreading melanoma with tumour thickness ≤2.0 mm—an interview study. Eur. J. Cancer Prev. 11, 49–55 (2002).
Paek, S. C. et al. The impact of factors beyond Breslow depth on predicting sentinel lymph node positivity in melanoma. Cancer 109, 100–108 (2007).
Statius Muller, M. G. et al. The sentinel lymph node status is an important factor for predicting clinical outcome in patients with stage I or II cutaneous melanoma. Cancer 91, 2401–2408 (2001).
Gershenwald, J. E. et al. Patterns of recurrence following a negative sentinel lymph node biopsy in 243 patients with stage I or II melanoma. J. Clin. Oncol. 16, 2253–2260 (1998).
Azzola, M. F. et al. Tumor mitotic rate is a more powerful prognostic indicator than ulceration in patients with primary cutaneous melanoma: an analysis of 3661 patients from a single center. Cancer 97, 1488–1498 (2003).
Sondak, V. K. et al. Mitotic rate and younger age are predictors of sentinel lymph node positivity: lessons learned from the generation of a probabilistic model. Ann. Surg. Oncol. 11, 247–258 (2004).
Attis, M. G. & Vollmer, R. T. Mitotic rate in melanoma: a reexamination. Am. J. Clin. Pathol. 127, 380–384 (2007).
Austin, P. F. et al. Age as a prognostic factor in the malignant melanoma population. Ann. Surg. Oncol. 1, 487–494 (1994).
Lasithiotakis, K. et al. Age and gender are significant independent predictors of survival in primary cutaneous melanoma. Cancer 112, 1795–1804 (2008).
Balch, C. M. et al. Long-term results of a prospective surgical trial comparing 2 cm vs 4 cm excision margins for 740 patients with 1–4 mm melanomas. Ann. Surg. Oncol. 8, 101–108 (2001).
Cohn-Cedermark, G. et al. Long term results of a randomized study by the Swedish Melanoma Study Group on 2-cm versus 5-cm resection margins for patients with cutaneous melanoma with a tumor thickness of 0.8–20 mm. Cancer 89, 1495–1501 (2000).
Veronesi, U. et al. Thin stage I primary cutaneous malignant melanoma. Comparison of excision with margins of 1 or 3 cm. N. Engl. J. Med. 318, 1159–1162 (1988).
Morton, D. L. et al. Sentinel-node biopsy or nodal observation in melanoma. N. Engl. J. Med. 355, 1307–1317 (2006).
Grange, F. et al. Variations in management of stage I to stage III cutaneous melanoma: a population-based study of clinical practices in France. Arch. Dermatol. 144, 629–636 (2008).
Cormier, J. N. et al. Population-based assessment of surgical treatment trends for patients with melanoma in the era of sentinel lymph node biopsy. J. Clin. Oncol. 23, 6054–6062 (2005).
Bilimoria, K. Y. et al. Health care system and socioeconomic factors associated with variance in use of sentinel lymph node biopsy for melanoma in the United States. J. Clin. Oncol. 27, 1857–1863 (2009).
Bilimoria, K. Y. et al. Complete lymph node dissection for sentinel node-positive melanoma: assessment of practice patterns in the United States. Ann. Surg. Oncol. 15, 1566–1576 (2008).
Pan, W. R., Suami, H. & Taylor, G. I. Senile changes in human lymph nodes. Lymphat. Res. Biol. 6, 77–94 (2008).
Pawlik, T. M. et al. Predictors and natural history of in-transit melanoma after sentinel lymphadenectomy. Ann. Surg. Oncol. 12, 587–596 (2005).
Conway, W. C. et al. Age-related lymphatic dysfunction in melanoma patients. Ann. Surg. Oncol. 16, 1548–1552 (2009).
Wolff, T., Tai, E. & Miller, T. Screening for skin cancer: an update of the evidence for the U.S. Preventive Services Task Force. Ann. Intern. Med. 150, 194–199 (2009).
Geller, A. C., Miller, D. R., Swetter, S. M., Demierre, M. F. & Gilchrest, B. A. A call for the development and implementation of a targeted national melanoma screening program. Arch. Dermatol. 142, 504–507 (2006).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Tsai, S., Balch, C. & Lange, J. Epidemiology and treatment of melanoma in elderly patients. Nat Rev Clin Oncol 7, 148–152 (2010). https://doi.org/10.1038/nrclinonc.2010.1
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2010.1
This article is cited by
-
Immune checkpoint inhibitor (ICI) genes and aging in malignant melanoma patients: a clinicogenomic TCGA study
BMC Cancer (2022)
-
Ultraviolet light-induced collagen degradation inhibits melanoma invasion
Nature Communications (2021)
-
Melanoma Diagnosis and Treatment in the Elderly
Current Geriatrics Reports (2020)
-
Treatment of elderly patients with melanoma
memo - Magazine of European Medical Oncology (2016)
-
Novel Therapies for Metastatic Melanoma: An Update on Their Use in Older Patients
Drugs & Aging (2015)