Abstract
Background We investigated in a longitudinal, multicenter, cohort study whether combined lipid apheresis and lipid-lowering medication can reduce extremely high levels of lipoprotein(a) (Lp[a]) and thus prevent major adverse coronary events (MACE) more efficaciously than lipid-lowering medication alone.
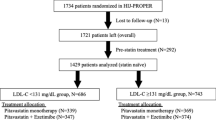
Methods Eligible patients had coronary artery disease and Lp(a) levels ≥2.14 µmol/l (95th percentile). All patients received lipid-lowering medications alone until maximally tolerated doses were no longer effective, followed by combined lipid apheresis and lipid-lowering medication. The rates of the primary outcome, MACE, were recorded for both periods.
Results A total of 120 patients were included. The mean duration of lipid-lowering therapy alone was 5.6±5.8 years, and that of apheresis was 5.0±3.6 years. Median Lp(a) concentration was reduced from 4.00 µmol/l to 1.07 µmol/l with apheresis treatment (P<0.0001); the corresponding mean annual MACE rate per patient was 1.056 versus 0.144 (P<0.0001).
Conclusions Lowering of Lp(a) levels by apheresis was efficacious and safe, and we recommend this therapy for patients in whom maximally tolerated doses of medication alone have failed to control coronary artery disease-associated events.
Key Points
-
The clinical relevance of lipoprotein(a) to atherothrombotic complications has been a matter of diagnostic and therapeutic controversy
-
Our findings provide evidence that lowering concentrations of lipoprotein(a) significantly reduces the rate of major adverse coronary events
-
Application of lipid apheresis—the only currently available method to drastically reduce lipoprotein(a) levels—safely and efficaciously reduced the frequency of myocardial infarction by 97%, irrespective of LDL cholesterol concentrations before therapy
-
Screening for extremely high lipoprotein(a) elevations in patients with premature atherosclerosis, recurrent MACE, or a positive family history for atherosclerosis might be useful to direct therapy
-
Given the inconvenience of apheresis therapy, our findings highlight the need for development of drugs to effectively lower pathogenic lipoprotein(a) concentrations
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Berg K (1963) A new serum type system in man: the Lp system. Acta Pathol Microbiol Scand 59: 369–382
Rifai N et al. (2004) Apolipoprotein(a) size and lipoprotein(a) concentration and future risk of angina pectoris with evidence of severe coronary atherosclerosis in men: the Physicians Health Study. Clin Chem 50: 1364–1371
Bostom AG et al. (1996) Elevated plasma lipoprotein(a) and coronary heart disease in men aged 55 years and younger. A prospective study. JAMA 276: 544–548
Berg K et al. (1997) Lp(a) lipoprotein level predicts survival and major coronary events in the Scandinavian Simvastatin Survival study. Clin Genet 52: 254–261
Kronenberg F et al. (1999) Role of lipoprotein(a) and apolipoprotein(a) phenotype in atherogenesis. Results from the Bruneck study. Circulation 10: 1154–1160
Kostner GM et al. (1981) Lipoprotein Lp(a) and the risk for myocardial infarction. Atherosclerosis 38: 51–61
Cremer P et al. (1994) Lp(a) as predictor of myocardial infarction in comparison to fibrinogen, LDL-cholesterol and other risk factors: results from the prospective Göttingen Risk Incidence and Prevalence Study (GRIPS). Eur J Clin Invest 24: 444–453
Danesh J et al. (2000) Lipoprotein(a) and coronary heart disease, meta-analysis of prospective studies. Circulation 102: 1082–1085
Luc G et al. (2002) Lipoprotein(a) as a predictor of coronary heart disease: the PRIME study. Atherosclerosis 163: 377–384
Utermann G (1989) The mysteries of lipoprotein(a). Science 346: 904–910
Bennett A et al. (2008) Lipoprotein(a) levels and risk of future coronary heart disease. Large-scale prospective data. Arch Intern Med 168: 598–608
Hajjar KA and Nachman R (1996) The role of lipoprotein(a) in atherogenesis and thrombosis. Annu Rev Med 47: 423–442
Strater R et al. (2002) Prospective assessment of risk factors for recurrent stroke during childhood: a 5-year follow-up study. Lancet 360: 1540–1545
Dieplinger B et al. (2007) Increased serum lipoprotein(a) concentrations and low molecular weight phenotypes of apolipoprotein(a) are associated with symptomatic peripheral arterial disease. Clin Chem 53: 1298–1305
von Eckardstein A et al. (2001) Lipoprotein(a) further increases the risk of coronary events in men with high global cardiovascular risk. J Am Coll Cardiol 37: 434–439
Panza F et al. (2007) Lipoproteins, vascular-related genetic factors, and human longevity. Rejuvenation Res 10: 441–458
Thompson GR et al. (1995) The familial hypercholesterolaemia regression study: a randomised trial of low-density-lipoprotein apheresis. Lancet 345: 811–816
Kroon AA et al. (1996) LDL-Apheresis Atherosclerosis Regression Study (LAARS). Effect of aggressive versus conventional lipid lowering treatment on coronary atherosclerosis. Circulation 93: 1826–1835
Maher VM et al. (1995) Effects of lowering elevated LDL cholesterol on the cardiovascular risk of Lp(a). JAMA 274: 1771–1774
Kraft HG et al. (1996) Apolipoprotein(a) kringle IV repeat number predicts risk for coronary heart disease. Arterioscler Thromb Vasc Biol 16: 713–719
Sandholzer C et al. (1992) Apo(a) isoforms predict risk for coronary heart disease. A study in six populations. Arterioscler Thromb 12: 1214–1226
Marcovina SM et al. (2003) Report of the National Heart, Lung and Blood Institute on lipoprotein(a) and cardiovascular disease: recent advances and future directions. Clin Chem 49: 1785–1796
Kostner GM et al. (1993) Preparation of a stable fresh frozen primary lipoprotein[a] (Lp[a]) standard. J Lipid Res 40: 2255–2263
Kronenberg F et al. (2004) Lipoprotein(a)- and low-density-derived cholesterol in nephrotic syndrome: impact on lipid-lowering therapy? Kidney Int 66: 348–354
Kamstrup PR et al. (2008) Extreme lipoprotein(a) levels and the risk of myocardial infarction in the general population: the Copenhagen City Heart Study. Circulation 117: 176–184
Brown BG et al. (2001) Simvastatin and niacin, antioxidant vitamins, or the combination for the prevention of coronary disease. N Engl J Med 345: 1583–1592
Derosa G et al. (2007) Effects of nateglinide and glibenclamide on prothrombotic factors in native type 2 diabetic patients treated with metformin: a 1-year, double-blind, randomized clinical trial. Intern Med 46: 1837–1846
Danik JS et al. (2008) Lipoprotein (a), hormone replacement therapy, and risk of future cardiovascular events. J Am Coll Cardiol 52: 124–131
Straube R and Kingreen H (1998) Lipoprotein(a)-immunapheresis in the treatment of familiar lipoprotein(a) hyperlipoproteinemia in a patient with coronary heart disease. Ther Apher 2: 243–245
Daida GH et al. (1994) Prevention of restenosis after percutaneous transluminal angioplasty by reducing lipoprotein(a) levels with low-density lipoprotein apheresis. Low-Density Lipoprotein Apheresis Angioplasty Restenosis Trial (L-ART) group. Am J Cardiol 73: 1037–1040
Jaeger BR (2003) The HELP system for the treatment of atherothrombotic disorders: a review. Ther Apher Dial 7: 391–396
Beschluss des Bundesausschusses der Ärzte und Krankenkassen vom 24.03.2003 (BUB-Richtlinien). (Reimbursement guidelines of the indication for chronic lipid apheresis by the German Federal Joint Committee as of March 24, 2003.) Dtsch Ärztebl 8: 373–374
Cummins RO et al. (1991) Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Ulstein-style: a statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation 84: 960–975
Smith SC Jr et al. (2006) AHA/ACC Guidelines for secondary prevention for patients with coronary or other atherosclerotic vascular disease: 2006 update. J Am Coll Cardiol 47: 2130–2139
European Patent by Dietrich Seidel: International publication number: WO_2001/048476 (05.07.2001, Gazette 2001/27), International registration number: PCT/EP/00/13294 published 9th March 2005, Patentblatt 2001/1 (EP1 242 825 B1)
Bosch T (1996) State of the art of lipid apheresis. Artif Organs 20: 292–295
Mikrozensus 2005: Fragen zur Gesundheit, Statistisches Bundesamt 2006; chapter: Rauchgewohnheiten der Patienten, page 13. Article number: 5239004059004.
Desmarais RL et al. (1995) Elevated lipoprotein(a) is a risk factor for clinical recurrence after coronary balloon angioplasty. Circulation 91: 1403–1409
Cushing GL et al. (1989) Quantification and localization of apolipoproteins [a] and B in coronary artery bypass vein grafts resected at re-operation. Arteriosclerosis 99: 593–603
Barre DE (2007) The molecular nature and consequences of lipoprotein (a)'s association with platelets. Protein Pept Lett 14: 839–842
Acknowledgements
We would like to dedicate this article to Kåre Berg. We are indebted to the patients for their trust and our families for their advice, encouragement and support. We appreciate the dedicated help of the colleagues and nurses of the participating apheresis centers.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Additional information
The Clinical investigators who participated in the Lipoprotein(a) Study Group are listed in the Supplementary Appendix 1.
Supplementary information
Supplementary Appendix 1
(DOC 24 kb)
Rights and permissions
About this article
Cite this article
Jaeger, B., Richter, Y., Nagel, D. et al. Longitudinal cohort study on the effectiveness of lipid apheresis treatment to reduce high lipoprotein(a) levels and prevent major adverse coronary events. Nat Rev Cardiol 6, 229–239 (2009). https://doi.org/10.1038/ncpcardio1456
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpcardio1456
This article is cited by
-
Lipoprotein apheresis affects the concentration of extracellular vesicles in patients with elevated lipoprotein (a)
Scientific Reports (2024)
-
Lipoproteinapherese
Herz (2022)
-
Therapeutic Apheresis for Management of Lp(a) Hyperlipoproteinemia
Current Atherosclerosis Reports (2020)
-
Lipoprotein(a)—antisense therapy
Clinical Research in Cardiology Supplements (2019)
-
Lipoprotein(a) apheresis in patients with peripheral arterial disease: rationale and clinical results
Clinical Research in Cardiology Supplements (2019)