Abstract
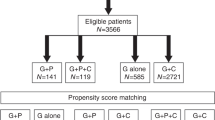
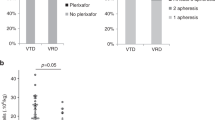
Multiple myeloma is the most common indication for high-dose chemotherapy with autologous stem cell support (ASCT) in North America today. Stem cell procurement for ASCT has most commonly been performed with stem cell mobilization using colony-stimulating factors with or without prior chemotherapy. The target CD34+ cell dose to be collected as well as the number of apheresis performed varies throughout the country, but a minimum of 2 million CD34+ cells/kg has been traditionally used for the support of one cycle of high-dose therapy. With the advent of plerixafor (AMD3100) (a novel stem cell mobilization agent), it is pertinent to review the current status of stem cell mobilization for myeloma as well as the role of autologous stem cell transplantation in this disease. On June 1, 2008, a panel of experts was convened by the International Myeloma Foundation to address issues regarding stem cell mobilization and autologous transplantation in myeloma in the context of new therapies. The panel was asked to discuss a variety of issues regarding stem cell collection and transplantation in myeloma especially with the arrival of plerixafor. Herein, is a summary of their deliberations and conclusions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Pasquini MC, He V, Perez WS . CIBMTR summary slides part 1. CIBMTR Newsletter 2006; 12: 5–7.
Mavroudis D, Read E, Cottler-Fox M, Couriel D, Molldrem J, Carter C et al. CD34+ cell dose predicts survival, posttransplant morbidity, and rate of hematologic recovery after allogeneic marrow transplants for hematologic malignancies. Blood 1996; 88: 3223–3229.
Bittencourt H, Rocha V, Chevret S, Socié G, Espérou H, Devergie A et al. Association of CD34 cell dose with hematopoietic recovery, infections, and other outcomes after HLA-identical sibling bone marrow transplantation. Blood 2002; 99: 2726–2733.
Sierra J, Storer B, Hansen JA, Bjerke JW, Martin PJ, Petersdorf EW et al. Transplantation of marrow cells from unrelated donors for treatment of high-risk acute leukemia: the effect of leukemic burden, donor HLA-matching, and marrow cell dose. Blood 1997; 89: 4226–4235.
Przepiorka D, Smith TL, Folloder J, Khouri I, Ueno NT, Mehra R et al. Risk factors for acute graft-versus-host disease after allogeneic blood stem cell transplantation. Blood 1999; 94: 1465–1470.
Perez-Simon JA, Diez-Campelo M, Martino R, Sureda A, Caballero D, Canizo C et al. Impact of CD34+ cell dose on the outcome of patients undergoing reduced-intensity-conditioning allogeneic peripheral blood stem cell transplantation. Blood 2003; 102: 1108–1113.
Zaucha R, Gooley T, Bensinger WI, Heimfeld S, Chauncey TR, Zaucha R et al. CD34 cell dose in granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear cell grafts affects engraftment kinetics and development of extensive chronic graft-versus-host disease after human leukocyte antigen-identical sibling transplantation. Blood 2001; 98: 3221–3227.
Mohty M, Bilger K, Jourdan E, Kuentz M, Michallet M, Bourhis JH et al. Higher doses of CD34+ peripheral blood stem cells are associated with increased mortality from chronic graft-versus-host disease after allogeneic HLA-identical sibling transplantation. Leukemia 2003; 17: 869–875.
Desikan KR, Tricot G, Munshi NC, Annaissie E, Spoon D, Fassas A et al. Preceding chemotherapy, tumour load and age influence engraftment in multiple myeloma patients mobilized with granulocyte colony-stimulating factor alone. Br J Haematol 2001; 112: 242–247.
Bensinger W, Appelbaum F, Rowley S, Storb R, Sanders J, Lilleby K et al. Factors that influence collection and engraftment of autologous peripheral blood-stem cells. J Clin Oncol 1995; 13: 2547–2555.
Weaver CH, Hazelton B, Birch R, Palmer P, Allen C, Schwartzberg L et al. An analysis of engraftment kinetics as a function of the CD34 content of peripheral blood progenitor cell collections in 692 patients after the administration of myeloablative chemotherapy. Blood 1995; 86: 3961–3969.
Benedetti G, Patoia L, Giglietti A, Alessio M, Pelicci P, Grignani F . Very large amounts of peripheral blood progenitor cell eliminate severe thrombocytopenia after high-dose melphalan in advanced breast cancer patients. Bone Marrow Transplant 1999; 24: 971–979.
Ketterer N, Salles G, Raba M, Espinouse D, Sonet A, Tremisi P et al. High CD34+ cell counts decrease hematologic toxicity of autologous peripheral blood progenitor cell transplantation. Blood 1998; 91: 3148–3155.
Oran B, Malek K, Sanchorawala V, Wright DG, Quillen K, Finn KT et al. Predictive factors for hematopoietic engraftment after autologous peripheral blood stem cell transplantation for AL amyloidosis. Bone Marrow Transplant 2005; 35: 567–575.
Kim DH, Sohn SK, Jeon SB, Baek JH, Kim JG, Lee NY et al. Prognostic significance of platelet recovery pattern after allogeneic HLA-identical sibling transplantation and its association with severe acute GVHD. Bone Marrow Transplant 2006; 37: 101–108.
Bruno B, Gooley T, Sullivan KM, Davis C, Bensinger WI, Storb R et al. Secondary failure of platelet recovery after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2001; 7: 154–162.
Desikan KR, Barlogie B, Jagannath S, Vesole DH, Siegel D, Fassas A et al. Comparable engraftment kinetics following peripheral-blood stem-cell infusion mobilized with granulocyte colony-stimulating factor with or without cyclophosphamide in multiple myeloma. J Clin Oncol 1998; 16: 1547–1553.
Alegre A, Tomás JF, Martínez-Chamorro C, Gil-Fernández JJ, Fernández-Villalta MJ, Arranz R et al. Comparison of peripheral blood progenitor cell mobilization in patients with multiple myeloma: high-dose cyclophosphamide plus GM-CSF vs G-CSF alone. Bone Marrow Transplant 1997; 20: 211–217.
Demirer T, Ayli M, Ozcan M, Gunel N, Haznedar R, Dagli M et al. Mobilization of peripheral blood stem cells with chemotherapy and recombinant human granulocyte colony-stimulating factor (rhG-CSF): a randomized evaluation of different doses of rhG-CSF. Br J Haematol 2002; 116: 468–474.
Arora M, Burns LJ, Barker JN, Miller JS, Defor TE, Olujohungbe AB et al. Randomized comparison of granulocyte colony-stimulating factor versus granulocyte-macrophage colony-stimulating factor plus intensive chemotherapy for peripheral blood stem cell mobilization and autologous transplantation in multiple myeloma. Biol Blood Marrow Transplant 2004; 10: 395–404.
Gojo I, Guo C, Sarkodee-Adoo C, Meisenberg B, Fassas A, Rapoport AP et al. High-dose cyclophosphamide with or without etoposide for mobilization of peripheral blood progenitor cells in patients with multiple myeloma: efficacy and toxicity. Bone Marrow Transplant 2004; 34: 69–76.
Dingli D, Nowakowski GS, Dispenzieri A, Lacy MQ, Hayman S, Litzow MR et al. Cyclophosphamide mobilization does not improve outcome in patients receiving stem cell transplantation for multiple myeloma. Clin Lymphoma Myeloma 2006; 6: 384–388.
Lefrère F, Zohar S, Ghez D, Delarue R, Audat F, Suarez F et al. The VAD chemotherapy regimen plus a G-CSF dose of 10 microg/kg is as effective and less toxic than high-dose cyclophosphamide plus a G-CSF dose of 5 microg/kg for progenitor cell mobilization: results from a monocentric study of 82 patients. Bone Marrow Transplant 2006; 37: 725–729.
Bruns I, Steidl U, Kronenwett R, Fenk R, Graef T, Rohr UP et al. A single dose of 6 or 12 mg of pegfilgrastim for peripheral blood progenitor cell mobilization results in similar yields of CD34+ progenitors in patients with multiple myeloma. Transfusion 2006; 46: 180–185.
Barlogie B, Anaissie E, van Rhee F, Pineda-Roman M, Zangari M, Shaughnessy J et al. The Arkansas approach to therapy of patients with multiple myeloma. Best Pract Res Clin Haematol 2007; 20: 761–781.
Hiwase DK, Bollard G, Hiwase S, Bailey M, Muirhead J, Schwarer AP . Intermediate-dose CY and G-CSF more efficiently mobilize adequate numbers of PBSC for tandem autologous PBSC transplantation compared with low-dose CY in patients with multiple myeloma. Cytotherapy 2007; 9: 539–547.
Zappasodi P, Nosari AM, Astori C, Ciapanna D, Bonfichi M, Varettoni M et al. DCEP chemotherapy followed by a single, fixed dose of pegylated filgrastim allows adequate stem cell mobilization in multiple myeloma patients. Transfusion 2008; 48: 857–860.
Pelus LM . Peripheral blood stem cell mobilization: new regimens, new cells, where do we stand. Curr Opin Hemato 2008; 15: 285–292.
Perea G, Sureda A, Martino R, Altés A, Martínez C, Cabezudo E et al. Predictive factors for a successful mobilization of peripheral blood CD34+ cells in multiple myeloma. Ann Hematol 2001; 80: 592–597.
de la Rubia J, Blade J, Lahuerta JJ, Ribera JM, Martínez R, Alegre A et al. Effect of chemotherapy with alkylating agents on the yield of CD34+ cells in patients with multiple myeloma. Results of the Spanish Myeloma Group (GEM) Study. Haematologica 2006; 91: 621–627.
Kumar S, Dispenzieri A, Lacy MQ, Hayman SR, Fuadi SK, Gastineau DA et al. Impact of lenalidomide therapy on stem cell mobilization and engraftment post-peripheral blood stem cell transplantation in patients with newly diagnosed myeloma. Leukemia 2007; 21: 2035–2042.
Mazumder A, Kaufman J, Niesvizky R, Lonial S, Vesole D, Jagannath S . Effect of lenalidomide therapy on mobilization of peripheral blood stem cells in previously untreated multiple myeloma patients. Leukemia 2007; 22: 1280–1281.
Paripati H, Stewart AK, Cabou S, Dueck A, Zepeda VJ, Pirooz N et al. Compromised stem cell mobilization following induction therapy with lenalidomide in myeloma. Leukemia 2008; 22: 1282–1284.
Mark T, Stern J, Furst J, Jayabalan D, Zafar F, LaRow A et al. Stem cell mobilization with cyclophosphamide overcomes the suppressive effect of lenalidomide therapy on stem cell collection in multiple myeloma. Biol Blood Marrow Transplant 2008; 14: 795–798.
Tricot G, Jagannath S, Vesole D, Nelson J, Tindle S, Miller L et al. Peripheral blood stem cell transplants for multiple myeloma: identification of favorable variables for rapid engraftment in 225 patients. Blood 1995; 85: 588–596.
Palumbo A, Bringhen S, Liberati AM, Caravita T, Falcone A, Callera V et al. Oral melphalan, prednisone, and thalidomide in elderly patients with multiple myeloma: updated results of a randomized, controlled trial. Blood 2008; 112: 3107–3114.
Mateos MV, Hernández JM, Hernández MT, Gutiérrez NC, Palomera L, Fuertes M et al. Bortezomib plus melphalan and prednisone in elderly untreated patients with multiple myeloma: updated time-to-events results and prognostic factors for time to progression. Haematologica 2008; 93: 560–565.
Grignani G, Perissinotto E, Cavalloni G, Carnevale Schianca F, Aglietta M . Clinical use of AMD3100 to mobilize CD34+ cells in patients affected by non-Hodgkin's lymphoma or multiple myeloma. J Clin Oncol 2005; 23: 3871–3872.
Flomenberg N, Devine SM, Dipersio JF, Liesveld JL, McCarty JM, Rowley SD et al. The use of AMD3100 plus G-CSF for autologous hematopoietic progenitor cell mobilization is superior to G-CSF alone. Blood 2005; 106: 1867–1874.
Dipersio JF, Stadtmauer EA, Nademanee AP, Stiff P, Micallef I, Angell J et al. A phase III, multicenter, randomized, double-blind, placebo-controlled, comparative trial of AMD3100 (Perixafor) + G-CSF vs G-CSF + placebo for mobilization in multiple myeloma (MM) patients for autologous hematopoietic stem cell (aHSC) transplantation. Blood 2007; 110 abstract 445, 137a.
Koreth J, Cutler CS, Djulbegovic B, Behl R, Schlossman RL, Munshi NC, Richardson PG et al. High-dose therapy with single autologous transplantation versus chemotherapy for newly diagnosed multiple myeloma: a systematic review and meta-analysis of randomized controlled trials. Biol Blood Marrow Transplant 2007; 3: 183–196.
Attal M, Harousseau JL, Facon T, Guilhot F, Doyen C, Fuzibet JG et al. Single versus double autologous stem-cell transplantation for multiple myeloma. N Engl J Med 2003; 349: 2495–2502.
Cavo M, Tosi P, Zamagni E, Cellini C, Tacchetti P, Patriarca F et al. Prospective, randomized study of single compared with double autologous stem-cell transplantation for multiple myeloma: Bologna 96 clinical study. J Clin Oncol 2007; 25: 2434–2441.
Barlogie B, Tricot GJ, van Rhee F, Angtuaco E, Walker R, Epstein J et al. Long-term outcome results of the first tandem autotransplant trial for multiple myeloma. Br J Haematol 2006; 135: 158–164.
Abdelkafi A, Ladeb S, Torjman L, Othman TB, Lakhal A, Romdhane NB et al. Single autologous stem-cell transplantation followed by maintenance therapy with thalidomide is superior to double autologous transplantation in multiple myeloma: results of a multicenter randomized clinical trial. Blood 2008; 111: 1805–1810.
Mehta J, Tricot G, Jagannath S, Ayers D, Singhal S, Siegel D et al. Salvage autologous or allogeneic transplantation for multiple myeloma refractory to or relapsing after a first-line autograft. Bone Marrow Transplant 1998; 21: 887–892.
Kumar A, Kharfan-Dabaja MA, Glasmacher A, Djulbegovic B . Tandem versus single autologous hematopoietic cell transplantation for the treatment of multiple myeloma: a systematic review and meta-analysis. J Natl Cancer Inst 2009; 21: 100–106.
Mehta J, Singhal S . Current status of autologous hematopoietic stem cell transplantation in myeloma. Bone Marrow Transplant 2008; 42 (Suppl 1): S28–S34.
Garban F, Attal M, Michallet M, Hulin C, Bourhis JH, Yakoub-Agha I et al. Prospective comparison of autologous stem cell transplantation followed by dose-reduced allograft (IFM99-03 trial) with tandem autologous stem cell transplantation (IFM99-04 trial) in high-risk de novo multiple myeloma. Blood 2006; 107: 3474–3480.
Bruno B, Rotta M, Patriarca F, Mordini N, Allione B, Carnevale-Schianca F et al. A comparison of allografting with autografting for newly diagnosed myeloma. N Engl J Med 2007; 356: 1110–1120.
Rosiñol L, Pérez-Simón JA, Sureda A, de la Rubia J, de Arriba F, Lahuerta JJ et al. A prospective PETHEMA study of tandem autologous transplantation versus autograft followed by reduced-intensity conditioning allogeneic transplantation in newly diagnosed multiple myeloma. Blood 2008; 112: 3591–3593.
Schilling G, Hansen T, Shimoni A, Zabelina T, Pérez-Simón JA, Gutierrez NC et al. Impact of genetic abnormalities on survival after allogeneic hematopoietic stem cell transplantation in multiple myeloma. Leukemia 2008; 22: 1250–1255.
Durie BGM, Harousseau JL, Miguel JS, Bladé J, Barlogie B, Anderson K et al. International uniform response criteria for multiple myeloma. Leukemia 2008; 20: 1467–1473.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix
Appendix
International Myeloma Working Group
Rafat Abonour, Indiana University School of Medicine, Indianapolis, IN, USA
Ray Alexanian, MD Anderson, Houston, TX, USA
Kenneth Anderson, DFCI, Boston, MA, USA
Michael Attal, Purpan Hospital, Toulouse, France
Herve Avet-Loiseau, Institute de Biologie, Nantes, France
Ashraf Badros, University of Maryland, Baltimore, MD, USA
Leif Bergsagel, Mayo Clinic Scottsdale, Scottsdale, AZ, USA
Joan Bladé, Hospital Clinica, Barcelona, Spain
Bart Barlogie, M.I.R.T. UAMS Little Rock, AR, USA
Regis Batille, Institute de Biologie, Nantes, France
Meral Beksac, Ankara University, Ankara, Turkey
Andrew Belch, Cross Cancer Institute, Alberta, Canada
Bill Bensinger, Fred Hutchinson Cancer Center, Seattle, WA, USA
Mario Boccadoro, University of Torino, Torino, Italy
Michele Cavo, Universita di Bologna, Bologna, Italy
Wen Ming Chen, MM Research Center of Beijing, Beijing, China
Tony Child, Leeds General Hospital, Leeds, United Kingdom
James Chim, Department of Medicine, Queen Mary Hospital, Hong Kong
Ray Comenzo, Memorial Sloane-Kettering, New York City, NY, USA
John Crowley, Cancer Research and Biostatistics, Seattle, WA, USA
William Dalton, H. Lee Moffitt, Tampa, FL, USA
Faith Davies, Royal Marsden Hospital, London, England
Cármino de Souza, Univeridade de Campinas, Caminas, Brazil
Michel Delforge, University Hospital Gasthuisberg, Leuven, Belgium
Meletios Dimopoulos, Alexandra Hospital, Athens, Greece
Angela Dispenzieri, Mayo Clinic, Rochester, MN, USA
Brian GM Durie, Cedars-Sinai Outpatient Cancer Center, Los Angeles, CA, USA
Hermann Einsele, Universitätsklinik Würzburg, Würzburg, Germany
Thierry Facon, Centre Hospitalier Regional Universitaire de Lille, Lille, France
Dorotea Fantl, Socieded Argentinade Hematolgia, Buenos Aires, Argentina
Jean-Paul Fermand, Hopitaux de Paris, Paris, France
Rafael Fonseca, Mayo Clinic Scottsdale, Scottsdale, AZ, USA
Gosta Gahrton, Karolinska Institute for Medicine, Huddinge, Sweden
Morie Gertz, Mayo Clinic, Rochester, MN, USA
John Gibson, Royal Prince Alfred Hospital, Sydney, Australia
Hartmut Goldschmidt, University Hospital Heidelberg, Heidelberg, Germany
Philip Greipp, Mayo Clinic, Rochester, MN, USA
Roman Hajek, Brno University, Brno, Czech Republic
Izhar Hardan, Tel Aviv University, Tel Aviv, Israel
Jean-Luc Harousseau, Institute de Biologie, Nantes, France
Hiroyuki Hata, Kumamoto University Hospital, Kumamoto, Japan
Yutaka Hattori, Keio University School of Medicine, Tokyo, Japan
Joy Ho, Royal Prince Alfred Hospital, Sydney, Australia
Vania Hungria, Clinica San Germano, Sao Paolo, Brazil
Shinsuke Ida, Nagoya City University Medical School, Nagoya, Japan
Peter Jacobs, Constantiaberg Medi-Clinic, Plumstead, South Africa
Sundar Jagannath, St Vincent's Comprehensive Cancer Center, New York, NY, USA
Hou Jian, Shanghai Chang Zheng Hospital, Shanghai, China
Douglas Joshua, Royal Prince Alfred Hospital, Sydney, Australia
Michio Kawano, Yamaguchi University, Ube, Japan
Nicolaus Kröger, University Hospital Hamburg, Hamburg, Germany
Shaji Kumar, Department of Hematology, Mayo Clinic, MN, USA
Robert Kyle, Department of Laboratory Med. and Pathology, Mayo Clinic, MN, USA
Juan Lahuerta, Grupo Espanol di Mieloma, Hospital Universitario, Madrid, Spain
Jae Hoon Lee, Gachon University Gil Hospital, Incheon, Korea
Xavier LeLeu, Hospital Huriez, CHRU Lille, France
Suzanne Lentzsch, UPMC Cancer Pavillion, Pittsburgh, PA, USA
Henk Lokhorst, University Medical Center Utrecht, Utrecht, The Netherlands
Sagar Lonial, Emory University School of Medicine, Atlanta, GA, USA
Heinz Ludwig, Wilhelminenspital Der Stat Wien, Vienna, Austria
Angelo Maiolino, Rua fonte da Saudade, Rio de Janeiro, Brazil
María-Victoria Mateos, University Hospital of Salamanca, Spain
Jayesh Mehta, Northwestern University, Chicago, IL, USA
GianPaolo Merlini, University of Pavia, Pavia, Italy
Joseph Mikhael, Mayo Clinic, Scottsdale, AZ, USA
Philippe Moreau, University Hospital, Nantes, France
Gareth Morgan, Royal Marsden Hospital, London, England
Nikhil Munshi, Diane Farber Cancer Institute, Boston, MA, USA
Yana Novis, Hospital SírioLibanês, Bela Vista, Brazil
Amara Nouel, Hospital Rutz y Paez, Bolivar, Venezuela
Robert Orlowski, MD Anderson, Houston, TX, USA
Antonio Palumbo, Cathedra Ematologia, Torino, Italy
Santiago Pavlovsky, Fundaleu, Buenos Aires, Argentina
Linda Pilarski, University of Alberta, Alberta, Canada
Raymond Powles, Leukaemia and Myeloma, Wimbledon, England
Ruben Niesvizky, Weill Medical College of Cornell University, New York, NY, USA
S Vincent Rajkumar, Mayo Clinic, Rochester, MN, USA
Donna Reece, Princess Margaret, Toronto, Canada
Tony Reiman, Cross Cancer Institute, Alberta, Canada
Paul Richardson, Dana Farber Cancer Institute, Boston, MA, USA
Angelina Rodriquez Morales, Bonco Metro Politano de Sangre, Caracas, Venezuela
Orhan Sezer, Department of Hem/Onc, Universitatsklinikum Charite, Berlin, Germany
John Shaughnessy, M.I.R.T. UAMS, Little Rock, AR, USA
Kazuyuki Shimizu, Nagoya City Midori General Hospital, Nagoya, Japan
David Siegel, Hackensack, Cancer Center, Hackensack, NJ, USA
Jesus San Miguel, University of Salamanca, Salamanca, Spain
Chaim Shustik, McGill, Toronto, Canada
Seema Singhal, Northwestern University, Chicago, IL, USA
Pieter Sonneveld, Erasmus MC, Rotterdam, The Netherlands
Andrew Spencer, The Alfred Hospital, Melbourne, Australia
Edward Stadtmauer, University of Pennsylvania, Philadelphia, PA, USA
Keith Stewart, Mayo Clinic Scottsdale, Scottsdale, AZ, USA
Patrizia Tosi, Italian Cooperative Group, Istituto di Ematologia Seragnoli, Bologna, Italy
Guido Tricot, Huntsman Cancer Institute, Salt Lake City, UT, USA
Ingemar Turesson, Department of Hematology, Malmo University, Malmo, Sweden
Brian Van Ness, University of Minnesota, Minneapolis, MN, USA
Ivan Van Riet, Brussels Vrija University, Brussels, Belgium
Robert Vescio, Cedars-Sinai Outpatient Cancer Center, Los Angeles, CA, USA
David Vesole, Loyola University Chicago, IL, USA
Anders Waage, University Hospital, Trondheim, Norway NSMG
Michael Wang, M.D. Anderson, Houston, TX, USA
Donna Weber, MD Anderson, Houston, TX, USA
Jan Westin, Sahlgrenska University Hospital, Gothenburg, Sweden
Keith Wheatley, University of Birmingham, Birmingham, United Kingdom
Dina B Yehuda, Department of Hematology, Hadassah University Hospital, Hadassah, Israel
Jeffrey Zonder, SWOG, Department of Hem/Onc, Karmanos Cancer Institute, MI, USA
Rights and permissions
About this article
Cite this article
Giralt, S., Stadtmauer, E., Harousseau, J. et al. International myeloma working group (IMWG) consensus statement and guidelines regarding the current status of stem cell collection and high-dose therapy for multiple myeloma and the role of plerixafor (AMD 3100). Leukemia 23, 1904–1912 (2009). https://doi.org/10.1038/leu.2009.127
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2009.127
Keywords
This article is cited by
-
Are haematopoietic stem cell transplants stem cell transplants, is there a threshold dose of CD34-positive cells and how many are needed for rapid posttransplant granulocyte recovery?
Leukemia (2023)
-
Bridging advanced myeloma patients to subsequent treatments and clinical trials with classical chemotherapy and stem cell support
Bone Marrow Transplantation (2023)
-
Effectiveness of biosimilar pegfilgrastim in patients with multiple myeloma after high-dose melphalan and autologous stem cell transplantation
Annals of Hematology (2023)
-
Stem cell mobilization in multiple myeloma: challenges, strategies, and current developments
Annals of Hematology (2023)
-
Carfilzomib, lenalidomide and dexamethasone followed by a second ASCT is an effective strategy in first relapse multiple myeloma: a study on behalf of the Chronic malignancies working party of the EBMT
Bone Marrow Transplantation (2023)