Abstract
Purpose
To evaluate the resolution time and the recurrence rate of acute central serous chorioretinopathy (CSC) after spontaneous resolution and low-fluence photodynamic therapy (PDT).
Methods
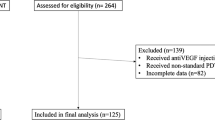
Case–control study: The CSC patients who were admitted to our clinic for the first time were included. No treatment was given during the first 6 months. Patients were treated with PDT after 6 months from the initial signs of the disease, if they did not show any sign of resolution. The patients who showed a significant decrease in subretinal fluid after month 6 were not scheduled for PDT. The primary outcomes were the resolution time and the recurrence rate after the first episode. Secondary outcome measures were the change in BCVA and CRT during the follow up.
Results
A total of 77 consecutive eyes of 77 patients were included, 41 eyes (53.2%) with spontaneously resolved CSC and 36 eyes (46.8%) with PDT-treated CSC. The initial resolution time was 4.1±3.2 months in spontaneous resolution group, and 8.1±0.8 months in PDT group, respectively (P<0.001). The recurrence rate was 51.2% in spontaneous resolution group, and 25% in PDT group (P=0.01). The change in BCVA from baseline to the last follow-up visit was statistically significant in both groups (P=0.002, P=0.003, respectively). The change in CRT from baseline to the last follow up was also statistically significant in both groups (P=0.002, P=0.003, respectively).
Conclusions
The recurrence rate of acute CSC was lower in PDT-treated patients than the spontaneously resolved patients.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSC) is a common macular disease, which is characterized by serous retinal detachment and sometimes associated with retinal pigment epithelium (RPE) detachment.1, 2 Two theories have been proposed regarding the pathophysiology of CSC, which were based either on choroidal or RPE dysfunction, respectively. Although RPE dysfunction theory has yielded more attention for several years, choroidal thickness theory has become more important after the results of indocyanine green angiography (ICGA) and the enhanced depth imaging optical coherence tomography (OCT) studies.3, 4, 5 In CSC patients, choroidal vascular abnormalities and leakage were shown via ICGA, and subfoveal choroidal thickness was found to be thicker via enhanced depth imaging OCT, two essential findings which further supported the role of choroidal dysfunction in the pathogenesis.3, 4, 5 Taking into account the importance of a normal functioning RPE which quickly absorbs the subretinal fluid (SRF), it is not possible to completely reject the RPE theory. Besides, several RPE abnormalities have been described in CSC patients.6
CSC is usually a self-limited condition, which spontaneously resolves within 4–6 months, therefore observation is preferred instead of treatment during the first month of onset. If the serous retinal detachment persists after the first 6 months or recurrence is detected after the resolution of the first episode, treatment options such as laser photocoagulation and photodynamic therapy have to be considered.7 Photodynamic therapy was first introduced for the treatment of neovascular age-related macular degeneration and it was no longer used after the introduction of the anti-vascular endothelial growth factor agents into the market because of its side effects such as choroidal atrophy.8 However, PDT was found to be an effective treatment option in polypoidal choroidal vasculopathy and CSC, which were recently classified as pachychoroid pigment epitheliopathies.9 As a general characteristic, the choroidal thickness was shown to be increased in pachychoroid pigment epitheliopathies.3, 4, 5, 6, 7, 9
It is well known that photodynamic therapy targets primarily the choroid. The choroidal leakage and thickness were shown to be decreased after PDT in patients with polypoidal choroidal vasculopathy and CSC.5, 10 Kang and Kim11 reported that the subfoveal choroidal thickness was decreased in both spontaneously resolved and PDT-treated CSC patients. However, the amount of decrease was higher in PDT-treated patients. The recurrence rate of CSC was underestimated for several years; however, it is now supposed to be around 50%, which is quite high.12 In the light of these findings, we aimed to compare the recurrence rate and resolution time between the spontaneously resolved and PDT-treated CSC patients after their first episode.
Materials and methods
We reviewed the medical records of the patients with the diagnosis of acute CSC who were admitted to our clinic for the first time between January 2012 and December 2013. The study adhered to the tenets of the Declaration of Helsinki. A written informed consent was obtained from all patients before the PDT, if applied. The patients who were diagnosed as acute CSC, and who suffered from the first episode of the disease, and had a minimum follow up time of 12 months after the complete resolution of the first episode were included in the study. The patients who had another retinal disease, such as diabetic retinopathy, or retinal vein occlusion, or were diagnosed as chronic CSC, or were diagnosed as CSC secondary to corticosteroid treatment were not included.
Data collected from the patients’ records included age, gender, best corrected visual acuity (BCVA), central retinal thickness (CRT), complete resolution time of SRF, and recurrence rate after complete recovery.
All patients underwent a standardized examination including measurement of BCVA via the Early Treatment Diabetic Retinopathy Study chart at 4 m slit-lamp biomicroscopy, measurement of IOP via applanation tonometry and biomicroscopic fundus examination. Fundus photography, fluorescein angiography (FA), ICGA (HRA-2; Heidelberg Engineering, Heidelberg, Germany), and OCT imaging (Spectralis; Heidelberg Engineering, Heidelberg, Germany) were performed. All examinations were repeated monthly, except for FA and ICGA. OCT was used to detect SRF and measure CRT. CRT, defined as the mean thickness of the neurosensory retina in a central 1 mm diameter area, was computed using OCT mapping software generated by the device. Acute CSC was diagnosed using FA, ICGA, and OCT in the light of previously reported findings.13
No treatment was given to the patients during the first 6 months. The patients were treated with PDT after a minimum time of 6 months from the initial signs of the disease, if they did not show any sign of resolution or if any increase was detected in SRF. The patients who showed decreased fluid (at least 50% decrease in SRF via eye examination of the OCT) after month 6 and/or showed functional improvement (at least one logarithm of the minimum angle of resolution (LogMAR) line of visual gain) were not scheduled for PDT and called for follow-up visits until the disease was totally resolved.
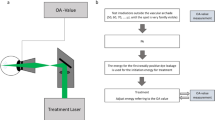
For the PDT procedure, a 689 nm laser system (Carl Zeiss, Dublin, CA, USA) with an indirect lens (Volk Area Centralis Lens; Volk Optical Inc, Mentor, OH, USA) was used. All patients underwent a modified fluence PDT with reduced total light energy (25 J/cm2) and laser intensity (300 mW/cm2) using the standard dose of verteporfin (Visudyne; Novartis AG, Basel, Switzerland) (6 mg/m2) and standard time of laser emission (83 s). The PDT was applied to the dilated choroidal vessels and choroidal vascular abnormality areas, which were detected via ICGA. The PDT spot size was equal to the size of the lesion in order to cover the entire lesion, and determined by measuring the greatest linear dimension of the area of choroidal vascular abnormality on ICGA with a device generated software tool. If there were multiple distinct lesions, each were measured and treated separately during the same PDT session.
Primary outcome measures were the time of the resolution and the recurrence rate after the resolution of the first episode in the spontaneously resolved and PDT-treated acute CSC patients. Secondary outcome measures were the change in BCVA and CRT in the two groups.
Statistical analysis
Visual acuity was converted to the LogMAR for statistical analysis. Categorical variables were presented as numbers and percentages, whereas numerical variables were expressed as the mean and standard deviation. Categorical variables were analyzed using the χ2 test. The Wilcoxon’s rank test was used to compare variables at baseline and after treatment. The Mann–Whitney U-test was used to compare variables between the two groups. The statistical evaluation was performed using SPSS (Version 20.0, SPSS Inc., Chicago, IL, USA). A P value of <0.05 was considered to be statistically significant.
Results
A total of 77 eyes of 77 patients with the diagnosis of acute CSC met the inclusion criteria and were included in the study. The mean age of the patients was 44.2±9.2 years (range, 31–64 years). Sixteen patients (20.8%) were female, 61 patients (79.2%) were male. Spontaneously resolved group comprised of 41 (53.2%) patients, and PDT group comprised of 36 (46.8%) patients. Analysis of the demographic data consisting of sex, age, and symptom duration revealed no significant difference between the two groups (P>0.05 for all). The baseline LogMAR BCVA and CRT were not significantly different between the two groups (P=0.3 and P=0.8, respectively). The baseline FA showed ink-blot or smoke-stack pattern of hyperfluorescence in all of the eyes. In the spontaneously resolved group, 29 eyes (70.7%) showed a single leakage point and 12 eyes (29.3%) showed multifocal leakage points. In the PDT-treated group, 23 eyes (63.9%) showed a single leakage point, and 13 eyes (36.1%) showed multifocal leakage points. There was not a significant difference between the two groups in regard to the leakage patterns (P=0.4). FA was repeated and ICGA was obtained from the patients who were in the PDT group before the treatment. Four of the eyes (11.1%) showed new diffuse leakage areas in addition to the previous focal leakage areas and six eyes (16.6%) showed transmission defects in FA, and all of the eyes showed dilated choroidal vessels and choroidal vascular hyperpermeability in the mid-phase of ICGA. The general characteristics of the two groups were summarized in Table 1.
Resolution of SRF
The mean resolution time from baseline to initial complete resolution of SRF was significantly shorter in spontaneously resolved group than in PDT group (4.1 vs 8.1 months, P<0.001). In spontaneously resolved group, complete resolution of SRF on OCT was observed in 11 of 41 eyes (26.9%) at month 1, and SRF resolved completely in the remaining 9 eyes (21.9%) between month 1 and 3, 12 eyes (29.3%) between month 3 and 6, and 9 eyes (21.9%) between month 6 and 11. PDT was performed between month 6 and 9 (mean, 6.8±0.82 months) after the first admission to the clinic. In PDT group, complete resolution of SRF was achieved in 15 of 36 eyes (41.6%) at month 7, and in 21 eyes (58.4%) between month 7 and 12. In PDT group, SRF resolved within 1–4 months after PDT (mean 1.3±0.8 months). After the complete resolution of the first episode of CSC, 21 (51.2%) eyes in spontaneously resolved group and 9 (25%) eyes in PDT group showed a recurrence of SRF (P=0.01). The mean recurrence time was 6.3±4.0 months in spontaneously resolved eyes, and 7.8±4.8 months in PDT-treated eyes (P=0.3).
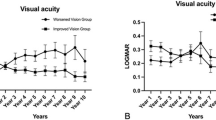
Visual acuity
Mean LogMAR BCVA changes in both groups are shown in Figure 1. Comparison of the two groups revealed no statistically significant difference in BCVA improvement at the last visit (P=0.12). The mean baseline LogMAR BCVA increased significantly from 0.16±0.19 (range, 0.0–0.7) to 0.08±0.1 (range, 0.0–0.4) at the last visit in the spontaneously resolved group and from 0.17±0.1 (range, 0.0–0.4) to 0.11±0.1 (range, 0.0–0.4) in the PDT group, respectively (P=0.002 and P=0.003, respectively).
The mean baseline visual acuity of the patients who showed recurrence in the spontaneously resolved (21 eyes) and PDT group (9 eyes) was 0.25±0.22 (range, 0.0–0.7) and 0.19±0.09 LogMAR (range 0.0–0.3) (P=0.6). The mean visual acuity of the eyes in the spontaneously resolved group at the time of complete recovery was 0.11±0.10 LogMAR (range, 0.0–0.4) and 0.23±0.22 LogMAR (range, 0.0–1.0) at the time of recurrence (P=0.01). The mean visual acuity of the eyes in the PDT-treated group at the time of complete recovery was 0.07±0.07 LogMAR (range, 0.0–0.2) and 0.30±0.23 LogMAR (range, 0.0–1.0) at the time of recurrence (P=0.03) (Table 2).
Central retinal thickness
The mean CRT changes from baseline to the last visit in both groups are shown in Figure 2. Comparison of the two groups revealed no statistically significant difference in CRT change at the last visit (P=0.78). The mean baseline CRT decreased significantly from 375±130 μm (range, 184–772 μm) to 230±38 μm (range, 142–314 μm) at the last visit in the spontaneously resolved group and from 364±82 μm (range, 237–514 μm) to 231±36 μm (range, 0.0–0.4) in PDT group (P=0.002 and P=0.003, respectively).
The mean baseline CRT of the patients who showed recurrence in the spontaneously resolved (21 eyes) and PDT group (9 eyes) was 403±161 μm (range, 184–772 μm) and 382±81 μm (range, 294–509 μm) (P=0.7). The mean CRT of the eyes in the spontaneously resolved group at the time of complete recovery was 222±43 μm (range, 142–314 μm) and 319±123 μm (range, 184–672 μm) at the time of recurrence (P=0.003). The mean CRT of the eyes in the PDT-treated group at the time of complete recovery was 238±52 μm (range, 157–348 μm) and 329±68 μm (range, 228–428 μm) at the time of recurrence (P=0.01) (Table 3).
Discussion
In the present study, we compared the resolution time of SRF and the recurrence rate after the initial resolution of SRF in acute CSC patients who either resolved spontaneously or were treated with half-fluence PDT. Changes in BCVA and CRT during the follow up were also examined. The results of this study showed that PDT was more effective than observation alone in decreasing the recurrence rate after complete resolution of SRF in the first episode of acute CSC. However, the mean resolution time which was calculated from the first admission to the initial complete resolution of SRF was shorter in spontaneously resolved patients; an issue probably due to our study design. We waited at least 6 months for the treatment, and during this period most of the patients recovered spontaneously. We assume that the patients who underwent PDT were those who might have more serious clinical courses. Although the PDT-treated patients had such a drawback, the two groups seemed to be equivalent in terms of clinical outcomes and showed significant improvements in vision and reductions in CRT. Also PDT treatment was associated with a significant reduction in recurrence rate.
CSC has been classified as acute or chronic, according to the duration of symptoms. Acute CSC is a self-limited disease and SRF usually resolves spontaneously within 3–4 months after the beginning of symptoms.14 Recurrence rate reported in the literature differs largely because of the heterogeneity of follow-up periods within studies. Hence, recurrence rate of acute CSC was reported to vary between 15 and 50% in spontaneously resolved patients.7 Accordingly, in our study, the recurrence rate in spontaneously resolved patients was 51% during the mean follow-up time of 21.8 months.
There is a consensus among the authors that the first-line approach for acute CSC is observation. However, optimal timing for intervention and the most suitable treatment option are still in debate in recurrent CSC patients. In CSC, PDT with verteporfin has been shown to be an effective treatment modality in reducing choroidal thickness, vascular hyperpermeability, and extravascular leakage by provoking hypoperfusion of the choriocapillaris and choroidal vascular remodeling.15 Half-fluence PDT is as effective as standard-fluence PDT and may have the advantage of causing lower amount of choroidal hypoxia and nonperfusion over the standard-fluence PDT.16 A study by Kang and Kim11 evaluating the choroidal thickness changes in spontaneously resolved CSC patients, and in patients treated with half-fluence PDT revealed that the mean choroidal thickness of CSC patients following PDT was similar to the healthy controls. However, in spontaneously resolved CSC patients, the decrease in choroidal thickness was not as much as the PDT-treated patients. They suggested that the healing mechanism of PDT might be different from the spontaneous resolution and thinning of the choroid may have a role on this phenomenon. This might be an explanation for the lower recurrence rate detected in patients with CSC who underwent PDT (25%) vs spontaneously resolved patients (51%) in our study.
Recurrence rate after PDT varies from 3 to 24% in the literature.17 The recurrence rate in our study (25%) was comparable with the previously reported rates. Indeed, the resolution of SRF often leads to an improvement in visual acuity in the majority of the patients with CSC after PDT. In the study by Kim et al,18 the patients with incomplete SRF resorption or SRF recurrence had a worse visual acuity than those with complete SRF resolution or without recurrence after PDT. Duration of symptoms, initial BCVA, and integrity of the foveal IS/OS line were reported to be related to final visual outcomes in previous studies.19, 20, 21 There is also emerging evidence that early resolution of SRF could reduce the risk of photoreceptor/RPE degeneration and improve visual acuity.22 However, in our study, despite the shorter resolution time in spontaneously resolved group, no difference was found between the groups in respect to the visual acuity changes during follow up. One possible reason for this non-significance may be the relative shorter recovery time in PDT-treated patients. Although none of the PDT-treated patients recovered within 6 months of onset, all of them responded very well to the PDT treatment and majority of them showed complete resolution of SRF after only 1 month from the initiation of treatment. Kim et al18 showed that the majority of patients with CSC showed a recurrence within 2 years. In our study, the mean recurrence time was 6.3±4.0 months in spontaneously resolved eyes and 7.8±4.8 months in PDT-treated eyes.
The present study has some limitations. The most important limitation is its retrospective design. Also as per study design and taking into consideration our clinical approach which was based on observation, we might have created a bias in favor of the spontaneous resolved eyes in terms of visual and anatomical outcomes. It is important to note here that this group of patients has a natural good prognosis in comparison to PDT-treated group, and their resolution time is expected to be shorter. Although the PDT-treated eyes had a disadvantage of ‘waiting with SRF’ for a longer time period than the spontaneous resolution group, PDT-treated group showed a significantly lower recurrence rate, which may underscore the effect of PDT on recurrence. And most importantly, our study consisted of a relatively good number of patients with a long mean follow-up period.
In conclusion, half-fluence PDT may reduce the recurrence rate in patients with acute CSC. However, recurrence may still occur in up to a quarter of eyes after PDT. The results of visual and anatomical outcomes are comparable between the two groups. Decreasing the recurrences with PDT may have a positive effect on visual acuity in the long-term. Although further studies are needed to prove our findings, it seems appropriate to recommend PDT in patients with prolonged history of acute CSC in order to hasten resolution of SRF and decrease recurrence rates.

References
Klais CM, Ober MD, Ciardella AP, Yannuzzi LA. Central serous chorioretinopathy. In: Ryan SJ (ed)Retina. Vol 2 Elsevier Mosby: Philadelphia, 2006, pp 1135–1161.
Lehmann M, Wolff B, Vasseur V, Martinet V, Manasseh N, Sahel JA et al. Retinal and choroidal changes observed with ‘En face’ enhanced-depth imaging OCT in central serous chorioretinopathy. Br J Ophthalmol 2013; 97: 1181–1186.
Prünte C, Flammer J . Choroidal capillary and venous congestion in central serous chorioretinopathy. Am J Ophthalmol 1996; 121: 26–34.
Hirami Y, Tsujikawa A, Sasahara M, Gotoh N, Tamura H, Otani A et al. Alterations of retinal pigment epithelium in central serous chorioretinopathy. Clin Experiment Ophthalmol 2007; 35: 225–230.
Alkin Z, Ozkaya A, Agca A, Yazici AT, Demirok A . Early visual and morphologic changes after half-fluence photodynamic therapy in chronic central serous chorioretinopathy. J Ocul Pharmacol Ther 2014; 30: 359–365.
Kim HC, Cho WB, Chung H . Morphologic changes in acute central serous chorioretinopathy using spectral domain optical coherence tomography. Korean J Ophthalmol 2012; 26: 347–354.
Daruich A, Matet A, Dirani A, Bousquet E, Zhao M, Farman N et al. Central serous chorioretinopathy: recent findings and new physiopathology hypothesis. Prog Retin Eye Res 2015; 48: 82–118.
Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials–TAP report. Treatment of age-related macular degeneration with photodynamic therapy (TAP) Study. Arch Ophthalmol 1999; 117: 1329–1345.
Warrow DJ, Hoang QV, Freund KB . Pachychoroid pigment epitheliopathy. Retina 2013; 33: 1659–1672.
Quaranta M, Mauget-Faÿsse M, Coscas G . Exudative idiopathic polypoidal choroidal vasculopathy and photodynamic therapy with verteporfin. Am J Ophthalmol 2002; 134: 277–280.
Kang NH, Kim YT . Change in subfoveal choroidal thickness in central serous chorioretinopathy following spontaneous resolution and low-fluence photodynamic therapy. Eye 2013; 27: 387–391.
Fok AC, Chan PP, Lam DS, Lai TY . Risk factors for recurrence of serous macular detachment in untreated patients with central serous chorioretinopathy. Ophthalmic Res 2011; 46: 160–163.
Liegl R, Ulbig MW . Central serous chorioretinopathy. Ophthalmologica 2014; 232: 65–76.
Baran NV, Gürlü VP, Esgin H . Long-term macular function in eyes with central serous chorioretinopathy. Clin Experiment Ophthalmol 2005; 33: 369–372.
Karim SP, Adelman RA . Profile of verteporfin and its potential for the treatment of central serous chorioretinopathy. Clin Ophthalmol 2013; 7: 1867–1875.
Reibaldi M, Cardascia N, Longo A, Furino C, Avitabile T, Faro S et al. Standard-fluence versus low-fluence photodynamic therapy in chronic central serous chorioretinopathy: a nonrandomized clinical trial. Am J Ophthalmol 2010; 149: 307–315.
Erikitola OC, Crosby-Nwaobi R, Lotery AJ, Sivaprasad S . Photodynamic therapy for central serous chorioretinopathy. Eye 2014; 28: 944–957.
Kim YK, Ryoo NK, Woo SJ, Park KH . Choroidal thickness changes after photodynamic therapy and recurrence of chronic central serous chorioretinopathy. Am J Ophthalmol 2015; 160 (1): 72–84.e1.
Karakus SH, Basarir B, Pinarci EY, Kirandi EU, Demirok A . Long-term results of half-dose photodynamic therapy for chronic central serous chorioretinopathy with contrast sensitivity changes. Eye 2013; 27: 612–620.
Lim JI, Glassman AR, Aiello LP, Chakravarthy U, Flaxel CJ, Spaide RF et al. Collaborative retrospective macula society study of photodynamic therapy for chronic central serous chorioretinopathy. Ophthalmology 2014; 121: 1073–1078.
Fujita K, Shinoda K, Imamura Y, Matsumoto CS, Mizutani Y, Mizota A et al. Correlation of integrity of cone outer segment tips line with retinal sensitivity after half-dose photodynamic therapy for chronic central serous chorioretinopathy. Am J Ophthalmol 2012; 154: 579–585.
Park SU, Lee SJ, Kim M . Intravitreal anti-vascular endothelial growth factor versus observation in acute central serous chorioretinopathy: one-year results. Korean J Ophthalmol 2014; 28: 306–313.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions
Involved in design and conduct of the study: AO, ZA, MO, ATY, MT; preparation and review of the study: AO, ZA, ATY, MT; data collection: AO, MO; and statistical analysis (AO, ZA).
Rights and permissions
About this article
Cite this article
Ozkaya, A., Alkin, Z., Ozveren, M. et al. The time of resolution and the rate of recurrence in acute central serous chorioretinopathy following spontaneous resolution and low-fluence photodynamic therapy: a case–control study. Eye 30, 1005–1010 (2016). https://doi.org/10.1038/eye.2016.79
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.79
This article is cited by
-
Central serous chorioretinopathy: updates in the pathogenesis, diagnosis and therapeutic strategies
Eye and Vision (2023)
-
OCT biomarkers related to subthreshold micropulse laser treatment effect in central serous chorioretinopathy
BMC Ophthalmology (2022)
-
Subthreshold micropulse laser photocoagulation versus half-dose photodynamic therapy for acute central serous chorioretinopathy
BMC Ophthalmology (2022)
-
Long-term follow-up of half-fluence photodynamic therapy in acute central serous chorioretinopathy
Spektrum der Augenheilkunde (2018)
-
The comparison of multimodal imaging findings of central serous chorioretinopathy patients in regard to the early anatomically treatment response to half-fluence photodynamic therapy: a retrospective case–control study
International Journal of Retina and Vitreous (2017)