Abstract
Background:
Recent studies have demonstrated that microRNAs (miRNAs) are stably detectable in blood and can serve as useful biomarkers for cancer.
Methods:
We performed an miRNA array using serum samples obtained from oesophageal squamous cell carcinoma (ESCC) patients or healthy controls. MiR-1246 was the most markedly elevated in ESCC patients. Therefore, miR-1246 was selected as a candidate for further analysis. The serum miR-1246 level in 46 healthy controls and 101 ESCC patients was evaluated and compared among various clinicopathological characteristics. MiR-1246 expressions in tissue, exosomal, and cellular samples were also examined.
Results:
Serum miR-1246 alone yielded an receiver-operating characteristic curve area of 0.754, with 71.3% sensitivity and 73.9% specificity for distinguishing ESCC patients from healthy controls. Serum miR-1246 was significantly correlated with the TNM stage and showed to be the strongest independent risk factor for poor survival (HR, 4.032; P=0.017). Unlike the tendency shown in previous reports, miR-1246 was not upregulated in ESCC tissue samples. Furthermore, exosomal miR-1246 did not reflect the abundance in the cell of origin.
Conclusion:
These data support our contention that serum miR-1246 has strong potential as a novel diagnostic and prognostic biomarker in ESCC, and its releasing mechanism is selective and independent of tissue miRNA abundance.
Similar content being viewed by others
Main
Oesophageal squamous cell carcinoma (ESCC) has one of the worst prognoses of any cancer, and has an overall 5-year survival rate of about 25–30% (Yuequan et al, 2010; Chen et al, 2012). Recently, improvements in diagnostic modalities and the development of treatments using a combination of surgery, radiation, and/or chemotherapy have improved the prognosis of ESCC patients (Tachimori et al, 2009; Barber et al, 2012). However, because of the absence of typical symptoms or signs, and the lack of a sufficiently sensitive and specific biomarker, ESCC is still often diagnosed at an advanced stage. Therefore, novel biomarkers for the early detection of primary ESCC, as well as its metastasis and recurrence, are urgently needed to reduce disease morbidity and mortality.
MicroRNA (miRNA) is a class of small (21–25 nucleotides) noncoding RNAs that negatively regulate target genes by translational repression or degradation of the complementary mRNA(s) (Ambros, 2004; Bartel, 2004). MiRNAs have important regulatory roles in cell growth, proliferation, differentiation, and death (Ambros, 2004; Bartel, 2004; He and Hannon, 2004; Schickel et al, 2008). The aberrant expression of miRNAs, which has been demonstrated in various types of malignancies, contributes to carcinogenesis and cancer development (Calin et al, 2005; He et al, 2005; Lu et al, 2005; Volinia et al, 2006). Growing evidence has indicated that unique miRNA expression profiles in tissues for each cancer type may contribute to the diagnosis of malignancies and prediction of prognosis (Iorio et al, 2005; Yanaihara et al, 2006). Recently, it was revealed that miRNAs circulate in a cell-free form in the blood (Chim et al, 2008; Hunter et al, 2008; Mitchell et al, 2008), and several studies have demonstrated the diagnostic and prognostic utility of circulating miRNA in cancer patients (Chen et al, 2008; Gilad et al, 2008; Mitchell et al, 2008; Taylor and Gercel-Taylor, 2008; Ji et al, 2009; Resnick et al, 2009; Wang et al, 2009; Ho et al, 2010). However, to date, there have been few reports on the role of circulating miRNAs in the serum of patients with ESCC, and the mechanism of miRNA release into the blood is not clearly understood.
In this study, we investigated whether the concentration of serum miRNAs could be used as diagnostic and prognostic biomarkers for cancer by comparing findings in ESCC patients and healthy controls and by monitoring tumour dynamics. Subsequently, we discussed the existence of the potential function of circulating miRNA independent of tissue miRNA abundance.
Material and methods
Patients and samples
Venous blood samples were collected from 101 ESCC patients and 46 normal control individuals at the Chiba University Hospital, between 2010 and 2012. These samples were collected before any therapeutic procedures, including surgery, chemotherapy, and radiotherapy. Postoperative samples from seven patients were obtained 1 month after oesophagectomy. Serum samples were then stored at −80 °C until further processing. Written consent for sample donation for research purposes was obtained from each patient before sample collection. The protocol was approved by the Institutional Review Board of Chiba University. Tissue samples were obtained from patients who underwent surgery at Chiba University Hospital between 2003 and 2012. Twenty-two pairs of primary ESCC and corresponding normal oesophageal epithelia were obtained. Lymph node samples were collected from four patients with no metastasis during surgery, to use as lymph node dissection tissue. The specimens were snap-frozen in liquid nitrogen and stored at −80 °C until they were analysed.
Cell lines and cell culture
The human ESCC cell lines, TE1, TE2, TE4, TE6, and TE11 were obtained from Tohoku University (Sendai, Japan), and the human fibroblast cell lines, WI38 and MRC5, were obtained from the European Collection of Cell Cultures (Wiltshire, UK). All cell lines were cultured in Dulbecco’s modified Eagle’s medium nutrient mixture (Life Technologies, Grand Island, NY, USA) supplemented with 10% fetal bovine serum in a humidified atmosphere containing 5% CO2 at 37 °C.
Isolation of exosomes from culture supernatants
All cell lines were plated onto collagen-coated 10-cm dishes at a concentration of 1 × 106 cells/dish using each of the media described above. After 48 h, the culture media were collected and sequential centrifugations were performed. Cell culture media were centrifuged at 300 g for 10 min at 4 °C, then these supernatants were centrifuged at 2000 g for 30 min at 4 °C to remove intact cells and cell debris. These supernatants were then passed through a 0.22-μm filter. The filtrates were ultracentrifuged at 100 000 g for 90 min at 4 °C to collect exosomes, using an Optima TLX Ultracentrifuge (Beckman Coulter, Brea, CA, USA). Exosomal pellets were washed in phosphate-buffered saline (PBS) and were further ultracentrifuged at 100 000 g for 90 min at 4 °C. Finally, the exosomes were washed with PBS and collected by ultracetrifugation again at 100 000 g for 90 min at 4 °C.
RNA extraction
Total RNA was extracted from 400 μl of serum using a mirVana PARIS kit (Ambion, Austin, TX, USA), and was isolated from tissue specimens, cultured cells, and exosomal pellets using the TRIzol reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturers’ instructions.
miRNA array
The miRNA microarrays were manufactured by Agilent Technologies (Santa Clara, CA, USA), and 100 ng of total RNA was labelled and hybridised using the Human microRNA Microarray Kit protocol for use with the Human miRNA Microarray Kit (Release 16.0, Agilent Technologies, Santa Clara, CA, USA). Hybridisation signals were detected with a DNA microarray scanner G2505C (Agilent Technologies) and the scanned images were analysed using the Agilent feature extraction software programme (v10.7.3.1). Normalisation was performed using the Agilent GeneSpring GX software programme version 11.0.2 (per chip: normalisation to control genes; per gene: none). There were a total of 1205 human and 144 human viral miRNAs on the Agilent Human miRNA Microarray (Design ID: 031181), not including control probes.
qRT–PCR
The expression levels of miR-1246 (assay ID: 462575) in tissues and cell lines were analysed by TaqMan quantitative real-time PCR (TaqMan MicroRNA Assays; Applied Biosystems, Carlsbad, CA, USA) and normalised to the level of RNU6B (assay ID: 001093) using a 7300 Real-Time PCR system (Applied Biosystems) according to the manufacturer’s protocol. For the serum samples and the culture media, miR-16 (assay ID: 000391), a reliable endogenous control for investigating the serum miRNA levels used in recent studies (Mitchell et al, 2008; Huang et al, 2010), was also detected. All reactions were performed in duplicate.
Squamous cell carcinoma antigen and carcinoembryonic antigen
The serum level of squamous cell carcinoma antigen (SCC-Ag), known as a potential indicator of ESCC tumour progression (Terashima et al, 1990), is commonly used in the diagnostics of oesophageal cancer. The serum levels of SCC-Ag were measured by chemiluminescent assays (Abbott Japan Co., Ltd, Tokyo, Japan). The serum level of carcinoembryonic antigen (CEA) is commonly used for screening of gastrointestinal malignancies. The serum levels of CEA were measured by chemiluminescent enzyme immunoassays (FUJIREBIO Inc., Tokyo, Japan). In our institution, the cut-off concentrations for SCC-Ag and CEA were 1.5 and 5.2 ng ml−1, respectively.
Statistical analyses
The Mann–Whitney U-test or unpaired Student’s t-test was performed to compare the differences in the serum miRNA expression levels between the cancer patients and the healthy control patients, and the Wilcoxon t-test was used to compare the paired serum samples obtained from pre- and postoperative patients and the paired tissue samples obtained from primary ESCC and corresponding normal oesophageal epithelia. The Kruskal–Wallis test was performed to compare the differences in miRNA expressions in more than three groups. The χ2-test or Fisher’s exact probability test was used to evaluate the correlations between the results of the serum miRNA expression levels and the clinicopathological factors. Receiver-operating characteristic (ROC) curves and the area under the ROC curve (AUC) were used to assess the feasibility of using the serum miRNA expression levels or SCC-Ag as diagnostic markers for detecting ESCC. The survival period of the patients was defined as the duration from the time of surgery to death, or to the last follow-up day, and the survival rate was calculated using the Kaplan–Meier method. The comparison of two groups as a univariate analysis was performed using the Log-rank test. From this result, factors with less than a P-value of 0.1 were selected for the multivariate analysis with Cox’s proportional hazard regression model. All tests were two-sided, and the significance level was set at P<0.05. The Expert StatView (version 5, SAS Institute, Inc., Cary, NC, USA) and SPSS version 16.0 (WPSS Ltd., Surrey, UK) software programme were used for the analyses.
Results
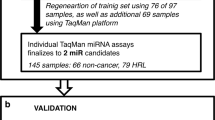
Marked upregulation/downregulation of serum miRNAs in ESCC patients compared with controls
The miRNA expression profile of the serum samples from ESCC patients was examined using a microarray analysis of three ESCC patients and four healthy controls. MiR-16 was used as an endogenous control. The microarray was only used to identify candidates for further analysis. The expression levels of six miRNAs were markedly upregulated in ESCC serum samples compared with controls, and the levels of five miRNAs were markedly downregulated in the ESCC serum samples (P<0.05; Table 1). The miR-1246 expression level was the most markedly upregulated in the serum from ESCC patients. Therefore, miR-1246 was selected as a candidate for a further analysis.
Upregulation of miR-1246 in ESCC serum samples
Following this miRNA screening, we evaluated the serum expression level of miR-1246 in a total of 46 healthy controls and 101 ESCC patients by qRT–PCR. The miR-1246 expression level in the serum from ESCC patients was significantly higher than in that from controls (P<0.0001; Figure 1a). During this analysis, we performed the Kruskal–Wallis H-test to compare the differences in the serum miRNA expression levels of all samples for each year. There were no significant differences in the expression levels of miR-1246 for each year. Furthermore, we grouped the patients and healthy controls based on age and gender, and compared the serum miR-1246 expression levels between patients and healthy controls within the same group. The median age was used as the threshold, and patients and healthy controls were separated into older and younger age groups, respectively. There was no significant difference between these groups. However, among male and female, a significant difference was observed only in healthy controls, not in patients. Although it is very interesting, this problem is considered to be a future examination subject. Either way, even when only the female healthy samples were used as controls, a significant difference existed between controls and patients (data not shown).
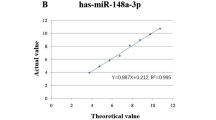
The serum expression levels of miR-1246. (A) Box plots of the serum miR-1246 expression levels in healthy controls (n=46) and ESCC patients (n=101). The Mann–Whitney U-test was performed to determine the statistical significance of the differences. The serum expression levels of miR-1246 were significantly higher in the ESCC patients than in the controls (P<0.0001). (B) The results of a comparison of the serum miR-1246 expression levels between pre- and postoperative samples obtained from ESCC patients. In seven cases, the miR-1246 expression levels of the postoperative samples were significantly lower than that of the preoperative samples (P<0.05).
To evaluate whether the serum expression level of miR-1246 could be used to monitor tumour dynamics, we compared the miR-1246 expression levels between pre- and postoperative samples obtained from ESCC patients. In seven cases, the miR-1246 expression levels of the postoperative samples were significantly lower than those of the preoperative samples (P<0.05; Figure 1b).
The ROC curve analysis revealed that at the optimal cut-off value of 1.3234 for miR-1246, the sensitivity was 71.3% and the specificity was 73.9%, with an AUC of 0.754 (95% confidence interval, 0.676–0.831; Figure 2a).
The results of the ROC curve analysis using the assays for detecting ESCC. (A) The results of the ROC curve analysis of the miR-1246 assay for detecting ESCC. The analysis revealed that at the optimal cut-off value of 1.3234 for miR-1246, the sensitivity was 71.3% and the specificity was 73.9%, with an AUC of 0.754 (95% confidence interval, 0.676–0.831). (B) The results of the ROC curve analysis of using SCC-Ag to detect ESCC. The ROC analysis revealed that at the optimal cut-off value of 1.15 for SCC-Ag, the sensitivity was 57.4% and the specificity was 67.4%, with an AUC of 0.665 (95% confidence interval, 0.577–0.754).
The usefulness of SCC-Ag for detecting ESCC was previously reported to be superior to that of other classical tumour markers (Mroczko et al, 2008). Therefore, to evaluate whether the serum level of miR-1246 could be used as a tumour marker, we compared the sensitivity and specificity of the miR-1246 expression with the serum level of SCC-Ag. The sensitivity was 57.4% and the specificity was 67.4% at the optimal cut-off value of 1.15 for SCC-Ag, with an AUC of 0.665 (95% confidence interval, 0.577–0.754; Figure 2b). This indicates that miR-1246 could be superior to SCC-Ag for the detection of ESCC.
Correlation of serum miR-1246 with the clinicopathological features of ESCC
We next examined the association of the serum expression level of miR-1246 with the clinicopathological factors of ESCC. In this study, the mean miR-1246 expression level of the 101 patients was used as the threshold, and patients were separated into a high-expression group (with an expression level above the mean expression level: 3.5899) and a low-expression group (with an expression level below the mean). Box plots of miR-1246 levels for controls and low-expression and high-expression categories were shown in Figure 3a. There were significant differences between controls and the patients with lower expression levels of serum miR-1246 (P<0.000001), and between the lower and higher expression levels (P<0.05). The relationship between the serum miR-1246 expression level and the clinicopathological features of the patients is summarised in Table 2. The results revealed that the miR-1246 expression levels in the serum samples from patients with T1–2 were significantly lower than those from patients with T3–4 (P=0.0024), from patients without lymph node metastasis were lower than those from patients with lymph node metastasis (P=0.0002), from patients without distant metastasis were lower than those from patients with distant metastasis (P=0.0020), and from patients with stage I–II were lower than those from patients with stage III–IV (P=0.0007; according to the Union International Contre le Cancer; Seventh Edition, 2009). Furthermore, there were significant correlations with survival of patients (P=0.0009) and resectability (P=0.0087). However, there was no correlation with age and gender.
The analysis for ESCC patients grouped by their mean level of serum miR-1246. (A) Box plots of miR-1246 levels for controls and low-expression and high-expression categories. There were significant differences between controls and the patients with lower expression levels of serum miR-1246 (P<0.000001), and between the lower and higher expression levels (P<0.05). (B) The prognostic value of the miR-1246 expression level. The Kaplan–Meier analysis and log-rank test showed that there was a significant difference (P<0.0001) between patients with higher and lower levels of serum miR-1246 expression. The 2-year overall survival rate for patients with a lower serum miR-1246 expression level was 77.3%, whereas that for patients with a higher miR-1246 expression level was 21.7%.
Correlation of serum miR-1246 with the prognosis of ESCC patients
An analysis of the overall survival was performed using the Kaplan–Meier approach, with the statistical analysis performed using the log-rank test. The ESCC patients were divided into two groups according to their miR-1246 expression level (high/low; Figure 3b). The prognostic value of the miR-1246 expression level was then tested. The log-rank test showed that there was a significant difference (P<0.0001) in the survival between the patients with higher and lower expression levels of serum miR-1246. The 2-year overall survival rate in the patients with lower serum miR-1246 expression was 77.3%, whereas that of the patients with the higher miR-1246 expression was 21.7%. We then performed comparisons of the 2-year survival rate with regard to various clinicopathological factors, as seen in Table 3a. Among the various clinical factors, the serum level of miR-1246, tumour depth, lymph node metastasis, and distant metastasis, were found to significantly impact survival (P<0.0001, P<0.0001, P<0.0001, and P=0.0005, respectively), although the age, sex, the serum level of SCC-Ag, and CEA did not significantly impact survival (P=0.5670, P=0.2495, P=0.0595, and P=0.7978, respectively).
We next analysed the importance of various factors that may be able to predict a poor prognosis for survival. According to a univariate analysis, tumour depth, lymph node metastasis, distant metastasis, the serum level of SCC-Ag, and miR-1246 were selected. On the basis of a multivariate analysis (Table 3b), the serum level of miR-1246 was found to be the strongest independent risk factor for a poor survival with a hazard ratio of 4.032 (95% confidence interval: 1.277–12.733; P=0.017).
No upregulation of miR-1246 in ESCC tissue samples
To determine whether the serum level of miR-1246 corresponded to the tissue expression, we evaluated the tissue miR-1246 expression level in samples from 22 ESCC patients by qRT–PCR. There were no significant differences in the expression levels of miR-1246 between primary ESCC tissues and the corresponding normal oesophageal epithelia in these patients (Figure 4a).
The tissue expression levels of miR-1246. (A) The miR-1246 expression levels in ESCC tissue samples. The Wilcoxon t-test was performed to determine the statistical significance of the differences. There was no significant difference (P=0.421) between primary ESCC and corresponding normal oesophageal epithelia. (B) The miR-1246 expression levels in lymph nodes dissected with the primary ESCC tumour. In four ESCC patients, the dissected lymph nodes were separated into four groups (A: abdominal lymph nodes; P: proximal lymph nodes; T: thoracic lymph nodes; and C: cervical lymph nodes). The miR-1246 expression in the lymph nodes was evaluated by qRT–PCR, and the average of each lymph node group was analysed. The Kruskal–Wallis test was performed to determine the statistical significance of the differences between lymph node groups. The expression level of miR-1246 in the proximal lymph nodes was significantly higher than that of the other groups (P<0.05). (C) The ratios of exosomal to cellular miR-1246. Exosomal miR-1246 and cellular miR-1246 were evaluated, and the ratios of exosomal to cellular miR-1246 were shown. In all ESCC cell lines we used, miR-1246 was found to be expressed to a greater extent in the exosomes compared with their donor cells, whereas it was not so in the fibroblast cell lines.
Upregulation of miR-1246 in proximal lymph nodes
We hypothesised that miR-1246 was secreted from the ESCC lesions into the blood or lymphatic vessels actively and selectively. To investigate our hypothesis, we examined the expression levels of miR-1246 in dissected lymph nodes, and a total of 32 lymph nodes from four different patients were evaluated. We divided all of the dissected lymph nodes into the four lymph node stations according to their location (abdominal lymph nodes, proximal lymph nodes, thoracic lymph nodes, and cervical lymph nodes). The proximal lymph nodes were the para-oesophageal lymph nodes located at the same level as the primary tumour. The lymph nodes were evaluated by qRT–PCR, and we calculated the mean value for each lymph node station. The expression levels of miR-1246 in proximal lymph nodes were significantly higher than those of the lymph nodes in other stations (P<0.05; Figure 4b), thus indicating that the miRNA is apparently secreted into the lymphatic system by the tumour.
The expression levels of exosomal and cellular miR-1246 in the cell lines
The human ESCC cell lines, TE1, TE2, TE4, TE6, and TE11, and the human fibroblast cell lines, WI38 and MRC5, were examined by qRT–PCR. Exosomal miR-1246 and cellular miR-1246 were evaluated, and the ratios of exosomal to cellular miR-1246 are shown in Figure 4c. In all ESCC cell lines we used, miR-1246 was found to be expressed to a greater extent in the exosomes compared with their donor cells, whereas it was not so in the fibroblast cell lines.
Discussion
Although the mechanism underlying their secretion is still being elucidated, the miRNAs present in the blood stream (circulating miRNAs) have been shown to be remarkably stable, even in the RNase-rich environment of the blood. Furthermore, the miRNA levels were found to be independent of the subject age and sex, and are similar in plasma and serum (Hunter et al, 2008; Michell et al, 2008). Freeze-thawing, as well as prolonged storage at room temperature, has a minimal effect on the miRNA levels (Michell et al, 2008). Recently, advances in circulating miRNA research have indicated that intracellular miRNAs may be released into the circulation during processes accompanying cellular destruction or pathological injury (Ji et al, 2009; Cheng et al, 2010). Thus, circulating miRNAs have the potential to be used as novel biomarkers.
The use of tumour-derived miRNA (miR-141) in the plasma to identify prostate cancer patients was first described by Mitchell et al (2008), and showed the potential of using miRNAs as new biomarkers. Accumulating reports have confirmed the potential of miRNAs as biomarkers for various cancers, such as lymphoma and oral, colorectal, ovarian, lung, breast, gastric, and oesophageal cancers (Lawrie et al, 2008; Wong et al, 2008; Ng et al, 2009; Resnick et al, 2009; Heneghan et al, 2010; Hu et al, 2010; Tsujiura et al, 2010; Komatsu et al, 2011; Wang et al, 2011). However, these previous studies did not provide any direct evidence demonstrating whether the serum miRNAs are actively secreted or passively leaked from tumour cells.
Recent studies of serum miRNAs have suggested the existence of several mechanisms underlying their release into the blood stream and their avoidance of RNase digestion. The breakthrough explanation of the circulating RNA stability was the discovery of mRNA and miRNA in exosomes from mouse and human mast cells (Valadi et al, 2007). The existence of extracellular Ago2–miRNA complexes in plasma raises the possibility that cells release a functional miRNA-induced silencing complex into the circulation, and this protein carrier-based communication mechanism could regulate the gene expression in recipient cells (Arroyo et al, 2011). Other investigators have also agreed that miRNAs can be secreted from cells and can deliver a gene-silencing signal between living cells in vitro and in vivo (Iguchi et al, 2010).
In the present study, we performed genome-wide miRNA profiling and identified 11 miRNAs whose expression was markedly different (6 miRNAs were upregulated and 5 miRNAs were downregulated) in the serum of patients with ESCC compared with healthy controls. MiR-1246 was the most markedly elevated of these miRNAs. Therefore, miR-1246 was selected as a candidate for the further analysis.
Our data in the validation group revealed that miR-1246 could have superior discriminatory power compared with SCC-Ag, and that the miR-1246 expression levels in the serum samples from patients with T1–2 were significantly lower than those from patients with T3–4 (P=0.0024), from patients without lymph node metastasis were lower than those from patients with lymph node metastasis (P=0.0002), from patients without distant metastasis were lower than those from patients with distant metastasis (P=0.0020), and from patients with stage I–II were lower than those from patients with stage III–IV (P=0.0007). Furthermore, there were significant correlations with survival of patients and resectability. According to the multivariate analysis, the serum level of miR-1246 was found to be the strongest independent poor prognostic factor. In seven cases, the miR-1246 expression levels of the postoperative samples were significantly lower than those of the preoperative samples. Evaluating the serum miR-1246 expression may thus have important clinical implications for risk stratification and the planning of post-therapeutic surveillance. These results suggested that miR-1246 could therefore be a valuable diagnostic and prognostic biomarker for ESCC.
MiR-1246 was reported to be a target of the p53 family, and inhibits Down syndrome-associated DYRK1A, consequently activating NFAT1c and inducing apoptosis (Zhang et al, 2011). Other reports showed that miR-1246 expressions were upregulated in colorectal cancer tissues (Piepoli et al, 2012). To date, whether miR-1246 acts as an oncomir or tumour suppressor is unknown. Pigati et al (2010) reported that the extracellular and intracellular miRNA profiles differed, and suggested the existence of a cellular selection mechanism for miR-1246 release. Thus, we speculate that ESCC cells may selectively secret or release intracellular miR-1246 into the serum, and as a result miR-1246 is increased in the serum samples of ESCC patients. Of note, we observed discrepant expression of miR-1246 between the tissue samples and serum obtained from ESCC patients. Other studies have also shown contrasting changes in the miRNA expression levels between tissue and blood samples (Tanaka et al, 2009; Wang et al, 2009; Liu et al, 2012). The reason for these differences can be explained by the possible existence of miRNA-releasing or -capturing mechanisms present in cells and blood.
Kosaka and Ochiya (2011) proposed two hypotheses regarding secretory miRNA-mediated cancer progression. One is the function of secreted miRNA with the potential to modulate the microenvironmental cells, which have the capacity to take up miRNAs. It is also possible that the secretory miRNA is produced remotely from the primary organ, and affects malignant cell recruitment, extracellular matrix deposition, and vascular proliferation. Aprelikova and Green, (2012) alsoreported that the extracellular miRNA could influence the tumour microenvironment, including cancer-associated fibroblasts, which are important stromal components of growing tumours. In addition, we showed that the miR-1246 expression levels were significantly upregulated in proximal lymph nodes compared with distal lymph nodes in ESCC patients with no metastasis. Furthermore, exosomal miR-1246 was found to be expressed to a greater extent compared with cellular miR-1246 in the ESCC cell lines, whereas it was not so in the fibroblast cell lines. These results suggested the existence of a mechanism leading to the active release of miRNAs, and of a potential signalling network mediated by secretory miRNAs, especially those associated with metastasis and the tumour microenvironment.
There were 178 potential miR-1246 target genes predicted by the TargetScan 6.1 programme. These genes, which have a conserved site in their 3′-untranslated regions, include three cell adhesion-related genes: CDH2 (cadherin 2), ANTXR2 (anthrax toxin receptor 2), and PCDHB5 (protocadherin beta 5). We therefore speculate that miR-1246 may function as a cell adhesion-related miRNA released from ESCC that affects distant organs. Such a role may be associated with the high rate of metastasis of ESCC.
In conclusion, our results demonstrated the diagnostic and prognostic values of the circulating miR-1246 level in ESCC patients, and suggested the existence of the potential functions of circulating miR-1246 as part of an intercellular network correlated with cancer development.
Change history
19 February 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ambros V (2004) The functions of animal microRNAs. Nature 431: 350–355
Aprelikova O, Green JE (2012) MicroRNA regulation in cancer-associated fibroblasts. Cancer Immunol Immunother 61: 231–237
Arroyo JD, Chevillet JR, Kroh EM, Ruf IK, Pritchard CC, Gibson DF, Mitchell PS, Bennett CF, Pogosova-Agadjanyan EL, Stirewalt DL, Tait JF, Tewari M (2011) Argonaute2 complexes carry a population of circulating microRNAs independent of vesicles in human plasma. Proc Natl Acad Sci USA 108: 5003–5008
Barber TW, Duong CP, Leong T, Bressel M, Drummond EG, Hicks RJ (2012) 18F-FDG PET/CT has a high impact on patient management and provides powerful prognostic stratification in the primary staging of esophageal cancer: a prospective study with mature survival data. J Nucl Med 53: 864–871
Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116: 281–297
Calin GA, Trapasso F, Shimizu M, Dumitru CD, Yendamuri S, Godwin AK, Ferracin M, Bernardi G, Chatterjee D, Baldassarre G, Rattan S, Alder H, Mabuchi H, Shiraishi T, Hansen LL, Overgaard J, Herlea V, Mauro FR, Dighiero G, Movsas B, Rassenti L, Kipps T, Baffa R, Fusco A, Mori M, Russo G, Liu CG, Neuberg D, Bullrich F, Negrini M, Croce CM (2005) Familial cancer associated with a polymorphism in ARLTS1. N Engl J Med 352: 1667–1676
Chen J, Pan J, Zheng X, Zhu K, Li J, Chen M, Wang J, Liao Z (2012) Number and location of positive nodes, postoperative radiotherapy, and survival after esophagectomy with three-field lymph node dissection for thoracic esophageal squamous cell carcinoma. Int J Radiat Oncol Biol Phys 82: 475–482
Chen X, Ba Y, Ma L, Cai X, Yin Y, Wang K, Guo J, Zhang Y, Chen J, Guo X, Li Q, Li X, Wang W, Zhang Y, Wang J, Jiang X, Xiang Y, Xu C, Zheng P, Zhang J, Li R, Zhang H, Shang X, Gong T, Ning G, Wang J, Zen K, Zhang J, Zhang CY (2008) Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res 18: 997–1006
Cheng Y, Tan N, Yang J, Liu X, Cao X, He P, Dong X, Qin S, Zhang C (2010) A translational study of circulating cell-free microRNA-1 in acute myocardial infarction. Clin Sci 119: 87–95
Chim SS, Shing TK, Hung EC, Leung TY, Lau TK, Chiu RW, Lo YM (2008) Detection and characterization of placental microRNAs in maternal plasma. Clin Chem 54: 482–490
Gilad S, Meiri E, Yogev Y, Benjamin S, Lebanony D, Yerushalmi N, Benjamin H, Kushnir M, Cholakh H, Melamed N, Bentwich Z, Hod M, Goren Y, Chajut A (2008) Serum microRNAs are promising novel biomarkers. PLoS One 3: e3148
He L, Hannon GJ (2004) MicroRNAs: small RNAs with a big role gene regulation. Nat Rev Genet 5: 522–531
He L, Thomson JM, Hemann MT, Hernando-Monge E, Mu D, Goodson S, Powers S, Cordon-Cardo C, Lowe SW, Hannon GJ, Hammond SM (2005) A microRNA polycistron as a potential human oncogene. Nature 435: 828–833
Heneghan HM, Miller N, Lowery AJ, Sweeney KJ, Newell J, Kerin MJ (2010) Circulating microRNAs as novel minimally invasive biomarkers for breast cancer. Ann Surg 251: 499–505
Ho AS, Huang X, Cao H, Christman-Skieller C, Bennewith K, Le QT, Koong AC (2010) Circulating miR-210 as a novel hypoxia marker in pancreatic cancer. Transl Oncol 3: 109–113
Hu Z, Chen X, Zhao Y, Tian T, Jin G, Shu Y, Chen Y, Xu L, Zen K, Zhang C, Shen H (2010) Serum microRNA signatures identified in a genome-wide serum microRNA expression profiling predict survival of non-small-cell lung cancer. J Clin Oncol 28: 1721–1726
Huang Z, Huang D, Ni S, Peng Z, Sheng W, Du X (2010) Plasma microRNAs are promising novel biomarkers for early detection of colorectal cancer. Int J Cancer 127: 118–126
Hunter MP, Ismail N, Zhang X, Aguda BD, Lee EJ, Yu L, Xiao T, Schafer J, Lee ML, Schmittgen TD, Nana-Sinkam SP, Jarjoura D, Marsh CB (2008) Detection of microRNA expression in human peripheral blood microvesicles. PLoS One 3: e3694
Iguchi H, Kosaka N, Ochiya T (2010) Secretory microRNAs as a versatile communication tool. Commun Integr Biol 3: 478–481
Iorio MV, Ferracin M, Liu CG, Veronese A, Spizzo R, Sabbioni S, Magri E, Pedriali M, Fabbri M, Campiglio M, Ménard S, Palazzo JP, Rosenberg A, Musiani P, Volinia S, Nenci I, Calin GA, Querzoli P, Negrini M, Croce CM (2005) MicroRNA gene expression deregulation in human breast cancer. Cancer Res 65: 7065–7070
Ji X, Takahashi R, Hiura Y, Hirokawa G, Fukushima Y, Iwai N (2009) Plasma miR-208 as a biomarker of myocardial injury. Clin Chem 55: 1944–1949
Komatsu S, Ichikawa D, Takeshita H, Tsujiura M, Morimura R, Nagata H, Kosuga T, Iitaka D, Konishi H, Shiozaki A, Fujiwara H, Okamoto K, Otsuji E (2011) Circulating microRNAs in plasma of patients with oesophageal squamous cell carcinoma. Br J Cancer 105: 104–111
Kosaka N, Ochiya T (2011) Unraveling the mystery of cancer by secretory microRNA: horizontal microRNA transfer between living cells. Front Genet 2: 97
Lawrie CH, Gal S, Dunlop HM, Pushkaran B, Liggins AP, Pulford K, Banham AH, Pezzella F, Boultwood J, Wainscoat JS, Hatton CS, Harris AL (2008) Detection of elevated levels of tumour-associated microRNAs in serum of patients with diffuse large B-cell lymphoma. Br J Haematol 141: 672–675
Liu H, Zhu L, Liu B, Yang L, Meng X, Zhang W, Ma Y, Xiao H (2012) Genome-wide microRNA profiles identify miR-378 as a serum biomarker for early detection of gastric cancer. Cancer Lett 316: 196–203
Lu J, Getz G, Miska EA, Alvarez-Saavedra E, Lamb J, Peck D, Sweet-Cordero A, Ebert BL, Mak RH, Ferrando AA, Downing JR, Jacks T, Horvitz HR, Golub TR (2005) MicroRNA expression profiles classify human cancers. Nature 435: 834–838
Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, Pogosova-Agadjanyan EL, Peterson A, Noteboom J, O'Briant KC, Allen A, Lin DW, Urban N, Drescher CW, Knudsen BS, Stirewalt DL, Gentleman R, Vessella RL, Nelson PS, Martin DB, Tewari M (2008) Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci USA 105: 10513–10518
Mroczko B, Kozłowski M, Groblewska M, Łukaszewicz M, Nikliński J, Jelski W, Laudański J, Chyczewski L, Szmitkowski M (2008) The diagnostic value of the measurement of matrix metalloproteinase 9 (MMP-9), squamous cell cancer antigen (SCC) and carcinoembryonic antigen (CEA) in the sera of esophageal cancer patients. Clin Chim Acta 389: 61–66
Ng EK, Chong WW, Jin H, Lam EK, Shin VY, Yu J, Poon TC, Ng SS, Sung JJ (2009) Differential expression of microRNAs in plasma of patients with colorectal cancer: a potential marker for colorectal cancer screening. Gut 58: 1375–1381
Piepoli A, Tavano F, Copetti M, Mazza T, Palumbo O, Panza A, di Mola FF, Pazienza V, Mazzoccoli G, Biscaglia G, Gentile A, Mastrodonato N, Carella M, Pellegrini F, di Sebastiano P, Andriulli A (2012) Mirna expression profiles identify drivers in colorectal and pancreatic cancers. PLoS One 7: e33663
Pigati L, Yaddanapudi SC, Iyengar R, Kim DJ, Hearn SA, Danforth D, Hastings ML, Duelli DM (2010) Selective release of microRNA species from normal and malignant mammary epithelial cells. PLoS One 5: e13515
Resnick KE, Alder H, Hagan JP, Richardson DL, Croce CM, Cohn DE (2009) The detection of differentially expressed microRNAs from the serum of ovarian cancer patients using a novel real-time PCR platform. Gynecol Oncol 112: 55–59
Schickel R, Boyerinas B, Park SM, Peter ME (2008) MicroRNAs: key players in the immune system, differentiation, tumorigenesis and cell death. Oncogene 27: 5959–5974
Tachimori Y, Kanamori N, Uemura N, Hokamura N, Igaki H, Kato H (2009) Salvage esophagectomy after high-dose chemoradiotherapy for esophageal squamous cell carcinoma. J Thorac Cardiovasc Surg 137: 49–54
Tanaka M, Oikawa K, Takanashi M, Kudo M, Ohyashiki J, Ohyashiki K, Kuroda M (2009) Down-regulation of miR-92 in human plasma is a novel marker for acute leukemia patients. PLoS One 4: e5532
Taylor DD, Gercel-Taylor C (2008) MicroRNA signatures of tumor-derived exosomes as diagnostic biomarkers of ovarian cancer. Gynecol Oncol 110: 13–21
Terashima M, Ikeda K, Ishida K, Saito K (1990) Establishment of an esophageal squamous cell carcinoma tumor line and development of serum squamous cell carcinoma-related antigen in athymic nude mice. J Surg Oncol 44: 225–228
Tsujiura M, Ichikawa D, Komatsu S, Shiozaki A, Takeshita H, Kosuga T, Konishi H, Morimura R, Deguchi K, Fujiwara H, Okamoto K, Otsuji E (2010) Circulating microRNAs in plasma of patients with gastric cancers. Br J Cancer 102: 1174–1179
Valadi H, Ekström K, Bossios A, Sjöstrand M, Lee JJ, Lötvall JO (2007) Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol 9: 654–659
Volinia S, Calin GA, Liu CG, Ambs S, Cimmino A, Petrocca F, Visone R, Iorio M, Roldo C, Ferracin M, Prueitt RL, Yanaihara N, Lanza G, Scarpa A, Vecchione A, Negrini M, Harris CC, Croce CM (2006) A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci USA 103: 2257–2261
Wang K, Zhang S, Marzolf B, Troisch P, Brightman A, Hu Z, Hood LE, Galas DJ (2009) Circulating microRNAs, potential biomarkers for drug-induced liver injury. Proc Natl Acad Sci USA 106: 4402–4407
Wang T, Wang Q, Zhao D, Cui Y, Cao B, Guo L, Lu SH (2011) The oncogenetic role of microRNA-31 as a potential biomarker in oesophageal squamous cell carcinoma. Clin Sci 121: 437–447
Wong TS, Liu XB, Wong BY, Ng RW, Yuen AP, Wei WI (2008) Mature miR-184 as potential oncogenic microRNA of squamous cell carcinoma of tongue. Clin Cancer Res 14: 2588–2592
Yanaihara N, Caplen N, Bowman E, Seike M, Kumamoto K, Yi M, Stephens RM, Okamoto A, Yokota J, Tanaka T, Calin GA, Liu CG, Croce CM, Harris CC (2006) Unique microRNA molecular profiles in lung cancer diagnosis and prognosis. Cancer Cell 9: 189–198
Yuequan J, Shifeng C, Bing Z (2010) Prognostic factors and family history for survival of esophageal squamous cell carcinoma patients after surgery. Ann Thorac Surg 90: 908–913
Zhang Y, Liao JM, Zeng SX, Lu H (2011) p53 downregulates Down syndrome-associated DYRK1A through miR-1246. EMBO Rep 12: 811–817
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Takeshita, N., Hoshino, I., Mori, M. et al. Serum microRNA expression profile: miR-1246 as a novel diagnostic and prognostic biomarker for oesophageal squamous cell carcinoma. Br J Cancer 108, 644–652 (2013). https://doi.org/10.1038/bjc.2013.8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.8
Keywords
This article is cited by
-
Exploring miR-155-5p and miR-1246 as Diagnostic and Prognostic Markers in Oral Squamous cell carcinoma
Molecular Biology Reports (2024)
-
A Literature Review of Traumatic Brain Injury Biomarkers
Molecular Neurobiology (2022)
-
Integrated view of molecular diagnosis and prognosis of dengue viral infection: future prospect of exosomes biomarkers
Molecular and Cellular Biochemistry (2022)
-
Urinary microRNA biomarkers for detecting the presence of esophageal cancer
Scientific Reports (2021)
-
miRNA-1246 in extracellular vesicles secreted from metastatic tumor induces drug resistance in tumor endothelial cells
Scientific Reports (2021)