Abstract
Background:
In recent years, plasma fibrinogen has been ascribed an important role in the pathophysiology of tumour cell invasion and metastases. A relatively small-scale study has indicated that plasma fibrinogen levels may serve as a prognostic factor for predicting clinical outcomes in non-metastatic renal cell carcinoma (RCC) patients.
Methods:
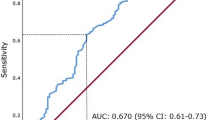
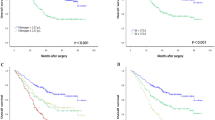
Data from 994 consecutive non-metastatic RCC patients, operated between 2000 and 2010 at a single, tertiary academic centre, were evaluated. Analyses of plasma fibrinogen levels were performed one day before the surgical interventions. Patients were categorised using a cut-off value of 466 mg dl−1 according to a calculation by receiver-operating curve analysis. Cancer-specific (CSS), metastasis-free (MFS), as well as overall survival (OS) were assessed using the Kaplan–Meier method. To evaluate the independent prognostic impact of plasma fibrinogen level, a multivariable Cox regression model was performed for all three different endpoints.
Results:
High plasma fibrinogen levels were associated with various well-established prognostic factors, including age, advanced tumour stage, tumour grade and histologic tumour necrosis (all P<0.05). Furthermore, in multivariable analysis, a high plasma fibrinogen level was statistically significantly associated with a poor outcome for patients’ CSS (hazard ratio (HR): 2.47, 95% confidence interval (CI): 1.49–4.11, P<0.001), MFS (HR: 2.15, 95% CI: 1.44–3.22, P<0.001) and OS (HR: 2.48, 95% CI: 1.80–3.40, P<0.001).
Conclusion:
A high plasma fibrinogen level seems to represent a strong and independent negative prognostic factor regarding CSS, MFS and OS in non-metastatic RCC patients. Thus, this easily determinable laboratory value should be considered as an additional prognostic factor for RCC patients’ individual risk assessment.
Similar content being viewed by others
Main
Worldwide, the incidence rates of renal cell carcinoma (RCC) have slightly increased within the last three decades, and a stage migration towards small and organ-confined tumours has been observed (Pichler et al, 2012; Siegel et al, 2012). To identify risk factors that are able to accurately predict the clinical outcome of RCC patients is of paramount importance. Such risk factors allow the assessment of the patient’s individual risk profile and thereby facilitate the decision whether to perform adjuvant treatment or not (Crispen et al, 2008; Meskawi et al, 2012). Growing evidence suggest that an interactive relationship exists between haemostatic factors and tumour biology (Palumbo, 2008). Of these haemostatic factors, plasma fibrinogen has been reported to be synthesised and overexpressed in human tumours (Sahni et al, 2008). Recently published studies have shown that a high pre-therapeutic plasma fibrinogen level independently predict adverse events and the clinical outcome of patients with various cancer types (Polterauer et al, 2009; Seebacher et al, 2010; Tang et al, 2010; Tanaka et al, 2012). In patients with metastatic RCC, high plasma fibrinogen levels were found to be independently associated with the patients’ survival and response to interleukin-2 therapy (Casamassima et al, 2005; Tsimafeyeu et al, 2009). However, with regards to patients with non-metastatic RCC, existing data on the prognostic role of high plasma fibrinogen levels are based on relatively small cohort studies (Xiao et al, 2011; Du et al, 2012). Only one study, which included 286 patients with non-metastatic RCC, found pre-operative plasma fibrinogen levels to be independently associated with distant metastases and survival (Du et al, 2012). The validation of a prognostic parameter using large independent cohorts of patients is regarded as inevitable before it’s general applicability (Altman and Royston, 2000; Bleeker et al, 2003). The aim of the present study was to further clarify the prognostic value of pre-operative plasma fibrinogen levels in patients with non-metastatic RCC. For this purpose, we conducted a large validation study using three different clinical endpoints, analysing almost 1000 consecutive non-metastatic RCC patients.
Materials and methods
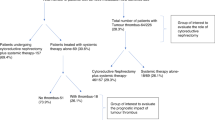
This retrospective analysis included data from 994 consecutive non-metastatic RCC patients who underwent a curative (open) partial or radical (open/laparoscopic) nephrectomy and a blood collection before surgery for RCC at the Department of Urology at the Medical University of Graz between January 2000 and December 2010. Lymphadenectomy was done only in the presence of enlarged nodes. All clinico-pathological data were retrieved from medical records from the Department of Urology, as well as from pathology records from the Institute of Pathology at the same institution. As the TNM classification system for RCC changed during the study period, pathologic T stages were uniformly adjusted according to the seventh edition of this system (Novara et al, 2010). Other documented clinico-pathological parameters included histological subtype, tumour grade, the presence or absence (not quantitatively assessed) of histologic coagulative tumour necrosis (TN), patients’ age and gender. Analyses of laboratory data, including plasma fibrinogen levels, were routinely performed 1 day before surgery. Plasma fibrinogen level was determined by the Clauss method by using reagents, standards and control plasma from Dade Behring on a BCS analyser (Dade Behring, Marburg, Germany). The inter-assay coefficient of variation was <3% and <7.5% for the plasma control in the normal and pathological range, respectively.
Pre-operative exploration to exclude metastatic disease included a computed tomography of the chest, abdomen and pelvis. Pre-operative bone scan or brain magnetic resonance imaging was only performed in the presence of clinical symptoms. Patients with metastatic disease at the date of diagnosis were excluded from this study. Follow-up examination after nephrectomy included routine clinical and laboratory examination every 3 months within the first 3 years, every 6 months within the fourth and fifth post-operative years, and every 12 months between the sixth and ninth post-operative years. Imaging methods included X-rays of the chest and abdominal ultrasound in patients with a low relapse risk (pT-1 and G1–2) every 6 months, whereas computed tomography or magnetic resonance imaging of the abdomen and chest was performed every 6 months within the first 3 years in all other patients, and every 12 months between the fourth and fifth years thereafter (Pichler et al, 2011). No neoadjuvant or adjuvant treatment was administered. Dates of death were obtained from the central registry of the Austrian Bureau of Statistics. Survival data were mainly retrieved from the electronic patient records of our institution (i.e., the Medical University of Graz) or by electronic records of any other accessible hospital in the district of Styria. Missing data were retrieved using letters and telephone interviews with patients and/or family doctors involved. Death was assessed as either cancer related or unrelated. All deaths of patients who had confirmed metastatic RCC at any time were considered to be cancer-related. Cancer-specific survival (CSS) was defined as the time (in months) from the date of surgery to a cancer-related death. Metastasis-free survival (MFS) was defined as the time (in months) from the date of surgery to the recurrence of radiologically or histologically confirmed distant metastases. Overall survival (OS) was defined as the time (in months) from the date of surgery to individuals’ death of any cause. The study was approved by the local ethical committee of the Medical University of Graz (No. 24-330 ex 11/12).
Statistical analyses
The primary study endpoint was CSS, which was calculated from the date of diagnosis to the date of cancer-related death. Secondary endpoints included OS (the time between diagnosis and death of any cause) and MFS (the time between diagnosis and occurrence of distant metastases). The optimal cut-off value for the continuous variable plasma fibrinogen level was calculated by applying a receiver-operating curve analysis to test all possible cut-offs that would discriminate between patients’ survival and cancer-related death. The relationship between plasma fibrinogen level and other clinico-pathological parameters was studied by non-parametric tests (χ2-test and Mann–Whitney’s U-test). Patients’ clinical endpoints were calculated using the Kaplan–Meier method and were compared by the log rank test. Backward stepwise multivariable Cox proportion analysis was performed to determine the influence of pathologic T stage, tumour grade, age, gender, as well as histologic TN on CSS, MFS and OS. Hazard ratios estimated from the Cox analysis were reported as relative risks with corresponding 95% confidence intervals. All statistical analyses were performed using the Statistical Package for Social Sciences version 17.0 (SPSS Inc., Chicago, IL, USA). A two-sided P<0.05 was considered statistically significant.
Results
Patient’s characteristics of the study cohort are shown in Table 1. Applying the criteria mentioned above, a plasma fibrinogen level cut-off value of 466 mg dl−1 was optimal for discrimination between CSS. We used this cut-off value throughout all further analyses. There were 694 (69.8%) patients with plasma fibrinogen levels below and 300 (30.2%) patients with plasma fibrinogen levels above the cut-off value. High plasma fibrinogen levels were associated with older age (P=0.007), high tumour grade, advanced tumour stage and the presence of histologic TN (all P<0.001), but not with the patients’ gender (P=0.096) or the histological RCC subtype (P=0.08).
Mean follow-up was 48.1 (range 0–132) months. Of the 994 RCC patients, 117 (11.8%) developed metastatic disease; of these, 79 (7.9%) died due to their advanced disease state. Overall, 180 (18.1%) patients died from any cause. Overall, two patients (0.2%) died within the post-operative 30-day course. Both patients belonged to the high plasma fibrinogen level group. One patient died of myocardial infarction and the other one because of post-operative sepsis. Among the 994 RCC patients, metastatic disease was diagnosed in 49 out of 694 (7.1%) patients with low plasma fibrinogen levels and in 68 out of 300 (22.7%) patients with high plasma fibrinogen levels (P<0.001). Regarding patients’ survival, cancer-related and overall deaths occurred in 30 (4.3%) and 91 (13.1%) patients with low plasma fibrinogen level, and in 49 (16.3%) and 89 (29.7%) patients with high plasma fibrinogen level (each, P<0.001). Figures 1, 2 and 3 show the Kaplan–Meier curves for CSS, MFS and OS, and reveal that a high plasma fibrinogen level is a consistent factor for poor prognosis in RCC patients (P<0.001 for all three tested endpoints, log-rank test).
Univariable analysis identified age, advanced tumour stage, high tumour grade, presence of histologic TN and high plasma fibrinogen levels as poor prognostic parameters for CSS, whereas gender was not statistically significantly associated with CSS (Table 2). To determine the prognostic value of pre-operative plasma fibrinogen levels for CSS, MFS and OS, independent of other prognostic parameters (older age, high tumour grade, advanced tumour stage and the presence of histologic TN), multivariable analyses using a Cox proportional hazard model were performed. The results of the multivariable analyses revealed high plasma fibrinogen levels to be associated with CSS, MFS and OS, independently of other prognostic parameters included in the analyses (Table 3).
Discussion
Despite recent progress in the identification of genetic and molecular alterations in RCC, including gene mutations, chromosomal aberrations and differential microRNA expression (Al-Ali et al, 2012; Gerlinger et al, 2012), the routine prognostic risk assessment of RCC patients currently relies on traditional clinico-pathological prognostic variables (Ficarra et al, 2010). Routinely measured blood-based parameters, such as the plasma fibrinogen level, are established, and reproducibly detectable parameters without additional laborious efforts, making them attractive parameters for improved diagnostic or prognostic purposes in RCC (Zahorec, 2001).
To the best of our knowledge to date, only one study addresses the prognostic significance of plasma fibrinogen level in localised RCC using a multivariable Cox proportional analysis. In this study, Du et al (2012) analysed a cohort of 286 RCC patients and showed that a high plasma fibrinogen level was statistically significantly associated with Fuhrman grade, tumour size and pathologic T stage. In a multivariable analysis, they also demonstrated that the high plasma fibrinogen level remained an independent prognostic factor for disease-free survival and OS in their relatively small cohort (Du et al, 2012). In our large validation study that included 994 patients with non-metastatic RCC, we were able to demonstrate that a high plasma fibrinogen level was an independent negative predictor for all tested clinical endpoints, including CSS, MFS and OS. To the best of our knowledge, our study currently represents the most comprehensive one testing the independent prognostic significance of plasma fibrinogen level in non-metastatic RCC patients. Our findings corroborate the results of Du et al (2012), who also found an independent prognostic value for the fibrinogen level in 286 RCC patients with regard to disease-free survival and OS.
A definitive explanation for this observation remains speculative. However, several previous experimental and clinical studies support the observation of our validation study. On the basis of the results derived from previous findings, fibrinogen may enhance human tumour progression and development of metastases through several possible mechanisms. First, the soluble form of fibrinogen could serve as a bridging molecule between tumour cells and the surrounding microenvironment. For instance, Zheng et al (2009) demonstrated that tumour cells prefer to adhere to fibrinogen and that fibrinogen enhances the adhesion of tumour cells to platelets. This mechanism is mediated by β3-integrins, which are expressed on human cancer cells and facilitate the protection of tumour cells from natural killer cell cytotoxicity (Zheng et al, 2009). The important influence of the interaction between cancer cell-expressed integrins and fibrinogen has also been demonstrated in an inflammation-driven animal cancer model of colorectal cancer (Steinbrecher et al, 2010). This study also suggests that therapies targeting fibrinogen-α(M)β(2) integrin interaction may be useful in preventing and/or treating this important subset of malignancies (Steinbrecher et al, 2010). In another study by Roche et al (2003), the authors showed that cancer cells from bladder cancer express intercellular calcium-dependent adhesion molecule 1, which facilitates the binding of extracellular localised fibrinogen. These interaction properties enable a fibrinogen-dependent migration and invasion of cancer cells. Second, fibrinogen might also directly influence biological behaviour of cancer cells. In this context, Sahni et al (2008) demonstrated that fibrinogen is synthesised by epithelial cancer cells and that this endogenously synthesised fibrinogen promotes the growth of lung and prostate cancer cells through interaction with fibroblast growth factor 2. However, in our retrospective study we were not able to show a precise causal relationship between hyperfibrinogenaemia and clinical outcome of RCC patients. Besides these functions, fibrinogen is also part of the coagulation cascade, and high pre-operative plasma fibrinogen levels might also impair patients’ survival by triggering thromboembolism events. Overall, the post-operative incidence of fatal thromboembolic events seemed to be low in our study cohort, as only two patients died in the postoperative 30-day period, due to non-thromboembolic complications. Although we did not systematically prospectively explore the incidence of thromboembolic events in our study cohort, a prospectively collected data set of 2208 RCC patients reported by Pettus et al (2006) also reported a low frequency (1%) of pulmonary embolism after nephrectomy. Several prospective studies reported about a higher rate of thromboembolic events and a higher risk of mortality associated with elevated plasma D-dimer levels in cancer patients (Ay et al, 2009, 2012; Stender et al, 2012; Yang et al, 2012). However, whether high plasma fibrinogen levels are invariably associated with a higher risk of thromboembolism in cancer patients, remains controversial. For instance, Tiedje et al (2011) showed in the prospective Vienna Cancer and Thrombosis Study that plasma fibrinogen level was not associated with a higher rate of venous thromboembolic events in their study cohort. Interestingly, there was also no association between high plasma fibrinogen levels and venous thromboembolic events in a large non-cancer-related study population of more than 20 000 patients (Tsai et al, 2002). In contrast, Song et al (2006) reported a higher postoperative risk for pulmonary embolism in patients with high plasma fibrinogen levels.
As with all retrospective studies, the limitations of our study are inherent to the design, including the retrospective data collection. Moreover, the patients from this study underwent surgical treatment by multiple surgeons. In an attempt to control for the homogeneity of the study population, we excluded patients with hereditary RCC, patients with metachronous secondary RCC and those with competitive invasive cancers originating from other sites if metastatic spread was not assessed through histology. The incidence of thromboembolic events, which might influence clinical outcome as a potential confounder, was not prospectively recorded. However, a simple retrospective analysis of the occurrence of symptomatic thromboembolic events will probably not be sufficient to answer the question whether higher fibrinogen levels are associated with higher thromboembolism-related mortality. As we have previously shown, also asymptomatic thrombosis might influence survival rates in cancer patients (Gary et al, 2012). Therefore, a future prospective study will have to systematically include all patients for duplex sonography/computed tomography of the chest screening to detect symptomatic as well as asymptomatic thromboembolic disease, and include this data into a multivariate analysis. Nonetheless, even considering these limitations, our data clearly indicate that a high plasma fibrinogen level is an independent prognostic factor for CSS, MFS and OS in non-metastatic RCC patients. This parameter should be considered in future prognostic studies and might enable a better ability to predict RCC patients’ clinical outcome when integrated into established prognostic models.
In conclusion, a high plasma fibrinogen level represents an independent predictor with respect to CSS, MFS and OS in patients with non-metastatic RCC. This parameter should be considered in future risk assessment tools and adjuvant trials as a selection criterion for risk factor-stratified patient management in non-metastatic RCC.
Change history
03 September 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Al-Ali BM, Ress AL, Gerger A, Pichler M (2012) MicroRNAs in renal cell carcinoma: implications for pathogenesis, diagnosis, prognosis and therapy. Anticancer Res 32 (9): 3727–3732.
Altman DG, Royston P (2000) What do we mean by validating a prognostic model? Stat Med 19 (4): 453–473.
Ay C, Dunkler D, Pirker R, Thaler J, Quehenberger P, Wagner O, Zielinski C, Pabinger I (2012) High D-dimer levels are associated with poor prognosis in cancer patients. Haematologica 97 (8): 1158–1164.
Ay C, Vormittag R, Dunkler D, Simanek R, Chiriac AL, Drach J, Quehenberger P, Wagner O, Zielinski C, Pabinger I (2009) D-dimer and prothrombin fragment 1+2 predict venous thromboembolism in patients with cancer: results from the Vienna Cancer and Thrombosis Study. J Clin Oncol 27 (25): 4124–4129.
Bleeker SE, Moll HA, Steyerberg EW, Donders AR, Derksen-Lubsen G, Grobbee DE, Moons KG (2003) External validation is necessary in prediction research: a clinical example. J Clin Epidemiol 56 (9): 826–832.
Casamassima A, Picciariello M, Quaranta M, Berardino R, Ranieri C, Paradiso A, Lorusso V, Guida M (2005) C-reactive protein: a biomarker of survival in patients with metastatic renal cell carcinoma treated with subcutaneous interleukin-2 based immunotherapy. J Urol 173 (1): 52–55.
Crispen PL, Boorjian SA, Lohse CM, Leibovich BC, Kwon ED (2008) Predicting disease progression after nephrectomy for localized renal cell carcinoma: the utility of prognostic models and molecular biomarkers. Cancer 113 (3): 450–460.
Du J, Zheng JH, Chen XS, Yang Q, Zhang YH, Zhou L, Yao X (2012) High preoperative plasma fibrinogen is an independent predictor of distant metastasis and poor prognosis in renal cell carcinoma. Int J Clin Oncol 18 (3): 517–523.
Ficarra V, Brunelli M, Cheng L, Kirkali Z, Lopez-Beltran A, Martignoni G, Montironi R, Novara G, Van Poppel H (2010) Prognostic and therapeutic impact of the histopathologic definition of parenchymal epithelial renal tumors. Eur Urol 58 (5): 655–668.
Gary T, Belaj K, Steidl K, Pichler M, Eisner F, Stoger H, Hafner F, Froehlich H, Samonigg H, Pilger E, Brodmann M (2012) Asymptomatic deep vein thrombosis and superficial vein thrombosis in ambulatory cancer patients: impact on short-term survival. Br J Cancer 107 (8): 1244–1248.
Gerlinger M, Rowan AJ, Horswell S, Larkin J, Endesfelder D, Gronroos E, Martinez P, Matthews N, Stewart A, Tarpey P, Varela I, Phillimore B, Begum S, McDonald NQ, Butler A, Jones D, Raine K, Latimer C, Santos CR, Nohadani M, Eklund AC, Spencer-Dene B, Clark G, Pickering L, Stamp G, Gore M, Szallasi Z, Downward J, Futreal PA, Swanton C (2012) Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med 366 (10): 883–892.
Meskawi M, Sun M, Trinh QD, Bianchi M, Hansen J, Tian Z, Rink M, Ismail S, Shariat SF, Montorsi F, Perrotte P, Karakiewicz PI (2012) A review of integrated staging systems for renal cell carcinoma. Eur Urol 62 (2): 303–314.
Novara G, Ficarra V, Antonelli A, Artibani W, Bertini R, Carini M, Cosciani Cunico S, Imbimbo C, Longo N, Martignoni G, Martorana G, Minervini A, Mirone V, Montorsi F, Schiavina R, Simeone C, Serni S, Simonato A, Siracusano S, Volpe A, Carmignani G (2010) Validation of the 2009 TNM version in a large multi-institutional cohort of patients treated for renal cell carcinoma: are further improvements needed? Eur Urol 58 (4): 588–595.
Palumbo JS (2008) Mechanisms linking tumor cell-associated procoagulant function to tumor dissemination. Semin Thrombosis Hemostasis 34 (2): 154–160.
Pettus JA, Eggener SE, Shabsigh A, Yanke B, Snyder ME, Serio A, Vickers A, Russo P, Donat SM (2006) Perioperative clinical thromboembolic events after radical or partial nephrectomy. Urology 68 (5): 988–992.
Pichler M, Hutterer GC, Chromecki TF, Jesche J, Kampel-Kettner K, Pummer K, Zigeuner R (2012) Renal cell carcinoma stage migration in a single European centre over 25 years: effects on 5- and 10-year metastasis-free survival. Int Urol Nephrol 44 (4): 997–1004.
Pichler M, Hutterer GC, Chromecki TF, Jesche J, Kampel-Kettner K, Rehak P, Pummer K, Zigeuner R (2011) External validation of the Leibovich prognosis score for nonmetastatic clear cell renal cell carcinoma at a single European center applying routine pathology. J Urol 186 (5): 1773–1777.
Polterauer S, Grimm C, Seebacher V, Concin N, Marth C, Tomovski C, Husslein H, Leipold H, Hefler-Frischmuth K, Tempfer C, Reinthaller A, Hefler L (2009) Plasma fibrinogen levels and prognosis in patients with ovarian cancer: a multicenter study. Oncologist 14 (10): 979–985.
Roche Y, Pasquier D, Rambeaud JJ, Seigneurin D, Duperray A (2003) Fibrinogen mediates bladder cancer cell migration in an ICAM-1-dependent pathway. Thrombosis Haemostasis 89 (6): 1089–1097.
Sahni A, Simpson-Haidaris PJ, Sahni SK, Vaday GG, Francis CW (2008) Fibrinogen synthesized by cancer cells augments the proliferative effect of fibroblast growth factor-2 (FGF-2). J Thrombosis Haemostasis 6 (1): 176–183.
Seebacher V, Polterauer S, Grimm C, Husslein H, Leipold H, Hefler-Frischmuth K, Tempfer C, Reinthaller A, Hefler L (2010) The prognostic value of plasma fibrinogen levels in patients with endometrial cancer: a multi-centre trial. Br J Cancer 102 (6): 952–956.
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics (2012) Cancer J Clin 62 (1): 10–29.
Song SW, Lee HS, Kim MS, Lee JM, Kim JH, Nam BH, Zo JI (2006) Preoperative serum fibrinogen level predicts postoperative pulmonary complications after lung cancer resection. Ann Thoracic Surg 81 (6): 1974–1981.
Steinbrecher KA, Horowitz NA, Blevins EA, Barney KA, Shaw MA, Harmel-Laws E, Finkelman FD, Flick MJ, Pinkerton MD, Talmage KE, Kombrinck KW, Witte DP, Palumbo JS (2010) Colitis-associated cancer is dependent on the interplay between the hemostatic and inflammatory systems and supported by integrin alpha(M)beta(2) engagement of fibrinogen. Cancer Res 70 (7): 2634–2643.
Stender MT, Larsen TB, Sorensen HT, Thorlacius-Ussing O (2012) Preoperative plasma D-dimer predicts 1-year survival in colorectal cancer patients with absence of venous thromboembolism (VTE): a prospective clinical cohort study. J Thrombosis Haemostasis 10 (10): 2027–2031.
Tanaka N, Kikuchi E, Matsumoto K, Hayakawa N, Ide H, Miyajima A, Nakamura S, Oya M (2012) Prognostic value of plasma fibrinogen levels in patients with localized upper tract urothelial carcinoma. BJU Int 111 (6): 857–864.
Tang L, Liu K, Wang J, Wang C, Zhao P, Liu J (2010) High preoperative plasma fibrinogen levels are associated with distant metastases and impaired prognosis after curative resection in patients with colorectal cancer. J Surg Oncol 102 (5): 428–432.
Tiedje V, Dunkler D, Ay C, Horvath B, Quehenberger P, Pabinger M, Zielinski C, Pabinger I, Mannhalter C (2011) The role of fibrinogen plasma levels, the -455G>A fibrinogen and the factor XIII A subunit (FXIII-A) Val34Leu polymorphism in cancer-associated venous thrombosis. Thrombosis Haemostasis 106 (5): 908–913.
Tsai AW, Cushman M, Rosamond WD, Heckbert SR, Tracy RP, Aleksic N, Folsom AR (2002) Coagulation factors, inflammation markers, and venous thromboembolism: the longitudinal investigation of thromboembolism etiology (LITE). Am J Med 113 (8): 636–642.
Tsimafeyeu IV, Demidov LV, Madzhuga AV, Somonova OV, Yelizarova AL (2009) Hypercoagulability as a prognostic factor for survival in patients with metastatic renal cell carcinoma. J Exper Clin Cancer Res 28: 30.
Xiao B, Ma LL, Zhang SD, Xiao CL, Lu J, Hong K, Liao HY (2011) Correlation between coagulation function, tumor stage and metastasis in patients with renal cell carcinoma: a retrospective study. Chinese Med J 124 (8): 1205–1208.
Yang Y, Zhou Z, Niu XM, Li ZM, Chen ZW, Jian H, Ai XH, Cheng BJ, Liao ML, Lu S (2012) Clinical analysis of postoperative venous thromboembolism risk factors in lung cancer patients. J Surg Oncol 106 (6): 736–741.
Zahorec R (2001) Ratio of neutrophil to lymphocyte counts—rapid and simple parameter of systemic inflammation and stress in critically ill. Bratislavske Lekarske Listy 102 (1): 5–14.
Zheng S, Shen J, Jiao Y, Liu Y, Zhang C, Wei M, Hao S, Zeng X (2009) Platelets and fibrinogen facilitate each other in protecting tumor cells from natural killer cytotoxicity. Cancer Sci 100 (5): 859–865.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Pichler, M., Hutterer, G., Stojakovic, T. et al. High plasma fibrinogen level represents an independent negative prognostic factor regarding cancer-specific, metastasis-free, as well as overall survival in a European cohort of non-metastatic renal cell carcinoma patients. Br J Cancer 109, 1123–1129 (2013). https://doi.org/10.1038/bjc.2013.443
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.443
Keywords
This article is cited by
-
High fibrinogen levels are associated with poor survival in patients with liposarcoma
Scientific Reports (2023)
-
Preoperative fibrinogen/CRP score predicts survival in upper urothelial tract carcinoma patients undergoing radical curative surgery
World Journal of Urology (2023)
-
The prognostic value of FAR and a novel FAR-CA125 score in resectable gastric signet ring cell carcinoma patients
Journal of Cancer Research and Clinical Oncology (2023)
-
Impact of fibrinogen levels and modified Glasgow prognostic score on survival of stage III/N2 non-small cell lung cancer patients treated with neoadjuvant therapy and radical resection
BMC Cancer (2022)
-
High fibrinogen-albumin ratio index (FARI) predicts poor survival in head and neck squamous cell carcinoma patients treated with surgical resection
European Archives of Oto-Rhino-Laryngology (2022)