Abstract
Objectives
The International Continence Society defines nocturia as the need to void one or more times during the night, with each of the voids preceded and followed by sleep. The chronic sleep disturbance and sleep deprivation experienced by patients with nocturia affects quality of life, compromising both mental and physical well-being. This paper aims to characterise the burden of nocturia by comparing published data from patients with nocturia with data from patients with any of 12 other common chronic conditions, specifically focusing on its impact on work productivity and activity impairment, as measured by the instrument of the same name (WPAI).
Methods
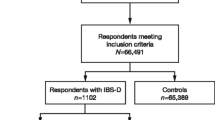
A systematic literature review of multiple data sources identified evaluable studies for inclusion in the analysis. Study eligibility criteria included use of the WPAI instrument in patients with one of a predefined list of chronic conditions. We assessed the quality of each included study using the Newcastle–Ottawa scale and extracted basic study information, work and activity impairment data. To assess how work and activity impairment from nocturia compares with impairment from other common chronic diseases, we conducted two data syntheses (pooled and unpooled).
Results
The number of evaluable studies and the range of overall work productivity impairment reported, respectively, were as follows: nocturia (3; 14–39 %), overactive bladder (5; 11–41 %), irritable bowel syndrome/constipation (14; 21–51 %), gastroesophageal reflux disease (GERD) (13; 6–42 %), asthma/allergies (11; 6–40 %), chronic obstructive pulmonary disease (COPD) (7; 19–42 %), sleep problems (3; 12–37 %), arthritis (13; 21–69 %), pain (9; 29–64 %), depression (4; 15–43 %) and gout (2; 20–37 %).
Conclusions
The overall work productivity impairment as a result of nocturia is substantial and was found to be similar to impairment observed as a result of several other more frequently researched common chronic diseases. Greater awareness of the burden of nocturia, a highly bothersome and prevalent condition, will help policy makers and healthcare decision makers provide appropriate management of nocturia.




Similar content being viewed by others
Notes
WPAI instructions for activity impairment: “By regular activities, we mean the usual activities you do, such as work around the house, shopping, childcare, exercising, studying, etc. Think about times you were limited in the amount or kind of activities you could do and times you accomplished less than you would like. If health problems affected your activities only a little, choose a low number. Choose a high number if health problems affected your activities a great deal.”
The WPAI database of studies (http://www.reillyassociates.net/WPAI_References.html) includes the following health issues: anemia, angioedema, ankylosing spondylitis, arthritis, asthma/allergies, cancer, caregivers, Crohn's disease, chronic obstructive pulmonary disease (COPD), dermatology, diabetes, dyspepsia, erectile dysfunction, eye disease, gastroesophageal reflux disease (GERD), general health, gout, headache, hepatitis, HIV/AIDS, hypertension, inflammatory bowel disease, irritable bowel syndrome (IBS)/chronic constipation, lupus, mental health, multiple sclerosis, neurology, nocturia, obesity/nutrition, OAB, pain, peripheral artery disease (PAD), respiratory, restless legs syndrome, rhinosinusitis, sleep, spondyloarthritis, substance abuse, ulcerative colitis, urinary incontinence, voice disorders, women's health.
For analysis, constipation is combined with IBS, and asthma is combined with rhinitis/allergies, hence 12 common chronic conditions are organised into ten categories to compare with nocturia.
References
van Kerrebroeck P, Abrams P, Chaikin D, Donovan J, Fonda D, Jackson S, Jennum P, Johnson T, Lose G, Mattiasson A, Robertson G, Weiss J. Standardisation Sub-committee of the International Continence Society. The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:179–83.
Tikkinen KA, Johnson TM 2nd, Tammela TL, Sintonen H, Haukka J, Huhtala H, Auvinen A. Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol. 2010;57:488–96.
Bosch JL, Weiss JP. The prevalence and causes of nocturia. J Urol. 2010;184:440–6.
Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, Coyne K, Kelleher C, Hampel C, Artibani W, Abrams P. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306–14.
Strickland R. Reasons for not seeking care for urinary incontinence in older community-dwelling women: a contemporary review. Urol Nurs. 2014;34(2):63–8, 94.
Van Kerrebroeck P, Weiss J. Standardization and terminology of nocturia. BJU Int. 1999;84(Suppl 1):1–4.
Drake MJ. Do we need a new definition of the overactive bladder syndrome? ICI-RS 2013. Neurourol Urodyn. 2014;33(5):622–4.
Van Kerrebroeck P, Hashim H, Holm-Larsen T, Robinson D, Stanley N. Thinking beyond the bladder: antidiuretic treatment of nocturia. Int J Clin Pract. 2010;64(6):807–16.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–65.
Van Roijen L, Essink-Bot ML, Koopmanschap MA, et al. Labour and health status in economic evaluations of health care. Int J Tech Assess Health Care. 1996;12:405–15.
Lerner D, Amick BC III, Rogers WH, et al. The work limitations questionnaire. Med Care. 2001;39:72–85.
Tuomi K, Ilmarinen J, Jahkola A, Katajarinne L, Tulkki A. Work Ability Index. 2nd revised edition. Helsinki: Finnish Institute of Occupational Health; 1998.
Kessler R, Barber C, Beck A. The World Health Organization health and work performance questionnaire (HPQ). J Occup Environ Med. 2003;45:156–74.
Coyne KS, Sexton CC, Kopp ZS, Ebel-Bitoun C, Milsom I, Chapple C. The impact of overactive bladder on mental health, work productivity and health-related quality of life in the UK and Sweden: results from EpiLUTS. BJU Int. 2011;108(9):1459–71.
Reilly Associates. Health outcomes research. http://www.reillyassociates.net/Index.html. Accessed Jun 2016.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M; STROBE Initiative. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12(12):1500–24.
Wells GA, Shea B, O’Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute 2011. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed June 2016.
Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Kobelt G, Borgstrom F, Mattiasson A. Productivity, vitality and utility in a group of healthy professionally active individuals with nocturia. Br J Urol Int. 2003;9(3):190–5.
Andersson F, Blemings A, Holm Larsen T, Nørgaard JP. Waking at night to void can have a profound impact on productivity. Value Health. 2013;16(3):A184.
Biliotti B, Andersson F, Anderson P, Piercy J. Nocturia results in work productivity and activity losses comparable with other chronic diseases. Neurourol Urodyn. 2014;33:779.
Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008;101(11):1388–95.
Coyne KS, Sexton CC, Thompson CL, Clemens JQ, Chen CI, Bavendam T, Dmochowski R. Impact of overactive bladder on work productivity. Urology. 2012;80(1):97–103.
Lee HE, Cho SY, Lee S, Kim M, Oh SJ. Short-term effects of a systematized bladder training program for idiopathic overactive bladder: a prospective study. Int Neurourol J. 2013;17(1):11–7.
Péntek M, Gulácsi L, Majoros A, Piróth C, Rubliczky L, Böszörményi Nagy G, Törzsök F, Timár P, Baji P, Brodszky V. Health related quality of life and productivity of women with overactive bladder. Orv Hetil. 2012;153(27):1068–76.
Tang DH, Colayco DC, Khalaf KM, Piercy J, Patel V, Globe D, Ginsberg D. Impact of urinary incontinence on healthcare resource utilization, health-related quality of life and productivity in patients with overactive bladder. BJU Int. 2014;113(3):484–91.
Bracco A, Reilly MC, McBurney C, Ambegaonkar B. Burden of irritable bowel syndrome with constipation on health care resource utilization, work productivity and activity impairment and quality of life. 13th World Congress of Gastroenterology; Montreal; September 10–14, 2005. Available from (http://www.reillyassociates.net/WPAI_References.html).
Bracco A, Reilly MC, McBurney C, Ambegaonkar B. Burden of irritable bowel syndrome with constipation on health care resource utilisation, work productivity and activity impairment and quality of life in France, Germany and United Kingdom. United European Gastroenterology Week; Copenhagen; Oct 15–19, 2005. Available from: http://www.reillyassociates.net/WPAI_References.html.
Buono JL, Tourkodimitris S, Sarocco P, Johnston JM, Carson RT. Impact of linaclotide treatment on work productivity and activity impairment in adults with irritable bowel syndrome with constipation: results from 2 randomized, double-blind, placebo-controlled phase 3 trials. Am Health Drug Benefits. 2014;7(5):289–97.
Dean BB, Aguilar D, Barghout V, Kahler KH, Frech F, Groves D, Ofman JJ. Impairment in work productivity and health-related quality of life in patients with IBS. Am J Manag Care. 2005;11:S17–26.
Dibonaventura MD, Prior M, Prieto P, Fortea J. Burden of constipation-predominant irritable bowel syndrome (IBS-C) in France, Italy, and the United Kingdom. Clin Exp Gastroenterol. 2012;5:203–12.
Dibonaventura M, Sun SX, Bolge SC, Wagner JS, Mody R. Health-related quality of life, work productivity and health care resource use associated with constipation predominant irritable bowel syndrome. Curr Med Res Opin. 2011;27(11):2213–22.
Neri L, Basilisco G, Corazziari E, Stanghellini V, Bassotti G, Bellini M, Perelli I, Cuomo R, LIRS Study Group. Constipation severity is associated with productivity losses and healthcare utilization in patients with chronic constipation. United European. Gastroenterol J. 2014;2(2):138–47.
Pare P, Lam S, Balshaw R, et al. Patient characteristics (irritable bowel syndrome with constipation [IBS-C]): baseline results from LOGIC (Longitudinal Outcomes study of GI symptoms in Canada). Presented American College of Gastroenterology October 30, 2005, Honolulu, Hawaii. Available from: http://www.reillyassociates.net/WPAI_References.html.
Reilly MC, Barghout V, McBurney CR, Niecko TE. Effect of tegaserod on work and daily activity in IBS with constipation. Aliment Pharmacol Ther. 2005;22:373–80.
Reilly MC, Bracco A, Geissler K, Johanson J, Kahler KH. Impact of irritable bowel syndrome (IBS) on work productivity and daily activities. 69th Annual Meeting American College of Gastroenterology; Orlando FL; 3 Nov 2004. Available from: http://www.reillyassociates.net/WPAI_References.html.
Sun SX, Dibonaventura M, Purayidathil FW, Wagner JS, Dabbous O, Mody R. Impact of chronic constipation on health-related quality of life, work productivity, and healthcare resource use: an analysis of the National Health and Wellness Survey. Dig Dis Sci. 2011;56(9):2688–95.
Engsbro AL, Begtrup LM, Kjeldsen J, Larsen PV, de Muckadell OS, Jarbøl DE, Bytzer P. Patients suspected of irritable bowel syndrome: cross-sectional study exploring the sensitivity of Rome III Criteria in primary care. Am J Gastroenterol. 2013;108(6):972–80.
Stanghellini V, Lecchi A, Mackinnon J, Bertsch J, Fortea J, Tack J. 2015 Economic and quality-of-life burden of moderate-to-severe irritable bowel syndrome with constipation (IBS-C) in Italy: The IBIS-C study. Digestive and Liver Disease Conference 21st National Congress of Digestive Diseases, Italian Federation of Societies of Digestive Diseases, FISMAD 2015; Bologna, Italy; 25–28 March 2015: e129.
Yiannakou Y, Eugenicos M, Sanders DS, Emmanuel A, Whorwell P, Butt F, Bridger S, Arebi N, Millar A, Kaushik V, Rance M, Mackinnon J, Bertsch J, Fortea J, Tack J. 2015 Economic and quality-of-life burden of moderate-to-severe irritable bowel syndrome with constipation (IBS-C) in the UK: The IBIS-C study. Gut Conference 2nd Digestive Disorders Federation Conference, DDF; July 22–25, 2015; London, p. A33–4.
Bixquert M, Calleja J, Maldonado J, Ballesteros E, Vara S, Rico-Villademoros F. Impact of nocturnal heartburn on quality of life, sleep and productivity: the Sinerge Study. Gut 2004; 53(Suppl V1):A99.
Bruley des Varannes S, Ducrotté P, Vallot T, Garofano A, Bardoulat I, Carrois F, Ricci L. Gastroesophageal reflux disease: Impact on work productivity and daily-life activities of daytime workers. A French cross-sectional study. Dig Liver Dis. 2013; 45(3):200–6.
Dean BB, Crawley JA, Schmitt CM., Ofman JJ. The Impact of GERD Symptoms on Worker Productivity and Absenteeism. ACG Meeting 2001. Available from: http://www.reillyassociates.net/WPAI_References.html.
El-Dika S, Guyatt GH, Armstrong D, Degl’innocenti A, Wiklund I, et al. The impact of illness in patients with moderate to severe gastro-esophageal reflux disease. BMC Gastroenterol. 2005;5:23.
Gisbert JP, Cooper A, Karagiannis D, Hatlebakk J, Agréus L, Jablonowski H, Nuevo J. Impact of gastroesophageal reflux disease on work absenteeism, presenteeism and productivity in daily life: a European observational study. Health Qual Life Outcomes. 2009;7:90.
Gross M, Beckenbauer U, Burkowitz J, Walther H, Brueggenjuergen B. Impact of gastro-oesophageal reflux disease on work productivity despite therapy with proton pump inhibitors in Germany. Eur J Med Res. 2010;15(3):124–30.
Mody R, Bolge SC, Kannan H, Fass R. Effects of gastro-esophageal reflux disease on sleep and outcomes. Clin Gastroenterol Hepatol. 2009;7(9):953–9.
Nordyke RJ, Aguilar D, Lee A, Singh A, Tedeschi MR, Dubois RW. Linking symptoms diurnality to productivity loss- a new conceptual approach. Presented ISPOR Tenth Annual International Meeting, May 17, 2005, Washington, DC. Available from http://www.reillyassociates.net/WPAI_References.html.
Shin WG, Kim HU, Kim SG, Kim GH, Shim KN, Kim JW, Kim JI, Kim JG, Kim JJ, Yim DH, Park SK, Park SH. The Korean College of Helicobacter and Upper Gastrointestinal Research. Work productivity and activity impairment in gastroesophageal reflux disease in Korean full-time employees: a multicentre study. Dig Liver Dis. 2012;44(4):286–91.
Wahlqvist P, Bergenheim K, Långström G, Næsdal J. Impact on work productivity of upper gastrointestinal symptoms associated with chronic NSAID therapy in a Swedish study population. Value Health. 2003;6(6):A688.
Wahlqvist P, Carlsson J, Stalhammar NO, Wiklund I. Validity of a work productivity and activity impairment questionnaire for patients with symptoms of gastro-esophageal reflux disease (WPAI-GERD) results from a cross-sectional study. Value Health. 2002;5:106–13.
Wahlqvist P, Reilly M, Barkun A. Systematic review: the impact of gastro-oesophageal reflux disease on work productivity. Aliment Pharmacol Ther. 2006;24(2):259–72.
Rokkas T, Panitti E, Nikas N. Prevalence and impact in work productivity of gastroesofageal reflux disease (GERD) in primary care patients with upper gastrointestinal (GI) symptoms. The Greek GERDQ study. ISPOR 13th Annual European Congress Prague Czech Republic. Conference Publication: 2010;13(7):A373.
Andréasson E, Svensson K, Berggren F. The validity of the work productivity and activity impairment questionnaire for patients with asthma (WPAI-asthma): Results from a web-based study. ISPOR 6th Annual European Congress; 9–11 November 2003; Barcelona, Spain. Available from: http://www.reillyassociates.net/WPAI_References.html.
Bousquet J, Neukirch F, Bousquet PJ, Gehano P, Klossek JM, Le Gal M, Allaf B. Severity and impairment of allergic rhinitis in patients consulting in primary care. J Allergy Clin Immunol. 2006;117(1):158–62.
Calhoun WJ, Haselkorn T, Mink DR, Miller DP, Dorenbaum A, Zeiger RS. Clinical burden and predictors of asthma exacerbations in patients on guideline-based steps 4–6 asthma therapy in the TENOR cohort. J Allergy Clin Immunol Pract. 2014;2(2):193–200.
Chen H, Blanc PD, Chawla A, Hayden M, Bleeker ER, Lee JH. Assessing productivity impairment in patients with severe or difficult to treat asthma: validation of the Work Productivity and Activity Impairment- Asthma questionnaire. J Allergy Clin Immunol. 2006;117(2):S181.
de la Hoz Caballer B, Rodríguez M, Fraj J, Cerecedo I, Antolín-Amérigo D, Colás C. Allergic rhinitis and its impact on work productivity in primary care practice and a comparison with other common diseases: The cross-sectional study to evaluate work productivity in allergic rhinitis compared with other common diseases (CAPRI) study. Am J Rhinol Allergy. 2012;26(5):390–4.
Dean BB, Calimlim BC, Sacco P, Aguilar D, Maykut R, Tinkelman D. Uncontrolled asthma: assessing quality of life and productivity of children and their caregivers using a cross-sectional Internet-based survey. Health Qual Life Outcomes. 2010;8(8):96.
Demoly P, Annunziata K, Gubba E, Adamek L. Repeated cross-sectional survey of patient-reported asthma control in Europe in the past 5 years. Eur Respir Rev. 2012;21(123):66–74.
Eisner MD, Yegin A, Trzaskoma B. Severity of asthma score predicts clinical outcomes in patients with moderate to severe persistent asthma. Chest. 2012;141(1):58–65.
Reilly MC, Tanner A, Meltzer EO. Allergy impairment questionnaires: validation studies. J Allergy Clin Immunology 1996; 97:1:3:430.
Stankiewicz J, Tami T, Truitt T, Atkins J, Winegar B, Cink P, Schaeffer BT, Raviv J, Henderson D, Duncavage J, Hagaman D. Impact of chronic rhinosinusitis on work productivity through one-year follow-up after balloon dilation of the ethmoid infundibulum. Int Forum Allergy Rhinol. 2011;1(1):38–45.
Tan H, Sarawate C, Singer J, Elward K, Cohen RI, Smart BA, Busk MF, Lustig J, O’Brien JD, Schatz M. Impact of asthma controller medications on clinical, economic, and patient-reported outcomes. Mayo Clin Proc. 2009;84(8):675–84.
Allen-Ramey FC, Gupta S, Dibonaventura MD. Patient characteristics, treatment patterns, and health outcomes among COPD phenotypes. Int J Chron Obstruct Pulmon Dis. 2012;7:779–87.
Dacosta Dibonaventura M, Paulose-Ram R, Su J, McDonald M, Zou KH, Wagner JS, Shah H. The impact of COPD on quality of life, productivity loss, and resource use among the elderly United States workforce. COPD. 2012;9(1):46–57.
Dibonaventura MD, Paulose-Ram R, Su J, McDonald M, Zou KH, Wagner JS, Shah H. The burden of chronic obstructive pulmonary disease among employed adults. Int J Chron Obstruct Pulmon Dis. 2012;7:211–9.
Fletcher MJ, Upton J, Taylor-Fishwick J, Buist SA, Jenkins C, Hutton J, Barnes N, Van Der Molen T, Walsh JW, Jones P, Walker S. COPD Uncovered: an International survey on the impact of chronic obstructive pulmonary disease (COPD) on a working age population. BMC Public Health. 2011;11(1):612.
Galaznik A, Chapnick J, Vietri J, Tripathi S, Zou KH, Makinson G. Burden of smoking on quality of life in patients with chronic obstructive pulmonary disease. Expert Rev Pharmacoecon Outcomes Res. 2013;13(6):853–60.
Solem CT, Sun SX, Sudharshan L, Macahilig C, Katyal M, Gao X. Exacerbation-related impairment of quality of life and work productivity in severe and very severe chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2013;8:641–52.
Troosters T, Sciurba FC, Decramer M, Siafakas NM, Klioze SS, Sutradhar SC, Weisman IM, Yunis C. Tiotropium in patients with moderate COPD naive to maintenance therapy: a randomised placebo-controlled trial. NPJ Prim Care Respir Med. 2014;20(24):14003.
Bolge SC, Joish VN, Balkrishnan R, Kannan H, Drake CL. Burden of Chronic sleep maintenance insomnia characterized by nighttime awakenings among anxiety and depression sufferers: results of a national survey. Prim Care Companion J Clin Psychiatry. 2010;12(2):PCC.09m00824. doi:10.4088/PCC.09m00824gry.
Moline M, DiBonaventura MD, Shah D, Ben-Joseph R. Impact of middle-of-the-night awakenings on health status, activity impairment, and costs. Nat Sci Sleep. 2014;23(6):101–11.
Bolge SC, Doan JF, Kannan H, Baran RW. Association of insomnia with quality of life, work productivity, and activity impairment. Qual Life Res. 2009;18(4):415–22.
Bae SC, Gun SC, Mok CC, Khandker R, Nab HW, Koenig AS, Vlahos B, Pedersen R, Singh A. Improved health outcomes with Etanercept versus usual DMARD therapy in an Asian population with established rheumatoid arthritis. BMC Musculoskelet Disord. 2013;14(1):13.
Bansback N, Zhang W, Walsh D, Kiely P, Williams R, Guh D, Anis A, Young A. Factors associated with absenteeism, presenteeism and activity impairment in patients in the first years of RA. Rheumatology (Oxford). 2012;51(2):375–84.
Braakman-Jansen LM, Taal E, Kuper IH, van de Laar MA. Productivity loss due to absenteeism and presenteeism by different instruments in patients with RA and subjects without RA. Rheumatology (Oxford). 2012;51(2):354–61.
Bushmakin AG, Cappelleri JC, Taylor-Stokes G, Sayers J, Sadosky A, Carroll D, Gosden T, Emery P. Relationship between patient-reported disease severity and other clinical outcomes in osteoarthritis: a European perspective. J Med Econ. 2011;14(4):381–9.
Chaparro Del Moral R, Rillo OL, Casalla L, Morón CB, Citera G, Cocco JA, Correa Mde L, Buschiazzo E, Tamborenea N, Mysler E, Tate G, Baños A, Herscovich N. Work productivity in rheumatoid arthritis: relationship with clinical and radiological features. Arthritis. 2012; 2012: 137635.
Di Bonaventura MD, Gupta S, McDonald MM, Sadosky A. Evaluating the health and economic impact of osteoarthritis pain in the workforce: results from the National Health and Wellness Survey. BMC Musculoskelet Disord. 2011;12(1):83.
Dibonaventura MD, Gupta S, McDonald M, Sadosky A, Pettitt D, Silverman S. Impact of self-rated osteoarthritis severity in an employed population: cross-sectional analysis of data from the national health and wellness survey. Health Qual Life Outcomes. 2012;15(10):30.
Hone D, Cheng A, Watson C, Huang B, Bitman B, Huang XY, Gandra SR. Impact of etanercept on work and activity impairment in employed moderate to severe rheumatoid arthritis patients in the United States. Arthritis Care Res (Hoboken). 2013;65(10):1564–72.
Radner H, Smolen JS, Aletaha D. Remission in rheumatoid arthritis: benefit over low disease activity in patient reported outcomes and costs. Arthritis Res Ther. 2014;16(1):R56.
Reilly MC, Gooch KL, Wong RL, Kupper H, van der Heijde D. Validity, reliability and responsiveness of the Work Productivity and Activity Impairment Questionnaire in ankylosing spondylitis. Rheumatology (Oxford). 2010;49(4):812–9.
Tillett W, Shaddick G, Askari A, Cooper A, Creamer P, Clunie G, Helliwell PS, Kay L, Korendowych E, Lane S, Packham J, Shaban R, Williamson L, McHugh N. Factors influencing work disability in psoriatic arthritis: first results from a large UK multicentre study. Rheumatology (Oxford). 2015;54(1):157–62.
Zhang W, Gignac MA, Beaton D, Tang K. Anis AH; Canadian Arthritis Network Work Productivity Group. Productivity loss due to presenteeism among patients with arthritis: estimates from 4 instruments. J Rheumatol. 2010;37(9):1805–14.
Pavelka K, Szekanecz Z, Damjanov N, Majdan M, Nasonov E, Mazurov V, Fabo T, Bananis E, Jones H, Szumski A, Tang B, Kotak S, Koenig AS, Vasilescu R. Induction of response with etanercept-methotrexate therapy in patients with moderately active rheumatoid arthritis in Central and Eastern Europe in the PRESERVE study. Clin Rheumatol. 2013;32:1275–81.
Coyne KS, LoCasale RJ, Datto CJ, Sexton CC, Yeomans K, Tack J. Opioid-induced constipation in patients with chronic noncancer pain in the USA, Canada, Germany, and the UK: descriptive analysis of baseline patient-reported outcomes and retrospective chart review. Clinicoecon Outcomes Res. 2014;23(6):269–81.
Fourquet J, Báez L, Figueroa M, Iriarte RI, Flores I. Quantification of the impact of endometriosis symptoms on health-related quality of life and work productivity. Fertil Steril. 2011;96(1):107–12.
Haglund E, Petersson IF, Bremander A, Bergman S. Predictors of presenteeism and activity impairment outside work in patients with spondyloarthritis. J Occup Rehabil. 2015;25(2):288–95.
Kronborg C, Handberg G, Axelsen F. Health care costs, work productivity and activity impairment in non-malignant chronic pain patients. Eur J Health Econ. 2009;10(1):5–13.
Langley PC, Ruiz-Iban MA, Molina JT, De Andres J, Castellón JR. The prevalence, correlates and treatment of pain in Spain. J Med Econ. 2011;14(3):367–80.
Langley PC, Van Litsenburg C, Cappelleri JC, Carroll D. The burden associated with neuropathic pain in Western Europe. J Med Econ. 2013;16(1):85–95.
Takura T, Ushida T, Kanchiku T, Ebata N, Fujii K, DiBonaventura MD, Taguchi T. The societal burden of chronic pain in Japan: an internet survey. J Orthop Sci. 2015;20(4):750–60.
Vietri J, Otsubo T, Montgomery W, Tsuji T, Harada E. The incremental burden of pain in patients with depression: results of a Japanese survey. BMC Psychiatry. 2015;7(15):104.
Mann R, Bergstrom F, Schaefer C, et al. Characteristics of subjects with human immunodeficiency virus-related neuropathic pain in the United States: beat neuropathic pain observational study. Regional Anesthesia and Pain Medicine. 11th Annual ASRA Pain Medicine Meeting; Miami; 2013;38(1).
Asami Y, Goren A, Okumura Y. Work productivity loss with depression, diagnosed and undiagnosed, among workers in an Internet-based survey conducted in Japan. J Occup Environ Med. 2015;57(1):105–10.
Beck A, Crain LA, Solberg LI, Unützer J, Maciosek MV, Whitebird RR, Rossom RC. The effect of depression treatment on work productivity. Am J Manag Care. 2014;20(8):e294–301.
Giovannetti ER, Wolff JL, Frick KD, Boult C. Construct validity of the Work Productivity and Activity Impairment questionnaire across informal caregivers of chronically ill older patients. Value Health. 2009;12(6):1011–7.
Trivedi MH, Morris DW, Wisniewski SR, Lesser I, Nierenberg AA, Daly E, Kurian BT, Gaynes BN, Balasubramani GK, Rush AJ. Increase in work productivity of depressed individuals with improvement in depressive symptom severity. Am J Psychiatry. 2013;170(6):633–41.
Dibonaventura MD, Andrews LM, Yadao AM, Kahler KH. The effect of gout on health-related quality of life, work productivity, resource use and clinical outcomes among patients with hypertension. Expert Rev Pharmacoecon Outcomes Res. 2012;12(6):821–9.
Khanna P, Nuki G, Bardin T, Tausche AK, Forsythe A, Goren A, Vietri JT, Khanna D. Tophi and frequent gout flares are associated with impairments to quality of life, productivity, and increased healthcare resource use: results from a cross-sectional survey. Health Qual Life Outcomes. 2012;10(1):117.
Acknowledgments
Paul Miller and Harry Hill conducted the searches, data extraction and data syntheses and contributed to drafting the manuscript. Fredrik Andersson designed the project and contributed to drafting the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Paul Miller and Harry Hill received funding from Ferring Pharmaceuticals to undertake this work.
Conflict of interest
Paul Miller has received funding from Ferring Pharmaceuticals for conference travel. Fredrik Andersson is an employee of Ferring Pharmaceuticals, which markets treatments for nocturia.
Rights and permissions
About this article
Cite this article
Miller, P.S.J., Hill, H. & Andersson, F.L. Nocturia Work Productivity and Activity Impairment Compared with Other Common Chronic Diseases. PharmacoEconomics 34, 1277–1297 (2016). https://doi.org/10.1007/s40273-016-0441-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-016-0441-9