Abstract
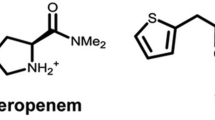
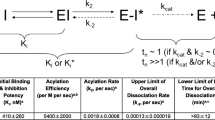
Relebactam (formerly known as MK-7655) is a non-β-lactam, bicyclic diazabicyclooctane, β-lactamase inhibitor that is structurally related to avibactam, differing by the addition of a piperidine ring to the 2-position carbonyl group. Vaborbactam (formerly known as RPX7009) is a non-β-lactam, cyclic, boronic acid-based, β-lactamase inhibitor. The structure of vaborbactam is unlike any other currently marketed β-lactamase inhibitor. Both inhibitors display activity against Ambler class A [including extended-spectrum β-lactamases (ESBLs), Klebsiella pneumoniae carbapenemases (KPCs)] and class C β-lactamases (AmpC). Little is known about the potential for relebactam or vaborbactam to select for resistance; however, inactivation of the porin protein OmpK36 in K. pneumoniae has been reported to confer resistance to both imipenem–relebactam and meropenem–vaborbactam. The addition of relebactam significantly improves the activity of imipenem against most species of Enterobacteriaceae [by lowering the minimum inhibitory concentration (MIC) by 2- to 128-fold] depending on the presence or absence of β-lactamase enzymes. Against Pseudomonas aeruginosa, the addition of relebactam also improves the activity of imipenem (MIC reduced eightfold). Based on the data available, the addition of relebactam does not improve the activity of imipenem against Acinetobacter baumannii, Stenotrophomonas maltophilia and most anaerobes. Similar to imipenem–relebactam, the addition of vaborbactam significantly (2- to > 1024-fold MIC reduction) improves the activity of meropenem against most species of Enterobacteriaceae depending on the presence or absence of β-lactamase enzymes. Limited data suggest that the addition of vaborbactam does not improve the activity of meropenem against A. baumannii, P. aeruginosa, or S. maltophilia. The pharmacokinetics of both relebactam and vaborbactam are described by a two-compartment, linear model and do not appear to be altered by the co-administration of imipenem and meropenem, respectively. Relebactam’s approximate volume of distribution (V d) and elimination half-life (t ½) of ~ 18 L and 1.2–2.1 h, respectively, are similar to imipenem. Likewise, vaborbactam’s V d and t½ of ~ 18 L and 1.3–2.0 h, respectively, are comparable to meropenem. Like imipenem and meropenem, relebactam and vaborbactam are both primarily renally excreted, and clearance correlates with creatinine clearance. In vitro and in vivo pharmacodynamic studies have reported bactericidal activity for imipenem–relebactam and meropenem–vaborbactam against various Gram-negative β-lactamase-producing bacilli that are not inhibited by their respective carbapenems alone. These data also suggest that pharmacokinetic–pharmacodynamic parameters correlating with efficacy include time above the MIC for the carbapenems and overall exposure for their companion β-lactamase inhibitors. Phase II clinical trials to date have reported that imipenem–relebactam is as effective as imipenem alone for treatment of complicated intra-abdominal infections and complicated urinary tract infections, including acute pyelonephritis. Imipenem–relebactam is currently in two phase III clinical trials for the treatment of imipenem-resistant bacterial infections, as well as hospital-associated bacterial pneumonia (HABP) and ventilator-associated bacterial pneumonia (VABP). A phase III clinical trial has reported superiority of meropenem–vaborbactam over piperacillin–tazobactam for the treatment of complicated urinary tract infections, including acute pyelonephritis. Meropenem–vaborbactam has recently demonstrated higher clinical cure rates versus best available therapy for the treatment of carbapenem-resistant Enterobacteriaceae (CRE), as well as for HABP and VABP. The safety and tolerability of imipenem–relebactam and meropenem–vaborbactam has been reported in various phase I pharmacokinetic studies and phase II and III clinical trials. Both combinations appear to be well tolerated in healthy subjects and hospitalized patients, with few serious drug-related treatment-emergent adverse events reported to date. In conclusion, relebactam and vaborbactam serve to broaden the spectrum of imipenem and meropenem, respectively, against β-lactamase-producing Gram-negative bacilli. The exact roles for imipenem–relebactam and meropenem–vaborbactam will be defined by efficacy and safety data from further clinical trials. Potential roles in therapy for these agents include the treatment of suspected or documented infections caused by resistant Gram-negative bacilli-producing ESBL, KPC, and/or AmpC β-lactamases. The usage of these agents in patients with CRE infections will likely become the standard of care. Finally, increased activity of imipenem–relebactam against P. aeruginosa may be of clinical benefit to patients with suspected or documented P. aeruginosa infections.

Similar content being viewed by others
Change history
10 May 2018
Section heading 5.2, which currently reads 5.2 Meropenem–Relebactam.
References
Zhanel GG, Wiebe R, Dilay L, Thomson K, Rubinstein E, Hoban DJ, et al. Comparative review of the carbapenems. Drugs. 2007;67(7):1027–52.
Doi Y, Chambers HF. Other β-lactam antibiotics. In: Mandell G, Bennett J, Dolin R, editors. Principles and practice of infectious diseases. 8th ed. Philadelphia: Saunders Elsevier; 2015. p. 293–7.
Cerceo E, Deitelzweig SB, Sherman BM, Amin AN. Multidrug-resistant Gram-negative bacterial infections in the hospital setting: overview, implications for clinical practice, and emerging treatment options. Microb Drug Resist. 2016;22(5):412–31.
Global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics [Internet]: World Health Organization [published 27 February 2017; cited 23 May 2017]. http://www.who.int/medicines/publications/global-priority-list-antibiotic-resistant-bacteria/en/. Accessed 17 May 2017.
Wong D, van Duin D. Novel beta-lactamase inhibitors: unlocking their potential in therapy. Drugs. 2017;77(6):615–28.
Lob SH, Hackel MA, Kazmierczak KM, Hoban DJ, Young K, Motyl MR, et al. In vitro activity of imipenem–relebactam against gram-negative bacilli isolated from patients with lower respiratory tract infections in the United States in 2015–Results from the SMART global surveillance program. Diagn Microbiol Infect Dis. 2017;88(2):171–6.
Livermore DM, Warner M, Mushtaq S. Activity of MK-7655 combined with imipenem against Enterobacteriaceae and Pseudomonas aeruginosa. J Antimicrob Chemother. 2013;68(10):2286–90.
Toussaint KA, Gallagher JC. β-lactam/β-lactamase inhibitor combinations: from then to now. Ann Pharmacother. 2015;49(1):86–98.
Lapuebla A, Abdallah M, Olafisoye O, Cortes C, Urban C, Quale J, et al. Activity of meropenem combined with RPX7009, a novel β-lactamase inhibitor, against Gram-negative clinical isolates in New York City. Antimicrob Agents Chemother. 2015;59(8):4856–60.
The Medicines Company TANGO-1 analyst call, Carbavance TANGO-1 phase III trial results [Internet]: The Medicines Company [published 27 June 2016; cited 22 May 2017]. http://www.themedicinescompany.com/investors/event/medicines-company-tango-1-analyst-call. Accessed 16 May 2017.
Hecker SJ, Reddy KR, Totrov M, Hirst GC, Lomovskaya O, Griffith DC, et al. Discovery of a cyclic boronic acid β-lactamase inhibitor (RPX7009) with utility vs class A serine carbapenemases. J Med Chem. 2015;58(9):3682–92.
Lin S, Huang C, Ko W, Chen Y, Hsueh P. Recent developments in antibiotic agents for the treatment of complicated intra-abdominal infections. Expert Opin Pharmacother. 2016;17(3):339–54.
Goldstein EJC, Citron DM, Tyrrell KL, Merriam CV. In vitro activity of biapenem plus RPX7009, a carbapenem combined with a serine β-lactamase inhibitor, against anaerobic bacteria. Antimicrob Agents Chemother. 2013;57(6):2620–30.
Livermore DM, Mushtaq S. Activity of biapenem (RPX2003) combined with the boronate β-lactamase inhibitor RPX7009 against carbapenem-resistant Enterobacteriaceae. J Antimicrob Chemother. 2013;68(8):1825–31.
Li XZ, Ma D, Livermore DM, Nikaido H. Role of efflux pump(s) in intrinsic resistance of Pseudomonas aeruginosa: active efflux as a contributing factor to β-lactam resistance. Antimicrob Agents Chemother. 1994;38(8):1742–52.
Köhler T, Michea-Hamzehpour M, Epp SF, Pechere JC. Carbapenem activities against Pseudomonas aeruginosa: respective contributions of OprD and efflux systems. Antimicrob Agents Chemother. 1999;43(2):424–7.
Olsen I. New promising β-lactamase inhibitors for clinical use. Eur J Clin Microbiol Infect Dis. 2015;34(7):1303–8.
Blizzard TA, Chen H, Kim S, Wu J, Bodner R, Gude C, et al. Discovery of MK-7655, a β-lactamase inhibitor for combination with Primaxin®. Bioorg Med Chem Lett. 2014;24(3):780–5.
Mangion IK, Ruck RT, Rivera N, Huffman MA, Shevlin M. A concise synthesis of a β-lactamase inhibitor. Org Lett. 2011;13(20):5480–3.
Morandi S, Morandi F, Caselli E, Shoichet BK, Prati F. Structure-based optimization of cephalothin-analogue boronic acids as beta-lactamase inhibitors. Bioorg Med Chem. 2008;16(3):1195–205.
Jackson JJ, Kropp H. β-lactam antibiotic-induced release of free endotoxin: in vitro comparison of penicillin-binding protein (PBP) 2-specific imipenem and PBP 3-specific ceftazidime. J Infect Dis. 1992;165(6):1033–41.
Lomovskaya O, Tsivkovski R. Vaborbactam (RPX7009) plus meropenem is active against the newly discovered BKC-1 and FRI-1 carbapenemases [abstract no. P1289 plus poster]. In: 26th European Congress of Clinical Microbiology and Infectious Diseases; 2016; Netherlands.
Tsivkovski R, Totrov M, Lomovskaya O. Inhibition of KPC-2 by vaborbactam (VAB; formerly Rpx7009) does not involve Ser130 (S130) that is important for its inhibition by avibactam (AVI) [presentation abstract]. In: ASM Microbe; 2016; Boston.
Zhanel GG, Lawson CD, Adam H, Schweizer F, Zelenitsky S, Lagacé-Wiens PRS, et al. Ceftazidime-avibactam: a novel cephalosporin/β-lactamase inhibitor combination. Drugs. 2013;73(2):159–77.
Jacoby GA, Munoz-Price LS. The new β-lactamases. N Engl J Med. 2005;352(4):380–91.
Shahid M, Sobia F, Singh A, Malik A, Khan HM, Jonas D, et al. Beta-lactams and beta-lactamase-inhibitors in current- or potential-clinical practice: a comprehensive update. Crit Rev Microbiol. 2009;35(2):81–108.
Drawz SM, Bonomo RA. Three decades of β-lactamase inhibitors. Clin Microbiol Rev. 2010;23(1):160–201.
Ambler RP. The structure of β-lactamases. Philos Trans R Soc Lond. 1980;289:321–31.
Bush K, Jacoby GA. Updated functional classification of β-lactamases. Antimicrob Agents Chemother. 2010;54(3):969–76.
Bush K, Jacoby GA, Medeiros AA. A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob Agents Chemother. 1995;39(6):1211–33.
Drawz SM, Papp-Wallace KM, Bonomo RA. New β-lactamase inhibitors: a therapeutic renaissance in an MDR world. Antimicrob Agents Chemother. 2014;58(4):1835–46.
Winkler M, Hujer AM, Bethel CR, Domitrovic TN, Young K, Donomo RA. Imipenem-ciastatin-relebactam (IMI/REL): an analysis of resistance in Pseudomonas aerugoinsa (Pa) isolates [abstract no. C-147 plus poster]. In: 55th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2015; San Diego.
Shlaes DM. New β-lactam-β-lactamase inhibitor combinations in clinical development. Ann N Y Acad Sci. 2013;1277(1):105–14.
Barnes MD, Papp-Wallace KM, Alsop J, Domitrovic TN, Becka SA, Hujer AM, et al. Determining resistance mechanisms in Pseudomonas aeruginosa clinical isolates that demonstrate altered susceptibility profiles to β-lactam-relebactam (REL) vs. β-lactam-avibactam (AVI) combinations [abstract no. P0235 plus poster]. In: 27th European Congress of Clinical Microbiology and Infectious Diseases; 2017; Vienna.
Barnes MD, Bethel CR, Alsop J, Becka SA, Rutter JD, Papp-Wallace KM, et al. Relebactam (REL) inhibits the PDC-3 β-lactamase and restores the susceptibility of imipenem (IMI) against Pseudomonas aeruginosa [abstract no. 2780 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Lapuebla A, Abdallah M, Olafisoye O, Cortes C, Urban C, Landman D, et al. Activity of imipenem with relebactam against Gram-negative pathogens from New York City. Antimicrob Agents Chemother. 2015;59(8):5029–31.
Thaden JT, Pogue JM, Kaye KS. Role of newer and re-emerging older agents in the treatment of infections caused by carbapenem-resistant Enterobacteriaceae. Virulence. 2017;8(4):403–16.
Bush K. A resurgence of β-lactamase inhibitor combinations effective against multidrug-resistant Gram-negative pathogens. Int J Antimicrob Agents. 2015;46(5):483–93.
El Amin N, Giske CG, Jalal S, Keijser B, Kronvall G, Wretlind B. Carbapenem resistance mechanisms in Pseudomonas aeruginosa: alterations of porin OprD and efflux proteins do not fully explain resistance patterns observed in clinical isolates. APMIS. 2005;113(3):187–96.
Haidar G, Clancy CJ, Chen L, Samanta P, Shields RK, Kreiswirth BN, et al. Identifying spectra of activity and therapeutic niches for ceftazidime-avibactam and imipenem–relebactam against carbapenem-resistant Enterobacteriaceae. Antimicrob Agents Chemother. 2017;AAC.00642-17 (in press).
Lomovskaya O, Tsivkovski R. Vaborbactam (VAB) is not affected by KPC-2 and KPC-3 variants containing Asp179Tyr amino acid substitution that are resistant to ceftazidime (CAZ) potentiation with avibactam [abstract no. 4169 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Tsivkovski R, Lomovskaya O. The effect of Trp105 substitutions in KPC on interactions with the novel beta-lactamase inhibitor RPX7009 [presentation abstract no. C-1194]. In: 54th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2014; Washington, D.C.
Sun D, Rubio-Aparicio D, Dudley MN, Lomovskaya O. Characterization of mutants selected in vitro using sub-optimal exposures of meropenem alone and with RPX7009 [abstract no. C-103 plus poster]. In: 54th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2014; Washington, D.C.
Sun D, Rubio-Aparicio D, Griffith D, Dudley MN, Lomovskaya O. Losing my resistance: loss of KPC following exposure of KPC-producing strains of Klebsiella pneumonia to carbapenems in combination with RPX7009 [presentation abstract no. C-1193]. In: 54th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2014; Washington, D.C.
Lob S, Hackel M, Badal R, Young K, Motyl M, Sahm D. In vitro activity of imipenem–relebactam (MK-7655) against Enterobacteriaceae and Pseudomonas aeruginosa from Latin America-SMART 2015 [abstract no. 2857 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Mavridou E, Melchers RJB, van Mil AC, Mangin E, Motyl MR, Mouton JW. Pharmacodynamics of imipenem in combination with β-lactamase inhibitor MK7655 in a murine thigh model. Antimicrob Agents Chemother. 2015;59(2):790–5.
Lob SH, Hackel MA, Kazmierczak KM, Young K, Motyl MR, Karlowsky JA, et al. In vitro activity of imipenem–relebactam against Gram-negative ESKAPE pathogens isolated by clinical laboratories in the United States in 2015–Results from the SMART global surveillance program. Antimicrob. Agents Chemother. 2017;61(6):e02209–16.
Lob S, Young K, Motyl M, Hawser S, Morrissey I, Magnet S, et al. Activity of imipenem–relebactam against Enterobacteriaceae and Pseudomonas aeruginosa from respiratory tract infections in Europe - SMART 2015 [abstract no. P1283 plus poster]. In: 27th European Congress of Clinical Microbiology and Infectious Diseases; 2017; Vienna.
Lob S, Hackel M, Badal R, Young K, Motyl M, Sahm D. In vitro activity of imipenem–relebactam (MK-7655) against Enterobacteriaceae from United States ICU and Non-ICU wards-SMART 2015-2016 [abstract no. 2846 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Lob S, Hackel M, Badal R, Young K, Motyl M, Sahm D. In vitro activity of imipenem–relebactam (MK-7655) against P. aeruginosa from United States ICU and Non-ICU Wards-SMART 2015-2016 [abstract no. 2848 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Hackel M, Young K, Motyl M, Sahm D. In vitro activity of imipenem–relebactam (MK-7655) against Enterobacteriaceae and Pseudomonas aeruginosa from urinary tract infections in North America—SMART 2015 [abstract no. 1840]. Open Forum Infect Dis. 2016;3(Suppl. 1):S515. Plus poster presented at IDWeek; 2016; New Orleans.
Hackel M, Young K, Motyl M, Sahm D. In vitro activity of imipenem–relebactam (MK-7655) against Enterobacteriaceae and Pseudomonas aeruginosa from respiratory tract infections in North America—SMART 2015 [abstract no. 1839]. Open Forum Infect Dis. 2016;3(Suppl. 1):S515. Plus poster presented at IDWeek; 2016; New Orleans.
Hackel M, Young K, Motyl M, Sahm D. In vitro activity of imipenem–relebactam (MK-7655) against Enterobacteriaceae and Pseudomonas aeruginosa from intraabdominal infections in North America—SMART 2015 [abstract no. 1838]. Open Forum Infect Dis. 2016;3(Suppl. 1):S515. Plus poster presented at IDWeek; 2016; New Orleans.
Zhang Y, Carpenter J, Altalhi S, Bush K. In vitro susceptibility of imipenem–relebactam against recent carbapenemase-producing carbapenem-resistant Enterobacteriaceae (CP-CRE) isolates [abstract no. 2944 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Snydman DR, Jacobus NV, McDermott LA. In vitro evaluation of the activity of imipenem–relebactam against 451 recent clinical isolates of Bacteroides group and related species. Antimicrob Agents Chemother. 2016;60(10):6393–7.
Citron DM, Merriam CV, Tyrrell KL, Leoncio E, Goldstein EJC. The in vitro activity of relebactam, imipenem, and the combination of the two, plus six comparator antimicrobial agents against 432 strains of anaerobic bacteria including imipenem-resistant organisms [abstract no. 5138 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Papp-Wallace KM, Barnes MD, Alsop J, Taracila MA, Bethel CR, Becka SA, et al. Relebactam is a potent inhibitor of the KPC-2 β-lactamase and restores the susceptibility of imipenem against KPC-producing Enterobacteriaceae [abstract no. P1284 plus poster]. In: 27th European Congress of Clinical Microbiology and Infectious Diseases; 2017; Vienna.
Performance standards for antimicobial susceptibility testing. Clinical and Laboratory Standards Institute (CLSI). 2017. M100-S27. 2017.
Castanheira M, Huband MD, Mendes RE, Flamm RK. Meropenem–vaborbactam tested against contemporary Gram-negative isolates collected worldwide during 2014, including carbapenem-resistant, KPC-producing, multidrug-resistant, and extensively drug-resistant Enterobacteriaceae. Antimicrob Agents Chemother. 2017;AAC.00567-17 (in press).
Castanheira M, Rhomberg PR, Flamm RK, Jones RN. Effect of the β-lactamase inhibitor vaborbactam combined with meropenem against serine carbapenemase-producing Enterobacteriaceae. Antimicrob Agents Chemother. 2016;60(9):5454–8 (Plus supplemental material).
Castanheira M, Rhomberg PR, Watters AA, Jones RN. In vitro activity of meropenem/RPX7009, a carbapenem/β-lactamase inhibitor combination tested against contemporary populations of Enterobacteriaceae and KPC-producing strains [abstract no. 257]. Open Forum Infect Dis. 2014;1(Suppl. 1):S70. Plus poster presented at IDWeek; 2014; Philadelphia.
Huband MD, Flamm RK, Rhomberg PR, Jones RN, Castanheira M. In vitro antibacterial activity of meropenem/RPX7009, (a carbapenem/β-lactamase inhibitor combination) against contemporary Enterobacteriaceae isolated from intra-abdominal and urinary tract infections in the United States [abstract no. 781]. Open Forum Infect Dis. 2015;2(Suppl. 1):S149. Plus poster presented at IDWeek; 2015; San Diego.
Hackel M, Badal R, Sahm D. In vitro activity of meropenem–vaborbactam against isolates of KPC-producing Enterobacteriaceae collected worldwide in 2014–2015 [abstract no. 1830]. Open Forum Infect Dis. 2016;3(Suppl. 1):S515. Plus poster presented at IDWeek; 2016; New Orleans.
Hackel M, Badal R, Sahm D. In vitro activity of meropenem–vaborbactam against KPC-producing Enterobacteriaceae from Europe collected in 2014–2015 [abstract no. P1287 plus poster]. In: 27th European Congress of Clinical Microbiology and Infectious Diseases; 2017; Vienna.
Castanheira M, Mendes RE, Flamm RK, Jones RN. Activity of meropenem/RPX7009 and comparator agents tested against contemporary Enterobacteriaceae isolates collected from bloodstream infections in USA hospitals [abstract no C-152 plus poster]. In: 55th Interscience Conference of Antimicrobial Agents and Chemotherapy; 2015; San Diego.
Castanheira M, Woosley LN, Huband MD, Flamm RK. Meropenem–vaborbactam activity against Enterobacteriaceae isolates, including carbapenem-resistant and carbapenemase-producing isolates, collected in United States (US) hospitals during 2016. [abstract no. 2705 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Yang Q, Xu Y, Xu Z, Zhang G, Chen X. In vitro activity of meropenem combined with RPX7009 against Enterobacteriaceae producing KPC-type carbapenemases in China [abstract no. P1285 plus poster]. In: 27th European Congress of Clinical Microbiology and Infectious Diseases; 2017; Vienna.
Castanheira M, Huband MD, Flamm RK, Jones RN. Meropenem–vaborbactam (MER-VAB) tested against contemporary Enterobacteriaceae isolates from USA hospitals [abstract no. 452 plus poster]. In: ASM Microbe; 2016; Boston.
Weiss WJ, Pulse ME, Nguyen P, Peterson K, Silva J, Simecka JW, et al. Efficacy of Carbavance (meropenem + RPX7009) against carbapenem-resistant E. coli and K. pneumoniae in a murine UTI model [abstract no. B-078 plus poster]. In: 55th Interscience Conference of Antimicrobial Agents and Chemotherapy; 2015; San Diego.
Tarazi Z, Sabet M, Rubio-Aparicio D, Nolan T, Parkinson J, Dudley MN, et al. Meropenem–vaborbactam against highly carbapenem-resistant Enterobacteriaceae in an in vitro hollow fiber model using PK from phase 1 and phase 3 data in patients [abstract no. P1288 plus poster]. In: 27th European Congress of Clinical Microbiology and Infectious Diseases; 2017; Vienna.
Tarazi Z, Sabet M, Rubio-Aparicio D, Nolan T, Parkinson J, Lomovskaya O, et al. Efficacy of simulated human exposures of Carbavance (meropenem-RPX7009) against carbapenem-resistant Enterobacteriaceae in an in vitro hollow fiber model [abstract no. F-959 plus poster]. In: 54th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2014; Washington, D.C.
Lomovskaya O, Griffith DC, Loutit JS, Dudley MN. Rationale for dose selection for Carbavance (CVC; meropenem/RPX7009 in phase 3 trials [abstract no. 64E plus poster]. In: 19th Making A Difference in Infectious Diseases; 2016; Florida.
Griffith DC, Sabet M, Tarazi Z, Lomovskaya O, Dudley MN. Pharmacodynamics of vaborbactam when administered in combination with meropenem [abstract no. 5980 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Lala M, Brown M, Kantesaria B, Walker B, Paschke A, Rizk M. Population pharmacokinetic analysis of relebactam (REL) and imipenem in phase 1 healthy volunteers and phase 2 patients with complicated intra-abdominal infection (cIAI) [abstract no. A-040 plus poster]. In: 55th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2015; San Diego.
Butterton JR, Jumes P, Calder N, Rizk ML, Nefliu M, Sun P, et al. A phase I study evaluating the safety, tolerability, and pharmacokinetics of an intravenous beta-lactamase inhibitor in healthy male volunteers [abstract no. F1-1967 plus presentation]. In: 50th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2010; Boston.
Jumes P, Rizk ML, Calder N, Gutierrez M, Warrington S, Li X, et al. Phase I studies evaluating the safety, tolerability, and pharmacokinetics of multiple doses of an intravenous beta-lactamase inhibitor in healthy young males and single doses in healthy elderly male, elderly female and young female volunteers [abstract no. A-009 plus poster]. In: 52nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2012; San Francisco.
Rhee EG, Jumes PA, Gotfried MH, Rizk ML, Liu Y, Mangin E, et al. Intrapulmonary pharmacokinetics of MK-7655, a novel β-lactamase inhibitor, dosed in combination with imipenem/cilastatin in healthy subjects [abstract no. A-1028 plus poster]. In: 53th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2013; Denver.
Rizk ML, Jumes P, Lasseter K, Marbury T, Mangin E, Liu Y, et al. Pharmacokinetics of MK-7655, a novel β-lactamase inhibitor (BLI), in combination with imipenem/cilastatin (IPM/CIL) in subjects with impaired renal function [abstract no. A-010 plus poster]. In: 52nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2012; San Francisco.
Trang M, Griffith DC, Bhavnani SM, Loutit JS, Dudley MN, Ambrose PG, et al. Population pharmacokinetics of meropenem and vaborbactam in healthy volunteers and infected patients [abstract no. 2685 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Griffith DC, Rubino CM, Loutit JS, Morgan EE, White D, Dudley MN. A phase 1 study of the safety, tolerability, and pharmacokinetics of the beta-lactamase inhibitor RPX7009 alone, meropenem alone, and both in combination (Carbavance) TID for 7 days in healthy adult subjects [abstract no. 401]. Open Forum Infect Dis. 2014;1(Suppl. 1):S70. Plus poster presented at IDWeek; 2014; Philadephia.
Griffith DC, Loutit JS, Morgan EE, Durso S, Dudley MN. Phase 1 study of the safety, tolerability, and pharmacokinetics of the β-lactamase inhibitor vaborbactam (RPX7009) in healthy adult subjects. Antimicrob Agents Chemother. 2016;60(10):6326–32.
Wenzler E, Gotfried MH, Loutit JS, Durso S, Griffith DC, Dudley MN, et al. Meropenem-RPX7009 concentrations in plasma, epithelial lining fluid, and alveolar macrophages of healthy adult subjects. Antimicrob Agents Chemother. 2015;59(12):7232–9.
Powles MA, Galgoci A, Misura A, Liberator P, Hammond M. In vivo efficacy of the beta-lactamase inhibitor, MK-7655, in combination with imipenem in murine models of infection [abstract no. F1-2140 plus poster]. In: 50th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2010; Boston.
Bhagunde P, Chang K, Hirsch EB, Ledesma KR, Nikolaou M, Tam VH. Novel modeling framework to guide design of optimal dosing strategies for β-lactamase inhibitors. Antimicrob Agents Chemother. 2012;56(5):2237–40.
Wu J, Racine F, Rizk ML, Wismer MK, Harradine P, Young K, et al. Exploring PK/PD relationship of a novel beta-lactamase inhibitor MK-7655 in combination with imipenem in a hollow fiber infection model [abstract no. P1740 plus poster]. In: 24th European Congress of Clinical Microbiology and Infectious Diseases; 2014; Barcelona.
Lucasti C, Vasile L, Sandesc D, Venskutonis D, McLeroth P, Lala M, et al. Phase 2, dose-ranging study of relebactam with imipenem-cilastatin in subjects with complicated intra-abdominal infection. Antimicrob Agents Chemother. 2016;60(10):6234–43.
Tarazi Z, Sabet M, Rubio-Aparicio D, Sun D, Nolan T, Parkinson J, et al. Efficacy of simulated human exposures of meropenem compared to Carbavance (meropenem-RPX7009) against Pseudomonas aeruginosa in an in vitro hollow fiber model [abstract no. P1288 plus poster]. In: 25th European Congress of Clinical Microbiology and Infectious Diseases; 2015; Denmark.
Bhavnani SM, Hammel JP, Rubino CM, Trang M, Loutit JS, Griffith DC, et al. Meropenem–vaborbactam pharmacokinetic-pharmacodynamic analyses for efficacy based on data from patients enrolled in phase 3 studies [abstract no. 2834 plus poster]. In: 2nd ASM Microbe; 2017; New Orleans.
Sabet M, Tarazi Z, Nolan T, Parkinson J, Rubio-Aparicio D, Lomovskaya O, et al. In vivo efficacy of carbavance (meropenem/RPX7009) against KPC-producing Enterobacteriaceae [abstract no. F-958 plus poster]. In: 54th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2014; Washington, D.C.
Sims M, Mariyanovski V, McLeroth P, Akers W, Lee Y, Brown ML, et al. Prospective, randomized, double-blind, phase 2 dose-ranging study comparing efficacy and safety of imipenem/cilastatin plus relebactam with imipenem/cilastatin alone in patients with complicated urinary tract infections. J Antimicrob Chemother. 2017. (in press).
Bidair M, Zervos M, Sagan OS, Zaitsev V, Loutit J, Dudley M, et al. Clinical outcomes in adults with complicated urinary tract infections (cUTI), including acute pyelonephritis (AP) in TANGO 1, a phase 3 randomized, double-blind, double-dummy trial comparing meropenem–vaborbactam (M-V) with piperacillin-tazobactam (P-T) [abstract no. P1289 plus poster]. In: 27th European Congress of Clinical Microbiology and Infectious Diseases; 2017; Vienna.
Walsh TJ, Bhowmick T, Darouiche RO, Shorr A, Zaitsev VI, Perlin DS, et al. Per pathogen outcomes of meropenem–vaborbactam (M-V) versus piperacillin-tazobactam (P-T) in the treatment of adults with complicated urinary tract infections (cUTI), including acute pyelonephritis (AP), in TANGO 1, a phase 3 randomized, double-blind,. double-dummy trial [abstract no. P1290 plus poster]. In: 27th European Congress of Clinical Microbiology and Infectious Diseases; 2017; Vienna.
Kaye KS, Vazquez J, Mathers A, Daikos G, Alexander E, Loutit JS, et al. Clinical outcomes of serious infections due to carbapenem-resistant enterobacteriaceae (CRE) in TANGO II a phase 3 randomized multi-national open-label trial of meropenem–vaborbactam (M-V) versus best available therapy (BAT). [abstract no. 1862]. In: IDWeek; 2017; San Diego.
Paterson D, Kwak EJ, Bhowmick T, Alexander E, Loutit JS, et al. Meropenem–vaborbactam vs. best available therapy for carbapenem-resistant enterobacteriaceae infections in TANGO II: Outcomes in immunocompromised patients. [abstract no. 1868]. In: IDWeek; 2017; San Diego.
Primaxin® product monograph. New Jersey: Merck Sharp & Dohme Corporation, a subsidiary of Merck & Company, Incorporated, 2016.
Merrem® product monograph. Ontario: AstraZeneca Canada Incorporated, 2017.
Acknowledgements
The authors would like to thank Pia Graham from Merck and Dr. Niki Patel from The Medicines Company for their efforts obtaining published literature on imipenem–relebactam and meropenem–vaborbactam, respectively.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this manuscript.
Conflict of interest
George Zhanel and Daryl Hoban have both received research grant funding from Merck and The Medicines Company. Courtney Lawrence, Heather Adam, Frank Schweizer, Sheryl Zelenitsky, Michael Zhanel, Philippe Lagacé-Wiens, Andrew Walkty, Andrew Denisuik, Alyssa Golden, Alfred Gin, Joseph Lynch and James Karlowsky have no conflicts to declare.
Rights and permissions
About this article
Cite this article
Zhanel, G.G., Lawrence, C.K., Adam, H. et al. Imipenem–Relebactam and Meropenem–Vaborbactam: Two Novel Carbapenem-β-Lactamase Inhibitor Combinations. Drugs 78, 65–98 (2018). https://doi.org/10.1007/s40265-017-0851-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-017-0851-9