Abstract
Objectives
On the basis of a systematic review, we aimed to establish the cost and drivers of cost and/or resource use of intra- and perioperative complications occurring as a result of selected major surgical procedures, as well as to understand the relationship between costs and severity of complication and, consequently, the economic burden they represent. We also assessed the clinical and economic methodologies used to derive costs and resource use across the studies with a view to providing guidance on reporting standards for these studies.
Methods
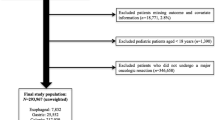
We searched EMBASE, MEDLINE and Econlit (from 2002 to 2012) for study publications including resource use/cost data relating to surgical complications.
Results
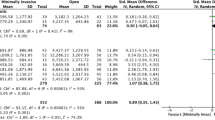
We identified 38 relevant studies on pancreatic (n = 14), urologic (n = 4), gynaecological (n = 6), thoracic (n = 13) and hepatic surgery (n = 1). All studies showed that complications lead to higher resource use and hospital costs compared with surgical procedures without complications. Costs depend on type of complication and complication severity, and are driven primarily by prolonged hospitalisation. There was considerable heterogeneity between studies with regard to patient populations, outcomes and procedures, as well as a lack of consistency and transparency of reporting of costs/resource use. Complication severity grading systems were used infrequently.
Conclusions
The overall conclusions of included studies are consistent: complications represent an important economic burden for health care providers. We conclude that more accurate and consistent data collection is required to serve as input for good-quality economic analyses, which in turn can inform hospital decisions on cost-efficient allocation of their limited resources.



Similar content being viewed by others
References
Bundesamt für Statistik. Kosten des Gesundheitswesens; 2010. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/themen/14/05/blank/key/ueberblick.html. Accessed Nov 2012.
Institut national de la statistique et des études économiques. Depense courante de santé en; 2011. Available from: http://www.insee.fr/fr/themes/tableau.asp?reg_id=0&ref_id=NATTEF06305. Accessed Nov 2012.
Centers for Medicare & Medicaid Services. National health expenditure projections 2011–2021. Available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/Proj2011PDF.pdf. Accessed Jun 2013.
Khuri SF, Daley J, Henderson W, et al. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg. 1998;228:491–507.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Ergina PL, Cook JA, Blazeby JM, et al. Challenges in evaluating surgical innovation. Lancet. 2009;374:1097–104.
Barkun JS, Aronson JK, Feldman LS, et al. Evaluation and stages of surgical innovations. Lancet. 2009;374:1089–96.
McCulloch P, Altman DG, Campbell WB, et al. No surgical innovation without evaluation: the IDEAL recommendations. Lancet. 2009;374:1105–12.
Vonlanthen R, Slankamenac K, Breitenstein S, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg. 2011;254:907–13.
Handy JR Jr, Denniston K, Grunkemeier GL, et al. What is the inpatient cost of hospital complications or death after lobectomy or pneumonectomy? Ann Thorac Surg. 2011;91:234–8.
Yu HY, Hevelone ND, Lipsitz SR, et al. Hospital volume, utilization, costs and outcomes of robot-assisted laparoscopic radical prostatectomy. J Urol. 2012;187:1632–7.
Nagel M, Gemmen E, Smith B, et al. Assessment of the clinical and economic impact of air leaks during post-operative pulmonary surgery. Presented at the 2010 15th annual International Society for Pharmacoeconomics and Outcomes research meeting, PRS18; 2010.
Spotnitz WD. Hemostats, sealants, and adhesives: a practical guide for the surgeon. Am Surg. 2012;78:1305–21.
Spotnitz WD, Burks S. State-of-the-art review: hemostats, sealants, and adhesives II: update as well as how and when to use the components of the surgical toolbox. Clin Appl Thromb Hemost. 2010;16:497–514.
Spotnitz WD, Burks S. Hemostats, sealants, and adhesives III: a new update as well as cost and regulatory considerations for components of the surgical toolbox. Transfusion. 2012;52:2243–55.
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration; 2011.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Breitenstein S, DeOliveira ML, Raptis DA, et al. Novel and simple preoperative score predicting complications after liver resection in noncirrhotic patients. Ann Surg. 2010;252:726–34.
Daskalaki D, Butturini G, Molinari E, et al. A grading system can predict clinical and economic outcomes of pancreatic fistula after pancreaticoduodenectomy: results in 755 consecutive patients. Langenbecks Arch Surg. 2011;396:91–8.
Kent TS, Sachs TE, Callery MP, et al. Readmission after major pancreatic resection: a necessary evil? J Am Coll Surg. 2011;213:515–23.
Pratt WB, Callery MP, Vollmer CM Jr. The latent presentation of pancreatic fistulas. Br J Surg. 2009;96:641–9.
Rodriguez JR, Germes SS, Pandharipande PV, et al. Implications and cost of pancreatic leak following distal pancreatic resection. Arch Surg. 2006;141:361–5; discussion 66.
Topal B, Peeters G, Vandeweyer H, et al. Hospital cost-categories of pancreaticoduodenectomy. Acta Chir Belg. 2007;107:373–7.
Vanounou T, Pratt WB, Callery MP, et al. Selective administration of prophylactic octreotide during pancreaticoduodenectomy: a clinical and cost-benefit analysis in low- and high-risk glands. J Am Coll Surg. 2007;205:546–57.
Coello R, Charlett A, Wilson J, et al. Adverse impact of surgical site infections in English hospitals. J Hosp Infect. 2005;60:93–103.
de Lissovoy G, Fraeman K, Hutchins V, et al. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009;37:387–97.
Gunnarsson C, Rizzo JA, Hochheiser L. The effects of laparoscopic surgery and nosocomial infections on the cost of care: evidence from three common surgical procedures. Value Health. 2009;12:47–54.
Rotermann M. Infection after cholecystectomy, hysterectomy or appendectomy. Health Rep. 2004;15:11–23.
Pilling JE, Martin-Ucar AE, Waller DA. Salvage intensive care following initial recovery from pulmonary resection: is it justified? Ann Thorac Surg. 2004;77:1039–44.
Roselli EE, Murthy SC, Rice TW, et al. Atrial fibrillation complicating lung cancer resection. J Thorac Cardiovasc Surg. 2005;130:438–44.
Varela G, Jimenez MF, Novoa N, et al. Estimating hospital costs attributable to prolonged air leak in pulmonary lobectomy. Eur J Cardiothorac Surg. 2005;27:329–33.
Rapoport J, Teres D, Lemeshow S, et al. Explaining variability of cost using a severity-of-illness measure for ICU patients. Med Care. 1990;28:338–48.
Casadei R, Ricci C, Pezzilli R, et al. Assessment of complications according to the Clavien-Dindo classification after distal pancreatectomy. JOP. 2011;12:126–30.
Jimenez RE, Mavanur A, Macaulay WP. Staple line reinforcement reduces postoperative pancreatic stump leak after distal pancreatectomy. J Gastrointest Surg. 2007;11:345–9.
Seely AJ, Ivanovic J, Threader J, et al. Systematic classification of morbidity and mortality after thoracic surgery. Ann Thorac Surg. 2010;90:936–42; discussion 42.
Stolz AJ, Schutzner J, Lischke R, et al. Predictors of prolonged air leak following pulmonary lobectomy. Eur J Cardiothorac Surg. 2005;27:334–6.
Behrman SW, Zarzaur BL. Intra-abdominal sepsis following pancreatic resection: incidence, risk factors, diagnosis, microbiology, management, and outcome. Am Surg. 2008;74:572–8; discussion 78–9.
Belyaev O, Munding J, Herzog T, et al. Histomorphological features of the pancreatic remnant as independent risk factors for postoperative pancreatic fistula: a matched-pairs analysis. Pancreatology. 2011;11:516–24.
Fuks D, Piessen G, Huet E, et al. Life-threatening postoperative pancreatic fistula (grade C) after pancreaticoduodenectomy: incidence, prognosis, and risk factors. Am J Surg. 2009;197:702–9.
Glowka TR, Kalff JC, Pantelis D, et al. Secondary surgery subsequent to distal pancreatectomy. Hepatogastroenterology. 2010;57:952–6.
Haddad LB, Scatton O, Randone B, et al. Pancreatic fistula after pancreaticoduodenectomy: the conservative treatment of choice. HPB (Oxford). 2009;11:203–9.
Simons JP, Shah SA, Ng SC, et al. National complication rates after pancreatectomy: beyond mere mortality. J Gastrointest Surg. 2009;13:1798–805.
Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13.
Bartsch GC, Kuefer R, Braun C, et al. Nosocomial bacteriuria in patients with indwelling catheter after radical retropubic prostatectomy for prostate cancer. Urol Int. 2008;81:389–93.
Guillonneau B, Gupta R, El Fettouh H, et al. Laparoscopic [correction of laproscopic] management of rectal injury during laparoscopic [correction of laproscopic] radical prostatectomy. J Urol. 2003;169:1694–6.
Treiyer A, Haben B, Stark E, et al. Uni- vs. multiloculated pelvic lymphoceles: differences in the treatment of symptomatic pelvic lymphoceles after open radical retropubic prostatectomy. Int Braz J Urol. 2009;35:164–9; discussion 70.
Aaronson DS, Wu AK, Blaschko SD, et al. National incidence and impact of noninfectious urethral catheter related complications on the Surgical Care Improvement Project. J Urol. 2011;185:1756–60.
Duong TH, Gellasch TL, Adam RA. Risk factors for the development of vesicovaginal fistula after incidental cystotomy at the time of a benign hysterectomy. Am J Obstet Gynecol. 2009;201(512):e1–4.
Antanavicius G, Lamb J, Papasavas P, et al. Initial chest tube management after pulmonary resection. Am Surg. 2005;71:416–9.
Bardell T, Petsikas D. What keeps postpulmonary resection patients in hospital? Can Respir J. 2003;10:86–9.
Dulu A, Pastores SM, Park B, et al. Prevalence and mortality of acute lung injury and ARDS after lung resection. Chest. 2006;130:73–8.
Ghosh S, Steyn RS, Marzouk JF, et al. The effectiveness of high dependency unit in the management of high risk thoracic surgical cases. Eur J Cardiothorac Surg. 2004;25:123–6.
Ishikawa S, Griesdale DE, Lohser J. Acute kidney injury after lung resection surgery: incidence and perioperative risk factors. Anesth Analg. 2012;114:1256–62.
Liberman M, Muzikansky A, Wright CD, et al. Incidence and risk factors of persistent air leak after major pulmonary resection and use of chemical pleurodesis. Ann Thorac Surg. 2010;89:891–7; discussion 97–8.
Okereke I, Murthy SC, Alster JM, et al. Characterization and importance of air leak after lobectomy. Ann Thorac Surg. 2005;79:1167–73.
Kassin MT, Owen RM, Perez SD, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215:322–30.
Drummond M, Griffin A, Tarricone R. Economic evaluation for devices and drugs: same or different? Value Health. 2009;12:402–4.
Association of Surgeons of Great Britain, Royal College of Surgeons in Ireland. Consensus statement on cost-effective and sustainable Surgery; 2012. Available from: http://www.asgbi.org.uk/en/publications/consensus_statements.cfm. Accessed Apr 2013.
Association of Surgeons of Great Britain and Ireland. Issues in professional practice: guidelines for implementation of enhanced recovery protocols; 2009. Available from: http://www.asgbi.org.uk/en/publications/issues_in_professional_practice.cfm. Accessed Apr 2013.
Bratzler DW, Hunt DR. The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis. 2006;43:322–30.
Fitzgerald J, Kanter G, Trelease R, et al. Reducing surgical complications. Nurs Manag. 2007;38:35–9.
National Institute for Health and Clinical Excellence. CG74: surgical site infection—prevention and treatment of surgical site infection; 2008. Available from: http://www.nice.org.uk/nicemedia/pdf/CG74NICEGuideline.pdf. Accessed Apr 2013.
American College of Surgeons National Surgical Quality Improvement Program. About ACS NSQIP. Available from: http://site.acsnsqip.org/about/. Accessed Apr 2013.
Hall BL, Hamilton BH, Richards K, et al. Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: an evaluation of all participating hospitals. Ann Surg. 2009;250:363–76.
Tennessee Surgical Quality Collaborative. Available from: http://www.tnsqc.com/. Accessed Apr 2013.
Guillamondegui OD, Gunter OL, Hines L, et al. Using the National Surgical Quality Improvement Program and the Tennessee Surgical Quality Collaborative to improve surgical outcomes. J Am Coll Surg. 2012;214:709–14; discussion 14–6.
Eappen S, Lane BH, Rosenberg B, et al. Relationship between occurrence of surgical complications and hospital finances. JAMA. 2013;309:1599–606.
Krupka DC, Sandberg WS, Weeks WB. The impact on hospitals of reducing surgical complications suggests many will need shared savings programs with payers. Health Aff (Millwood). 2012;31:2571–8.
Hashimoto Y, Traverso LW. Incidence of pancreatic anastomotic failure and delayed gastric emptying after pancreatoduodenectomy in 507 consecutive patients: use of a web-based calculator to improve homogeneity of definition. Surgery. 2010;147:503–15.
Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
Acknowledgments
This study was funded by Takeda Pharmaceuticals International GmbH, Zurich, Switzerland. Annika Bergman is an employee of Takeda. Ajay S. Patel and Brigitte W. Moore received honoraria from Takeda for conducting this systematic review and writing the article. Ulf Haglund has, on occasion, been contracted as a lecturer by Nycomed/Takeda, last in 2011. The authors thank Felicity Allen (FA) and Sarah Collins (SC), employees of Abacus International, who both received honoraria from Takeda, for their help with the selection of publications to be included.
Author contributions
Ajay Patel and Annika Bergman designed the systematic review and contributed to the presentation and analysis of results, as well as the discussion. Ajay Patel conducted screening of abstracts and full publications. Brigitte Moore and Ulf Haglund performed the analysis and presentation of results, as well as their interpretation for the discussion. Annika Bergman is the guarantor for the overall content.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Patel, A.S., Bergman, A., Moore, B.W. et al. The Economic Burden of Complications Occurring in Major Surgical Procedures: a Systematic Review. Appl Health Econ Health Policy 11, 577–592 (2013). https://doi.org/10.1007/s40258-013-0060-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-013-0060-y