Abstract
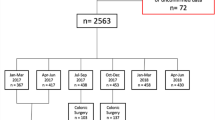
Improvements in living conditions and progress in medical management have resulted in better quality of life and longer life expectancy. Therefore, the number of older people undergoing surgery is increasing. Frailty is often described as a syndrome in aged patients where there is augmented vulnerability due to progressive loss of functional reserves. Studies suggest that frailty predisposes elderly to worsening outcome after surgery. Since emergency surgery is associated with higher mortality rates, it is paramount to have an accurate stratification of surgical risk in such patients. The aim of our study is to characterize the clinicopathological findings, management, and short-term outcome of elderly patients undergoing emergency surgery. The secondary objectives are to evaluate the presence and influence of frailty and analyze the prognostic role of existing risk-scores. The final FRAILESEL protocol was approved by the Ethical Committee of “Sapienza” University of Rome, Italy. The FRAILESEL study is a nationwide, Italian, multicenter, observational study conducted through a resident-led model. Patients over 65 years of age who require emergency surgical procedures will be included in this study. The primary outcome measures are 30-day postoperative mortality and morbidity rates. The Clavien-Dindo classification system is used to categorize complications. The secondary outcome measures include length of hospital stay, length of stay in intensive care unit, and predictive value for morbidity and mortality of several frailty and surgical risk-scores. The results of the FRAILESEL study will be disseminated through national and international conference presentations and peer-reviewed journals. The study is also registered at ClinicalTrials.gov (ClinicalTrials.gov identifier: NCT02825082).
Similar content being viewed by others

Abbreviations
- FRAILESEL:
-
Frailty and Emergency Surgery in the Elderly
- ERASO:
-
Elderly Risk Assessment and Surgical Outcome
- SICUT:
-
Società Italiana di Chirurgia d’Urgenza e del Trauma
- ACOI:
-
Associazione dei Chirurghi Ospedalieri Italiani
- SICG:
-
Società Italiana di Chirurgia Geriatrica SICE Società Italiana Chirurgia Endoscopica
- WSES:
-
World Society of Emergency Surgery
- DCC:
-
Data Coordination Center
- PI:
-
Principal Investigator
- ICD-9-CM:
-
Ninth revision of international classification of disease clinical modification
- P-POSSUM:
-
Portsmouth-Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity
- CR-POSSUM:
-
ColoRectal Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity
- SAPS II:
-
Simplified Acute Physiology Score II
- mFI:
-
Modified Frailty Index
- CACI:
-
Charlson Age-Comorbidity Index
References
United Nations, Department of Economic and Social Affairs, Population Division: World Population Ageing. (ST/ESA/SER.A/390).2015. Reference Source
Istat: Stime per l’anno 2016.2017. Reference Source
Costa G, La Torre M, Frezza B et al (2014) Changes in the surgical approach to colonic emergencies during a 15-year period. Dig Surg 31(3):197–203. https://doi.org/10.1159/000365254 (25170867)
Costa G, Nigri G, Tierno SM et al (2009) Emergency abdominal surgery in the elderly: a ten-year experience. BMC Geriatrics. https://doi.org/10.1186/1471-2318-9-s1-a53
Costa G, Tomassini F, Tierno SM et al (2009) Emergency colonic surgery: analysis of risk factors predicting morbidity and mortality. Chir Italy 61(5–6):565–571 (20380259)
Desserud KF, Veen T, Søreide K (2016) Emergency general surgery in the geriatric patient. Br J Surg 103(2):e52–e61. https://doi.org/10.1002/bjs.10044 (26620724)
McLean RC, McCallum IJ, Dixon S et al (2016) A 15-year retrospective analysis of the epidemiology and outcomes for elderly emergency general surgical admissions in the North East of England: A case for multidisciplinary geriatric input. Int J Surg 28:13–21. https://doi.org/10.1016/j.ijsu.2016.02.044 (26892599)
Shah AA, Zafar SN, Kodadek LM et al (2016) Never giving up: outcomes and presentation of emergency general surgery in geriatric octogenarian and nonagenarian patients. Am J Surg 212(2):211.e3–220.e3. https://doi.org/10.1016/j.amjsurg.2016.01.021 (27086200)
Hewitt J, McCormack C, Tay HS et al (2016) Prevalence of multimorbidity and its association with outcomes in older emergency general surgical patients: an observational study. BMJ Open 6(3):e010126. https://doi.org/10.1136/bmjopen-2015-0101264823401 (27033960)
Joseph B, Zangbar B, Pandit V et al (2016) Emergency general surgery in the elderly: too old or too frail? J Am Coll Surg 222(5):805–813. https://doi.org/10.1016/j.jamcollsurg.2016.01.063 (27113515)
Merani S, Payne J, Padwal RS et al (2014) Predictors of in-hospital mortality and complications in very elderly patients undergoing emergency surgery. World J Emerg Surg 9:43. https://doi.org/10.1186/1749-7922-9-43 (25050133)
St-Louis E, Sudarshan M, Al-Habboubi M et al (2016) The outcomes of the elderly in acute care general surgery. Eur J Trauma Emerg Surg 42(1):107–113. https://doi.org/10.1007/s00068-015-0517-9 (26038035)
Revenig LM, Canter DJ, Taylor MD et al (2013) Too frail for surgery? Initial results of a large multidisciplinary prospective study examining preoperative variables predictive of poor surgical outcomes. J Am Coll Surg 217(4):665.e1–670.e1. https://doi.org/10.1016/j.jamcollsurg.2013.06.012 (24054409)
Duron JJ, Duron E, Dugue T et al (2011) Risk factors for mortality in major digestive surgery in the elderly: a multicenter prospective study. Ann Surg 254(2):375–382. https://doi.org/10.1097/sla.0b013e318226a959 (21772131)
Igari K, Ochiai T, Yamazaki S (2013) POSSUM and P-POSSUM for risk assessment in general surgery in the elderly. Hepatogastroenterology 60(126):1320–1327
Karres J, Heesakkers NA, Ultee JM et al (2015) Predicting 30-day mortality following hip fracture surgery: evaluation of six risk prediction models. Injury 46(2):371–377. https://doi.org/10.1016/j.injury.2014.11.004 (25464983)
Mansmann U, Rieger A, Strahwald B et al (2016) Risk calculators-methods, development, implementation, and validation. Int J Colorectal Dis 31(6):1111–1116. https://doi.org/10.1007/s00384-016-2589-3 (27108006)
Poldermans D, Hoeks SE, Feringa HH (2008) Pre-operative risk assessment and risk reduction before surgery. J Am Coll Cardiol 51(20):1913–1924. https://doi.org/10.1016/j.jacc.2008.03.005 (18482658)
Scott S, Lund JN, Gold S et al (2014) An evaluation of POSSUM and P-POSSUM scoring in predicting post-operative mortality in a level 1 critical care setting. BMC Anesthesiol 14:104. https://doi.org/10.1186/1471-2253-14-104 (25469106)
Sutton R, Bann S, Brooks M et al (2002) The Surgical Risk Scale as an improved tool for risk-adjusted analysis in comparative surgical audit. Br J Surg 89(6):763–768 (12027988)
Tominaga T, Takeshita H, Takagi K et al (2016) E-PASS score as a useful predictor of postoperative complications and mortality after colorectal surgery in elderly patients. Int J Colorectal Dis 31(2):217–225. https://doi.org/10.1007/s00384-015-2456-7 (26607908)
Brooks MJ, Sutton R, Sarin S (2005) Comparison of Surgical Risk Score, POSSUM and p-POSSUM in higher-risk surgical patients. Br J Surg 92(10):1288–1292. https://doi.org/10.1002/bjs.5058 (15981213)
Chand M, Armstrong T, Britton G et al (2007) How and why do we measure surgical risk? J R Soc Med 100(11):508–512. https://doi.org/10.1177/014107680710001113 (18048708)
Scandrett KG, Zuckerbraun BS, Peitzman AB (2015) Operative risk stratification in the older adult. Surg Clin North Am 95(1):149–172. https://doi.org/10.1016/j.suc.2014.09.014 (25459549)
Turrentine FE, Wang H, Simpson VB et al (2006) Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg 203(6):865–877. https://doi.org/10.1016/j.jamcollsurg.2006.08.026
Bhangu A, Kolias AG, Pinkney T et al (2013) Surgical research collaboratives in the UK. Lancet 382(9898):1091–1092. https://doi.org/10.1016/s0140-6736(13)62013-9 (24075040)
van Rossem CC, Bolmers MD, Schreinemacher MH et al (2016) Prospective nationwide outcome audit of surgery for suspected acute appendicitis. Br J Surg 103(1):144–151. https://doi.org/10.1002/bjs.9964 (26509648)
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56(3):M146–M156. https://doi.org/10.1093/gerona/56.3.m146 (11253156)
NCEPOD Classification of Intervention (2004) Reference Source
von Elm E, Altman DG, Egger M et al (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013 (25046131)
Rockwood K, Fox RA, Stolee P et al (1994) Frailty in elderly people: an evolving concept. CMAJ 150(4):489–495 (8313261 1486322)
Rockwood K, Stadnyk K, MacKnight C et al (1999) A brief clinical instrument to classify frailty in elderly people. Lancet 353(9148):205–206. https://doi.org/10.1016/s0140-6736(98)04402-x (9923878)
Fried LP, Borhani NO, Enright P et al (1991) The Cardiovascular Health Study: design and rationale. Ann Epidemiol 1(3):263–276. https://doi.org/10.1016/1047-2797(91)90005-w (1669507)
Chen X, Mao G, Leng SX (2014) Frailty syndrome: an overview. Clin Interv Aging 9:433–441. https://doi.org/10.2147/cia.s45300 (24672230)
Clegg A, Young J, Iliffe S et al (2013) Frailty in elderly people. Lancet 381(9868):752–762. https://doi.org/10.1016/s0140-6736(12)62167-94098658 (23395245)
Hall DE, Arya S, Schmid KK et al (2017) Development and initial validation of the risk analysis index for measuring frailty in surgical populations. JAMA Surg 152(2):175–182. https://doi.org/10.1001/jamasurg.2016.4202 (27893030)
Hoogendijk EO, Theou O, Rockwood K et al (2016) Development and validation of a frailty index in the Longitudinal Aging Study Amsterdam. Aging Clin Exp Res. https://doi.org/10.1007/s40520-016-0689-0 (27896796)
Makary MA, Segev DL, Pronovost PJ et al (2010) Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 210(6):901–908. https://doi.org/10.1016/j.jamcollsurg.20 (20510798)
Orouji Jokar T, Ibraheem K, Rhee P et al (2016) Emergency general surgery specific frailty index: A validation study. J Trauma Acute Care Surg 81(2):254–260. https://doi.org/10.1097/ta.0000000000001120 (27257694)
Xue QL (2011) The frailty syndrome: definition and natural history. Clin Geriatr Med 27(1):1–15. https://doi.org/10.1016/j.cger.20 (21093718)
Partridge JS, Harari D, Dhesi JK (2012) Frailty in the older surgical patient: a review. Age Ageing 41(2):142–147. https://doi.org/10.1093/ageing/afr182 (22345294)
Lin HS, Watts JN, Peel NM et al (2016) Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr 16(1):157. https://doi.org/10.1186/s12877-016-0329-8 (27580947)
Amrock LG, Deiner S (2014) The implication of frailty on preoperative risk assessment. Curr Opin Anaesthesiol 27(3):330–335. https://doi.org/10.1097/aco.00000000000000654076287 (24566452)
Rockwood K, Mitnitski A (2011) Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med 27(1):17–26. https://doi.org/10.1016/j.cger.20 (21093719)
Søreide K, Desserud KF (2015) Emergency surgery in the elderly: the balance between function, frailty, fatality and futility. Scand J Trauma Resusc Emerg Med 23:10. https://doi.org/10.1186/s13049-015-0099-x (25645443)
Chimukangara M, Helm MC, Frelich MJ et al (2017) A 5-item frailty index based on NSQIP data correlates with outcomes following paraesophageal hernia repair. Surg Endosc 31(6):2509–2519. https://doi.org/10.1007/s00464-016-5253-75378684 (27699515)
Mogal H, Vermilion SA, Dodson R et al (2017) Modified Frailty Index predicts morbidity and mortality after pancreaticoduodenectomy. Ann Surg Oncol 24(6):1714–1721. https://doi.org/10.1245/s10434-016-5715-0 (28058551)
Wahl TS, Graham LA, Hawn MT et al (2017) Association of the Modified Frailty Index with 30-day surgical readmission. JAMA Surg. https://doi.org/10.1001/jamasurg.2017.1025 (28467535)
Velanovich V, Antoine H, Swartz A et al (2013) Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res 183(1):104–110. https://doi.org/10.1016/j.jss.2013.01.021 (23415494)
Louwers L, Schnickel G, Rubinfeld I (2016) Use of a simplified frailty index to predict Clavien 4 complications and mortality after hepatectomy: analysis of the National Surgical Quality Improvement Project database. Am J Surg 211(6):1071–1076. https://doi.org/10.1016/j.amjsurg.2015.09.015 (26800866)
Hubbard RE, Peel NM, Samanta M et al (2015) Derivation of a frailty index from the interRAI acute care instrument. BMC Geriatr 15:27. https://doi.org/10.1186/s12877-015-0026-z (25887105)
Revenig LM, Canter DJ, Kim S et al (2015) Report of a Simplified Frailty Score Predictive of Short-Term Postoperative Morbidity and Mortality. J Am Coll Surg 220(5):904-11.e1. https://doi.org/10.1016/j.jamcollsurg.2015.01.053 (25907870)
Gomes A, Rocha R, Marinho R et al (2015) Colorectal surgical mortality and morbidity in elderly patients: comparison of POSSUM, P-POSSUM, CR-POSSUM, and CR-BHOM. Int J Colorectal Dis 30(2):173–179. https://doi.org/10.1007/s00384-014-2071-z (25430595)
Abbas SM, Kahokehr A, Mahmoud M et al (2010) The Simple Prognostic Index (SPI)—a pathophysiologic prognostic scoring tool for emergency laparotomy. J Surg Res 163(2):e59–e65. https://doi.org/10.1016/j.jss.20 (20701926)
Miyazaki N, Haga Y, Matsukawa H et al (2014) Development and validation of the calculation of post-operative risk in emergency surgery (CORES) model. Surg Today 44(8):1443–1456. https://doi.org/10.1007/s00595-013-0707-1 (23996132)
Oliver CM, Walker E, Giannaris S et al (2015) Risk assessment tools validated for patients undergoing emergency laparotomy: a systematic review. Br J Anaesth 115(6):849–860. https://doi.org/10.1093/bja/aev350 (26537629)
Appendix list
List of ERASO Collaborative Study Group members on behalf of SICUT, ACOI, SICG, SICE, and the WSES Italian Chapter: Agresta F, Anania G, Ansaloni L, Antropoli M, Argenio G, Atzeni J, Avenia N, Azzinnaro A, Balani A, Baldazzi G, Balducci G, Barbera G, Bellanova G, Bergamini C, Bersigotti L, Bianchi PP, Bombardini C, Borzellino G, Bozzo S, Brachini G, Buccoliero F, Buonanno GM, Buononato M, Campanile FC, Canini T, Cardella S, Carrara G, Cascini F, Cassini D, Castriconi M, Catalini G, Catena F, Ceccarelli G, Celi D, Ceresoli M, Chiarugi M, Cillara N, Cimino F, Cobuccio L, Coccolini F, Cocorullo G, Colangelo E, Costa G, Crafa F, Crucitti A, Dalla Caneva P, De Luca M, de Manzoni Garberini A, De Nisco C, De Sol A, Falcioni T, Falco N, Farina C, Filippone G, Finotti E, Fiume S, Fontana T, Francioni G, Fransvea P, Frezza B, Gemini S, Genna M, Giannessi S, Gioffrè A, Giordano A, Gozzo D, Grimaldi S, Gulotta G, Iarussi T, Laterza E, Lepre L, Lorenzon L, Lotti R, Luridiana G, Marini P, Marzaioli R, Massa G, Mingoli A, Mulas S, Nagliati C, Nigri G, Niolu P, Noviello A, Occhionorelli S, Paderno N, Palini GM, Paradies D, Paroli M, Perrone F, Petruzzelli L, Pezzolla A, Piazza D, Piazza V, Piccoli M, Pisanu A, Podda M, Poillucci G, Porfidia R, Rossi G, Ruscelli P, Santella S, Sartelli M, Spagnoli A, Sulis R, Tarasconi A, Tranà C, Travaglino A, Valeri A, Vasquez G, Zago M, Zanoni E.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
No competing interests were disclosed.
Research involving Human Participants and/or Animals
The final FRAILESEL protocol was approved by the Ethics Committee of the “Sapienza” University of Rome, Italy on 12/12/2016 (allocated under approval number 4252_2016). Secondary approval has been obtained from all Ethics Committees of the other participating centers. The DCC provided assistance to each participating center during their local IRB application.
Informed consent
Informed consent was obtained from all individual participants included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Grant information
The author(s) declared that no Grants were involved in supporting this work.
Additional information
Members of ERASO (Elderly Risk Assessment for Surgical Outcome) Collaborative Study Group are listed in the Appendix list.
Rights and permissions
About this article
Cite this article
Costa, G., Massa, G. & ERASO (Elderly Risk Assessment for Surgical Outcome) Collaborative Study Group. Frailty and emergency surgery in the elderly: protocol of a prospective, multicenter study in Italy for evaluating perioperative outcome (The FRAILESEL Study). Updates Surg 70, 97–104 (2018). https://doi.org/10.1007/s13304-018-0511-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-018-0511-y