Abstract
Aim/Objective
Peripartum cardiomyopathy (PPCM) is a disorder of unknown etiology in which symptoms of heart failure occur between the last month of pregnancy and 5 months post-partum. These findings prompted us to carry out a more detailed study aimed at correlating plasma levels of C-reactive protein TNF-α and IL-6 as prognostic value for major clinical in-hospital events and 6-month follow-up in patients with PPCM.
Materials and Methods
After ethical clearance, in the present prospective case–control study, a total of 86 subjects were enrolled [patients (n = 46) and controls (n = 40)]. After checking for the inclusion and exclusion criteria, informed consent was obtained and patients were enrolled. The details of history of pre-eclampsia and mode of delivery were obtained from the patients. The history of onset of symptoms and signs was recorded at the first presentation and at 6 months. Clinical assessment, echocardiography, and blood analysis were done at baseline and after 6 months of standard therapy. All patients received treatment with diuretics and the ACE inhibitor (ramipril), Carvedilol if not contraindicated, and inotropic support inj-Dobutamine. Inflammatory markers (C-reactive protein, TNF-α, and IL-6) were measured at baseline and at 6 months. Data were analyzed using the SAS version 9.1 statistical program.
Results
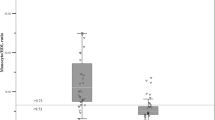
The characteristics of the study population at first presentation to the cardiac clinic are similar (compared with controls): 0.91 % of the study patients were diagnosed as PPCM patients for the first time and 49 % patients presented within one month after delivery. C-reactive protein (22 vs 08 mg/dl, p < 0.05), TNF-α (9.6 vs 3.2 pg/dl, p < 001), and IL-6 (73.19 ± 34.4 vs 31.52 ± 8.83 pg/dl, p < 0.005) were significantly abnormal, and these patients showed significantly higher LV dimensions, LV EDD (61.6 ± 7.1 vs 46 ± 9 mm p < 0.004) LV ESD (53.1 ± 7 vs 32 ± 8, p < 0.005), and significantly lower echocardiographic left ventricular ejection fraction (LVEF) (25.9 ± 8.2 vs 55 ± 12 p < 0.001) and correlate well with NYHA FC and death. LVEF improved from 25.9 ± 8.2 to 42.9 + 13.6 % at 6 months (p < 0.0001). Patients who completed 6 months of standard care showed a significant reduction of heart rate, LV dimensions, and NYHA FC (p < 0.001). However, normalization of LVEF (>50 %) was only observed in 11 (35 %) patients. Seven patients died within 6 months of diagnoses and eight patients were lost to follow-up.
Conclusions
Plasma markers of inflammation were significantly elevated in PPCM patients and correlated with increased LV dimensions and lower EF at presentation. Baseline CRP, IL-6, TNF-α, and higher NYHA FC were the only predictors of mortality. These results contribute to inflammation which may contribute to the pathogenesis of PPCM and its complications and predictors of mortality.


Similar content being viewed by others
References
Pearson GD, Veille JC, Rahimtoola S. Peripartum cardiomyopathy: National Institutes of Health workshop recommendations and review. JAMA. 2000;283:262–7.
Reimold S, Rutherford J. Peripartum cardiomyopathy. N Engl J Med. 2000;344:1629–30.
Lampert M, Lang RM. Peripartum cardiomyopathy. Am Heart J. 1995;130:860–70.
Demakis JG, Rahimtoola SH, Sutton GC. Natural course of peripartum cardiomyopathy. Circulation. 1971;44:1053–61.
Sato Y, Takatsu Y, Kataoka K. Serial circulating concentrations of C-reactive protein, interleukin-4, and IL-6 in patients with acute left heart decompensation. Clin Cardiol. 1999;22:811–3.
Kanebo K, Kanada T, Yamauchi Y. C-reactive protein in dilated cardiomyopathy. Cardiology. 1999;91:215–9.
Hayakawa Y, Chandra M, Wenfeng M, et al. Inhibition of cardiac myocyte apoptosis improves cardiac function and abolishes mortality in peripartum cardiomyopathy of Galpha(q) transgenic mice. Circulation. 2003;108:1037–42.
Sliwa K, Skudicky D, Bergemann A. The addition of pentoxifylline to conventional therapy improves outcome in patients with peripartum cardiomyopathy. Eur J Heart Fail. 2002;4:305–9.
Sliwa K, Skudicky D, Bergemann A. Peripartum cardiomyopathy: analysis of clinical outcome, left ventricular function, plasma levels of cytokines and Fas/APO-1. J Am Coll Cardiol. 2000;35(3):701–5.
Ansari A, Fett JD, Carraway RE. Autoimmune mechanisms as the basis for human peripartum cardiomyopathy. Clin Rev Allergy Immunol. 2002;23(3):301–24.
Felker GM, Thompson R, Joshua MH. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000;342:1077–84.
Rauchhaus M, Clark AL, Doehner W. The relationship between cholesterol and survival in patients with chronic heart failure. J Am Coll Cardiol. 2003;42:1933–40.
Horwich TB, Hamilton MA, Fonarow GC. Low serum cholesterol is associated with marked increase in mortality in advanced heart failure. J Card Fail. 2002;8:216–24.
Narula J, Haider N, Virmani R. Apoptosis in myocytes in end-stage heart failure. N Engl J Med. 1996;335:1182–9.
Sahn DJ, DeMaria A, Kisslo J. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978;58:1072–83.
Hu CL, Li YB, Zou YG, et al. Troponin T measurement can predict persistent left ventricular dysfunction in peripartum cardiomyopathy. Heart. 2007;93(4):488–90.
Amos AM, Jaber WA, Russell SD. Improved outcomes in peripartum cardiomyopathy with contemporary. Am Heart J. 2006;152(3):509–13.
Cole P, Cook F, Plappert T. Longitudinal changes in left ventricular architecture and function in peripartum cardiomyopathy. Am J Cardiol. 1987;60(10):871–6.
Hameed A, Elkayam U. Peripartum cardiomyopathy. In: Crawford M, DiMarco J, editors. Cardiology. 1st ed. London: Mosby; 2001. p. 513.1.
Rauchhaus M, Coats AJS, Anker SD. The endotoxin-lipoprotein hypothesis. Lancet. 2000;346:930–3.
Sliwa K, Forster O, Zhanje F. Outcome of subsequent pregnancy in patients with documented peripartum cardiomyopathy. Am J Cardiol. 2004;93:1441–3.
Ansari AA, Fett JD, Carraway RE. Autoimmune mechanism as the basis for human peripartum cardiomyopathy. Clin Rev Allergy Immunol. 2002;23:301–24.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sarojini, A., Sai Ravi Shanker, A. & Anitha, M. Inflammatory Markers-Serum Level of C-Reactive Protein, Tumor Necrotic Factor-α, and Interleukin-6 as Predictors of Outcome for Peripartum Cardiomyopathy. J Obstet Gynecol India 63, 234–239 (2013). https://doi.org/10.1007/s13224-013-0428-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-013-0428-9