Abstract
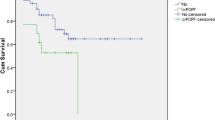
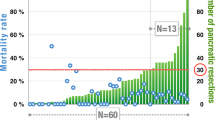
With advances in surgical management of pancreaticoduodenectomy (PD), mortality rate for PD has been reported to be less than 5%. Postoperative pancreatic fistula (POPF) remains a major complication and morbidity after PD with incidence of up to 40%. This is a retrospective analysis of patients who underwent PD in a tertiary cancer referral center in southern India. Data was collected for the patients operated during the period from Jan 2014 to Dec 2018. Surgicopathological, oncological, and survival outcomes were described. Of 76 patients presumed as operable, 16 were excluded and data analyzed for 60 patients. Forty-four percent underwent classical Whipple’s PD and 56% pylorus-preserving PD. The most common postoperative complications were wound infection (25%); pneumonia (20%); clinically relevant POPF (13%); and delayed gastric emptying (19%). Thirty-day in-hospital mortality was 5%, 90-day mortality was 8.3%, and fistula-related mortality was 1.6%. Ampullary cancer was the most common histology. Three-year survival rate was 23.3% with a mean overall survival of 33.2 months with significantly better survival in the node negative than positive group (41.3 vs 20.5 months, P = 0.003) and significantly lower survival in pancreatic head cancer than other tumor histologies (16.6 vs 37.3 months, P = 0.002). Multivariate analysis has shown pancreatic head histology (HR = 2.38, 95% CI (1.08–5.26), P = 0.033) and nodal positivity (HR = 2.38, 95% CI (1.27–4.44), P = 0.007) as poor prognostic factors. Pancreaticoduodenectomy is a safe operation in experienced hands. Adhering to a meticulous adaptable reproducible anastomotic technique with standard perioperative management strategies significantly decreases the operative morbidity and mortality.

Similar content being viewed by others
Data Availability
Yes.
References
Whipple AO (1945) Pancreaticoduodenectomy for islet carcinoma: a five-year follow-up. Ann Surg. 121:847–852. https://doi.org/10.1097/00000658-194506000-00008
Shrikhande SV, Barreto G, Shukla PJ (2008) Pancreatic fistula after pancreaticoduodenectomy: the impact of a standardized technique of pancreaticojejunostomy. Langenbecks Arch Surg. 393:87–91. https://doi.org/10.1007/s00423-007-0221-2
Yamashita Y, Yoshizumi T, Fukuzawa K et al (2016) Surgical results of pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: a multi-institutional retrospective study of 174 patients. Anticancer Res 36:2407–2412
Z’graggen K, Uhl W, Friess H, Büchler MW (2002) How to do a safe pancreatic anastomosis. J Hepatobiliary Pancreat Surg 9:733–7. https://doi.org/10.1007/s005340200101
Shrikhande SV, Kleeff J, Büchler MW, Friess H (2007) Pancreatic anastomosis after pancreaticoduodenectomy: how we do it. Indian J Surg. 69:224–9. https://doi.org/10.1007/s12262-007-0031-3
Bassi C, Marchegiani G, Dervenis C et al. (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 161:584 91. https://doi.org/10.1016/j.surg.2016.11.014
Wente MN, Bassi C, Dervenis C et al. (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 142:761–8. https://doi.org/10.1016/j.surg.2007.05.005
Wente MN, Veit JA, Bassi C et al. (2007) Postpancreatectomy hemorrhage (PPH): An International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 142:20–5. https://doi.org/10.1016/j.surg.2007.02.001
Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr (2013) A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg 216:1–14. https://doi.org/10.1016/j.jamcollsurg.2012.09.002
Miller BC, Christein JD, Behrman SW et al. (2014) A multi-institutional external validation of the fistula risk score for pancreatoduodenectomy. J Gastrointest Surg. 18:172–79; discussion 179–80. https://doi.org/10.1007/s11605-013-2337-8
McClusky DA, Skandalakis LJ, Colborn GL, Skandalakis JE (2002) Harbinger or hermit? Pancreatic anatomy and surgery through the ages--part 1. World J Surg. 26(9):1175–85. https://doi.org/10.1007/s00268-002-1238-x
Schnelldorfer T, Adams DB, Warshaw AL, Lillemoe KD, Sarr MG (2008) Forgotten pioneers of pancreatic surgery: beyond the favorite few. Ann Surg. 247:191–202. https://doi.org/10.1097/SLA.0b013e3181559a97
Whipple AO, Parsons WB, Mullins CR (1935) Treatment of carcinoma of the ampulla of Vater. Ann Surg. 102:763–79. https://doi.org/10.1097/00000658-193510000-00023
Whipple AO (1946) Observations on radical surgery for lesions of the pancreas. Surg Gynecol Obstet 82:623–631
Cameron JL, Pitt HA, Yeo CJ, Lillemoe KD, Kaufman HS, Coleman J (1993) One-hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg. 217:430–38. https://doi.org/10.1097/00000658-199305010-00002
Ji W, Shao Z, Zheng K et al. (2015) Pancreaticojejunostomy with double-layer continuous suturing is associated with a lower risk of pancreatic fistula after pancreaticoduodenectomy: a comparative study. Int J Surg. 13:84–89. https://doi.org/10.1016/j.ijsu.2014.11.034
Bassi C, Butturini G, Molinari E et al. (2004) Pancreatic fistula rate after pancreatic resection. The importance of definitions. Dig Surg. 21:54–9. https://doi.org/10.1159/000075943
Barreto SG, Shukla PJ (2017) Different types of pancreatico-enteric anastomosis. Transl Gastroenterol Hepatol. 2:89. https://doi.org/10.21037/tgh.2017.11.02
Torres OJM, Costa RCNDC, Costa FFM et al. (2017) Modified Heidelberg technique for pancreatic anastomosis. Arq Bras Cir Dig. 30:260–63. https://doi.org/10.1590/0102-6720201700040008
Ecker BL, McMillan MT, Asbun HJ et al. (2018) Characterization and optimal management of high-risk pancreatic anastomoses during pancreatoduodenectomy. Ann Surg. 267:608–16. https://doi.org/10.1097/SLA.0000000000002327
Shrikhande SV, Sivasanker M, Vollmer CM et al. (2017) Pancreatic anastomosis after pancreatoduodenectomy: a position statement by International Study Group of Pancreatic Surgery (ISGPS). Surgery. 161:1221–34. https://doi.org/10.1016/j.surg.2016.11.021
Lin JW, Cameron JL, Yeo CJ, Riall TS, Lillemoe KD (2004) Risk factors and outcomes in postpancreaticoduodenectomy pancreaticocutaneous fistula. J Gastrointest Surg. 8:951–9. https://doi.org/10.1016/j.gassur.2004.09.044
Hanna MM, Gadde R, Allen CJ et al. (2016) Delayed gastric emptying after pancreaticoduodenectomy. J Surg Res. 202:380–8. https://doi.org/10.1016/j.jss.2015.12.053
El Nakeeb A, Askr W, Mahdy Y et al. (2015) Delayed gastric emptying after pancreaticoduodenectomy. Risk factors, predictors of severity and outcome. A single center experience of 588 cases. J Gastrointest Surg. 19:1093–100. https://doi.org/10.1007/s11605-015-2795-2
Velanovich V, Kheibek T, Khan M (2009) Relationship of postoperative complications from preoperative biliary stents after pancreaticoduodenectomy. A new cohort analysis and meta-analysis of modern studies. JOP. 10(1):24–9.
Yeo CJ, Cameron JL, Maher MM et al. (1995) A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 222:580–8. https://doi.org/10.1097/00000658-199510000-00014
Büchler MW, Friess H, Wagner M, Kulli C, Wagener V, Z’Graggen K (2000) Pancreatic fistula after pancreatic head resection. Br J Surg. 87:883–89. https://doi.org/10.1046/j.1365-2168.2000.01465.x
Schlitt HJ, Schmidt U, Simunec D et al. (2002) Morbidity and mortality associated with pancreatogastrostomy and pancreatojejunostomy following partial pancreatoduodenectomy. Br J Surg. 89:1245–51. https://doi.org/10.1046/j.1365-2168.2002.02202.x
Schmidt CM, Powell ES, Yiannoutsos CT et al. (2004) Pancreaticoduodenectomy: a 20-year experience in 516 patients. Arch Surg. 139:718–25; discussion 725–7. https://doi.org/10.1001/archsurg.139.7.718
Grobmyer SR, Kooby D, Blumgart LH, Hochwald SN (2010) Novel pancreaticojejunostomy with a low rate of anastomotic failure-related complications. J Am Coll Surg. 210:54–9. https://doi.org/10.1016/j.jamcollsurg.2009.09.020
Caronna R, Peparini N, Cosimo Russillo G, Antonio Rogano A, Dinatale G, Chirletti P (2012) Pancreaticojejuno anastomosis after pancreaticoduodenectomy: brief pathophysiological considerations for a rational surgical choice. Int J Surg Oncol. 2012:636824. https://doi.org/10.1155/2012/636824
Kim M, Shin WY, Lee KY, Ahn SI (2017) An intuitive method of duct-to-mucosa pancreaticojejunostomy after pancreaticoduodenectomy: use of one-step circumferential interrupted sutures. Ann Hepatobiliary Pancreat Surg. 21:39–47. https://doi.org/10.14701/ahbps.2017.21.1.39
Cameron JL, Riall TS, Coleman J, Belcher KA (2006) One thousand consecutive pancreaticoduodenectomies. Ann Surg. 244(1):10–5. https://doi.org/10.1097/01.sla.0000217673.04165.ea.
van Roessel S, Mackay TM, Tol JAMG et al. (2019) Impact of expanding indications on surgical and oncological outcome in 1434 consecutive pancreatoduodenectomies. HPB (Oxford). 21(7):865–875. https://doi.org/10.1016/j.hpb.2018.10.020
Chen SC, Shyr YM, Wang SE (2013) Longterm survival after pancreaticoduodenectomy for periampullary adenocarcinomas. HPB (Oxford). 15(12):951–7. https://doi.org/10.1111/hpb.12071
Schnelldorfer T, Ware AL, Sarr MG et al. (2008) Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma: is cure possible? Ann Surg. 247(3):456–62. https://doi.org/10.1097/SLA.0b013e3181613142
Perysinakis I, Avlonitis S, Georgiadou D, Tsipras H, Margaris I (2015) Five-year actual survival after pancreatoduodenectomy for pancreatic head cancer. ANZ J Surg. 85(3):183–6. https://doi.org/10.1111/ans.12422.
Acknowledgements
We would like to thank all the residents of surgical oncology and anesthesia for making this publication possible.
Author information
Authors and Affiliations
Contributions
All authors had contributed on the conception and design, data acquisition and analysis, data interpretation, preparation of the manuscript, and its final approval.
Corresponding author
Ethics declarations
Ethics Approval
This study was conducted retrospectively from data obtained in course of common clinical practice in the treatment of cancers. We consulted extensively with the institutional review board of Kidwai Memorial Institute of Oncology, who determined that our study did not need ethical approval. The study protocol conforms to the ethical guidelines of the World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Fortaleza, Brazil, October 2013, and written informed consent was obtained from all patients before the proposed treatment and surgery.
Consent to Participate
All patients had consented for the proposed surgery and were explained about the nature of the disease, treatment options, outcomes, and need for regular follow-up.
Consent for Publication
All authors have consented for publication.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arjunan, R., Karthik, S., Chowdappa, R. et al. Contemporary Surgical, Oncological, and Survival Outcomes of Pancreaticoduodenectomy for Periampullary Tumours: a 5-Year Experience from Tertiary Cancer Center. Indian J Surg Oncol 12, 603–610 (2021). https://doi.org/10.1007/s13193-021-01385-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-021-01385-7