Abstract
Emotional dysregulation is increasingly recognized as a core feature of attention-deficit/hyperactivity disorder (ADHD). The purpose of the present systematic literature review was to identify published data related to the neuropsychology of emotional dysregulation in children with ADHD. The literature obtained is discussed in the contexts of deficits in emotional control, impairments in executive function, the emotional components of comorbidities, neurophysiological and autonomic correlates of emotional dysregulation, and the significance of multiple neuropsychological pathways of ADHD on emotional dysregulation. These various lines of evidence are used to create a patient-oriented conceptual model framework of the pathway from stimulus to inappropriate internalized (sadness, moodiness) or externalized (anger, aggressiveness) emotional responses. The article concludes by calling for continued research into the development of reliable and universally accepted measures of emotional dysregulation in order to provide children affected with ADHD, and their caregivers, some explanation for their emotional lability and, ultimately, to be used as tools to evaluate potential treatments.
Similar content being viewed by others
Introduction
Barry is a 10-year-old boy with attention-deficit/hyperactivity disorder (ADHD) who has been suspended from school. His father stays at home with him, but insists that Barry does a number of homework exercises. Barry understands the necessity and is doing the work, but becomes increasingly frustrated by the amount of work. Barry thinks he is doing the last exercise when his father indicates there is one more page of math to do. Barry’s heart starts to beat a little faster and he feels agitated. Just then the telephone rings; it is the school principal wishing to speak to Barry’s father about the suspension and reintegration process. Barry can hear only a little of the conversation but, already agitated, he becomes increasingly angry. His blood pressure rises, his face turns red, and he begins to throw things, first around his bedroom and then around the house. He yells and screams, disrupting the telephone call, and strikes out at his father in desperation. Finally, he retreats to his bedroom, destroying things along the route.
Equally, consider Rachel, a 7-year-old girl with the inattentive presentation of ADHD. Rachel is frustrated with not understanding some homework on which she is working. She feels overwhelmed by a project that is due in a few days. Rachel has kept her emotions inside, and her mother is not aware of her frustrations. Her mother asks her to clear the dinner table. Rachel does not respond at first, but when her mother asks her again, Rachel bursts into tears stating that her mother is always demanding so much of her.
ADHD is a neurodevelopmental disorder characterized by impulsivity, hyperactivity, and/or inattention according to the Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-5) (American Psychiatric Association 2013). It has been recognized for many years, however, that many children with ADHD exhibit low frustration tolerance and explosive behavior (Laufer et al. 1957) and, increasingly, there are calls to re-assess the characteristics of emotional impulsiveness and deficient emotional self-regulation as core features, rather than simply associated aspects of the disorder (Barkley 1997a, 2010). Indeed, the childhood manifestations of emotional dysregulation are important criteria of the Wender Utah Rating Scale used in the diagnosis of adult ADHD (Ward et al. 1993). Initial efforts to develop a unified model of ADHD proposed that impaired behavioral inhibition leads to deficits in executive neuropsychological functions that depend on such inhibition, including working memory, self-regulation of affect–motivation–arousal, internalization of speech, and reconstitution (behavioral analysis and synthesis) (Barkley 1997b), although others have argued that impaired behavioral inhibition and executive function are independent of each other (Rhodes et al. 2005). Based on a discovery-based community algorithm, Karalunas et al. (2014) proposed three subtypes of ADHD: mild (normative emotional regulation); surgent (extreme levels of positive-approach motivation); and irritable (extreme levels of negative emotionality, anger, and poor soothability) (Karalunas et al. 2014). The three subtypes were independent of existing clinical groupings, showed stability over time, and were distinguished by unique patterns of cardiac physiological response, resting-state functional brain connectivity, and clinical outcomes.
According to Barkley’s model (Barkley 1997a, b), the deficits in inhibition when individuals with ADHD are faced with emotionally charged situations lead to greater emotional reactivity or emotional dysregulation, compared with those without ADHD. Dysregulated emotion is characterized by excessive and rapidly shifting emotions, often associated with irritable and aggressive behavior (Stringaris 2011), and high rates of comorbid oppositional defiant disorder (Stringaris and Goodman 2009). For the purposes of the present review, we define emotional dysregulation as an inability to modulate emotional responses, resulting in extreme responses of an internalizing or externalizing nature that would be considered inappropriate for the developmental age of the person. In a recent review, the authors concluded that emotional dysregulation is highly prevalent in ADHD and is a major contributor to impairment, is associated with deficits in the recognition and/or allocation of attention to emotional stimuli, implicating deficits in the striato-amygdalo-medial prefrontal cortical network, and may be ameliorated by ADHD treatments (Shaw et al. 2014).
The purpose of the present article is to undertake a systematic literature review of clinical data relating to emotional dysregulation in children with ADHD, focusing on deficits in emotional inhibition and emotional self-regulation, and evidence of impaired executive function. To conclude, the article proposes a conceptual model of the construct of emotional dysregulation in ADHD and describes the importance of recognizing that emotional dysregulation is a common feature in children with ADHD.
Literature search
A PubMed search was performed on September 4, 2015, using the following terms: ((((((addh[MeSH Terms]) AND ((emotion OR emotional)) AND (regulation OR dysregulation))) AND Humans[Mesh] AND English[lang])) NOT review[Publication Type]) NOT adult. Articles were required to contain data related to the neuropsychology of emotional dysregulation in children with ADHD. Reviews, case studies, and commentaries were excluded, as were articles that were not specifically related to ADHD and emotional dysregulation (including articles describing studies in individuals in which ADHD was not the primary diagnosis). The search strategy is described in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Fig. 1). The literature search identified 25 original articles (Table 1).
Deficits in emotional control
According to Barkley’s model (Barkley 1997a, b), individuals with ADHD exhibit deficits in inhibition when faced with emotionally charged situations, leading to greater emotional reactivity compared with those without ADHD. In support, children and adolescents (aged 6–15 years) with ADHD were significantly more emotionally reactive than control participants to positive and negative emotionally charged immediate and future challenges (Jensen and Rosen 2004). Similarly, in a study in boys aged 6–12 years challenged with a regulation and control task consisting of a competitive unsolvable Lego puzzle task in which half of the participants were told to hide their feelings, individuals with ADHD were found to have greater behavioral disinhibition and were less able to regulate their emotions, even when prompted to do so, than healthy controls (Walcott and Landau 2004).
Deficit in emotional self-regulation was assessed in a large cohort of 216 children with ADHD and 142 siblings using Conners’ Rating Scale (Parent version) (Anastopoulos et al. 2011). A greater proportion of children with ADHD (46.92 %) displayed high levels of emotional lability than controls (15.38 %). Children with ADHD also showed significantly inferior outcomes in functional impairment and comorbidities, especially aggression and depression, compared with controls. Emotional lability in ADHD was associated with worse outcomes and with multiple-treatment utilization (e.g., use of medication, parent training, and individual therapy). The self-regulation of affect was compared in boys with ADHD and unaffected peers (Braaten and Rosen 2000). Compared with controls, boys with ADHD were found to be less empathic (based on the empathy response task) and had higher scores on the negative emotions subscale (scores for sadness, anger, and guilt) of the Emotional Intensity Scale for Children, although the level of emotional intensity reported by the children did not differ between controls and those with ADHD.
Evidence for a relationship between disturbed emotional self-regulation (the capacity to regulate affect and sustain attention) and the severity of symptoms of ADHD was provided using the Rorschach inkblot method (Meehan et al. 2008). Although without a formal diagnosis of ADHD, children with higher ADHD symptom scores exhibited reduced access to internal resources compared with the comparison group. Furthermore, children with more severe ADHD symptoms generated fewer human movement responses than those with fewer symptoms, suggesting that the former group may have shied away from social exchange. These results appeared to point to a deficit in emotional self-regulation in children with greater symptoms of ADHD. In an investigation of the impact of the subtype of ADHD on emotional self-regulation, children with the combined subtype of ADHD displayed emotional dysregulation (high intensity and high levels of positive and negative behavior) and aggressive behavior, whereas those with the inattentive subtype of ADHD displayed impaired social functioning (social passivity and deficits in social knowledge), but did not exhibit problems with emotional regulation (Maedgen and Carlson 2000). In contrast, a study that evaluated emotional regulation using family interactions during a frustration-inducing task found that poor emotion regulation was not linked to core ADHD symptomatology, but was associated with an aggressive subgroup of boys with ADHD (Melnick and Hinshaw 2000).
Although rating scales are important tools in understanding emotional lability in individuals with ADHD, most are not designed to examine how emotional dysregulation varies over time as children with the disorder attempt to maintain emotional homeostasis during their daily lives. The ecological momentary assessment (EMA) utilizes a handheld device both to prompt parents to enter assessments of their child’s emotional state and to receive them and, therefore, has the potential to assess both discrete and temporal facets of emotional dysregulation. In a small (n = 11), exploratory study in children (aged 8–11 years) with ADHD, parents reported data about their child’s emotional status three times daily (before school, after school, and in the evening) for 28 days (a total of 84 assessments) with outcomes correlated with those of the emotion regulation checklist, the child behavior checklist, and the Children’s Depression Inventory 2nd Edition supporting the validity and utility of the parent-reported EMA (Rosen et al. 2013). Results from a small (n = 5) parallel study did not support the validity of child-reported EMA, perhaps because self-report was problematic in emotionally distressed children (Rosen et al. 2013).
Impairments in executive functioning
Poor executive functioning, which includes the maintenance of future goals, inhibitory control, working memory, and planning, has been linked to the impairment associated with ADHD (Barkley 2001; Willcutt et al. 2005). Accordingly, in 21 boys aged 7–10 years diagnosed with combined or predominantly hyperactive–impulsive subtypes of ADHD and 43 age-matched controls, several measures of executive function, including tests of inhibition, working memory, internalization of speech, self-regulation of emotional arousal, and reconstitution, but not the repetition of the hand movements test relating to working memory, were all found to be independent predictors of ADHD (Berlin et al. 2004).
A possible link between the symptoms and impaired executive function in individuals with ADHD and several socioemotional behaviors, including emotional dysregulation, was investigated in a longitudinal, 2-year study in 87 children (aged 4–6 years) with ADHD and/or impaired executive function (Wahlstedt et al. 2008). Executive function was assessed using measures of inhibition, spatial and verbal working memory, verbal fluency, and intelligence; behavioral assessments included symptoms, emotional regulation, social competence, and internalizing problems. Although both symptoms and impaired executive function were evident for the entire study period, only symptoms at study initiation predicted emotional dysregulation and lower levels of social competence at study end, suggesting that symptoms and impaired executive function are not entirely co-dependent facets of the disorder.
The Behavior Rating Inventory of Executive Function (BRIEF) is a generic instrument used to assess executive function in children and adolescents with ADHD (McCandless and O’Laughlin 2007; Toplak et al. 2009). The BRIEF comprises two indices, Behavioral Regulation and Metacognition, with the former incorporating elements of emotional dysregulation, including inhibition (the ability to resist impulses and stop one’s behavior at the appropriate time), shifting (the ability to make transitions, tolerate change, problem-solve flexibly, and switch one’s attention from one topic to another), and emotional control (the influence of executive functions on the expression and regulation of emotions) (Isquith and Gioia 2008). Sorensen et al. (2011) compared parent-reported BRIEF outcomes in children with ADHD (n = 23), anxiety disorder (n = 24), ADHD with comorbid anxiety disorder (n = 11), and a healthy control group. ADHD was associated with impairments on the inhibit, emotional control, and working memory elements of the BRIEF (Sorensen et al. 2011). Semrud-Clikeman et al. (2010) also used the BRIEF, alongside neuropsychological measures, to evaluate executive function in children with predominantly inattentive ADHD (n = 28), combined-type ADHD (n = 21), Asperger syndrome (n = 15), and controls (n = 32) (Semrud-Clikeman et al. 2010). Overall, this study found that the clinical groups exhibited more difficulty in measures of executive function than controls, although the pattern of impairment across the three clinical groups varied across individual neuropsychological measures and individual BRIEF scales. For example, in the behavioral regulation scales of the BRIEF, scores for children with the combined subtype of ADHD were significantly higher than controls for emotional control, inhibit, and shift, whereas scores for children with the predominantly inattentive subtype of ADHD significantly differed from controls in the inhibit scale only. In contrast, children with combined and predominantly inattentive subtypes of ADHD exhibited significantly greater difficulty than controls in all of the metacognition scales of the BRIEF. Differences in the executive functioning in the clinical groups, including ADHD subtypes, have implications for therapeutic interventions. Furthermore, the observation that the severity of the symptoms of ADHD (or Asperger syndrome) was significantly related to difficulties with behavioral regulation and metacognition suggests that symptom-related behaviors interact with executive processes.
Emotional components of comorbidities
Evidence that emotional dysregulation may be an important component of ADHD, particularly as it presents in adolescence, was provided by a longitudinal study in which individuals diagnosed with ADHD with or without comorbid disruptive behavior disorders during childhood (aged 7–11 years) were followed up 10 years later (Harty et al. 2009). High levels of aggression associated with increased emotionality in the form of anger were reported in adolescents diagnosed with ADHD during childhood, with most of the group differences at follow-up in verbal aggression and anger (but not physical aggression) accounted for by the persistence of ADHD symptoms into adolescence.
A positive correlation between ADHD and both depressive symptoms and emotional dysregulation in a small study of youths aged 10–14 years with (n = 37) or without (n = 32) ADHD led to the hypothesis that emotional dysregulation may link ADHD in childhood with the development of depression in later life (Seymour et al. 2012). Evidence of a link between ADHD symptoms, emotion regulation ability, and depressive symptoms was subsequently confirmed in a larger cohort of 227 youths, of whom 27 met DSM-IV diagnostic criteria for ADHD and were monitored over a 3-year period (Seymour et al. 2014). Structural equation modeling suggested that emotional dysregulation was a significant mechanism underlying the relationship between ADHD and the development of later depression. Although both hyperactive–impulsive symptoms and inattentive symptoms predicted the development of depression, the symptoms of hyperactivity–impulsivity were the more robust predictors of emotional dysregulation. Differences in the pathophysiology of emotional dysregulation in ADHD and other psychiatric disorders were suggested by a functional imaging study in which children with ADHD, unlike those with bipolar disorder or severe mood disorder, displayed hyperactivity of the left amygdala when rating subjective fear of neutral faces suggesting different neural correlates of face-emotion processing in patients with ADHD compared with the other disorders (Brotman et al. 2010).
Neurophysiology and imaging correlates of emotional dysregulation
The amygdala is implicated in the regulation of emotion and the relationship between intrinsic functional connectivity (iFC) of amygdala circuits, and emotion regulation deficit in children aged 6–13 years with ADHD (n = 63) and healthy controls (n = 19) was evaluated using functional magnetic resonance imaging (fMRI) (Hulvershorn et al. 2014). Within the ADHD group, higher levels of emotional lability, determined using the Emotional Lability subscale of the Conners’ Parent Rating Scale–Revised, long version, were associated with greater positive iFC between the amygdala and the anterior cingulate cortex, and with negative iFC between the amygdala and the posterior insula/superior temporal gyrus. Differences between the ADHD subgroup with low levels of emotional lability and healthy controls were small and nonsignificant, suggesting that the abnormal functional connectivity was specific to emotional lability rather than to other ADHD symptoms.
Effortful control, or the self-regulation aspects of temperament, was investigated in children with ADHD (n = 10) and typically developing controls (n = 16) using a combination of psychosocial (the Effortful Control Scale and the Attentional Control Scale) and physiological [electroencephalographic event-related potentials (ERPs)] measures during the administration of the Go/No-Go task (Wiersema and Roeyers 2009). ADHD symptoms were associated with low scores on the rating scales, errors of commission in the Go/No-Go task, and small No-Go P3 amplitudes, suggesting that effortful control is implicated in ADHD. ERP evidence of atypical emotional processing was also observed during a facial emotional processing task in adolescent boys with ADHD (n = 31) compared with controls without ADHD (n = 32) (Gow et al. 2013). Negative facial expressions were associated with an exaggerated P2 wave in those with ADHD; N2 and N4 waves were also atypical in this group. Furthermore, ERP abnormalities in emotional processing were significantly associated with lower plasma omega-3 fatty acids levels in the ADHD group, suggesting that lower plasma long-chain polyunsaturated fatty acids are associated with impaired emotional processing in ADHD.
Autonomic correlates of emotional dysregulation
Respiratory sinus arrhythmia (RSA) is the natural variation in heart rate that occurs during breathing, whereby heart rate increases during inhalation and decreases during exhalation and is an indirect biomarker of vagal tone. RSA is particularly pronounced in children, and abnormal RSA has been linked to emotional dysregulation in childhood psychopathologies (Beauchaine et al. 2013). In a study of children with ADHD (n = 32) and typically developing controls (n = 34), physiological recordings were conducted during a task that required participants to view an emotion-laden film while mimicking (induction) or masking (suppression) the emotion of the main character (Musser et al. 2011). Healthy controls exhibited systematic variation in RSA, which depended on emotional valence (more activation for negative emotion, reduced activation for positive emotion) and task demand (more activation for suppression than induction), whereas children with ADHD displayed a stable pattern of elevated parasympathetic activity across all task conditions compared to baseline. No group differences in cardiac pre-ejection period (PEP, an indicator of sympathetic activity) were observed. Added complexity was provided by a subsequent study using similar methodology in which participants were classified into three groups: children with ADHD and low prosocial behavior such as callousness or unemotional traits (n = 21), those with ADHD with developmentally appropriate prosocial behavior (n = 54), and typically developing children (n = 75) (Musser et al. 2013). In the ADHD group with developmentally appropriate prosocial behavior, positive induction was associated with atypically elevated parasympathetic (RSA) reactivity during positive induction, along with increased sympathetic (PEP) activity across conditions. In contrast, children with ADHD and low prosocial behavior displayed both reduced parasympathetic reactivity and reduced sympathetic activity across baseline and task conditions. Thus, both ADHD groups exhibited altered patterns of autonomic functioning, but in two distinct forms.
The possible utility of this form of physiological testing in identifying children at risk of emotional dysregulation was investigated in a cohort of 99 young children (aged 4–6 years) with ADHD during three conditions (baseline, reward task, and block building) (Beauchaine et al. 2013). Children with low RSA at baseline and greater RSA withdrawal during block building exhibited poorer regulation of emotion and scored lower for prosocial behavior than their peers. Furthermore, lengthened cardiac PEP at rest and reduced PEP reactivity to incentives were associated with increased levels of conduct problems and aggression.
Multiple pathway models of ADHD
The heterogeneity of ADHD is reflected in the proposal of various multiple pathway models for the disorder. One example proposes that executive deficits lead to symptoms of inattention and that reward–response deficits lead to hyperactivity (Sonuga-Barke 2002, 2005). A second example proposes that effortful control is associated with the core symptoms of ADHD, negative emotionality with comorbid antisocial or disruptive behavior (Nigg et al. 2004). This suggests that the neuropsychological deficits that underpin the symptoms of ADHD may be different from those leading to disruptive behavior problems was investigated by examining the personality–temperament traits of reactive and effortful control, resiliency, and emotionality in 179 children aged 6–12 years with ADHD (n = 92), without ADHD (n = 52), or with borderline or not otherwise specified ADHD (n = 35) (Martel and Nigg 2006). The results support a model in which regulation problems contribute to the emergence of symptoms of inattention–disorganization and reactive or motivational control problems contribute to the emergence of hyperactivity–impulsivity symptoms, whereas negative affect was associated with oppositional defiance. Thus, children exhibiting regulation deficits and reactive motivational behaviors may be at particular risk of the development of ADHD.
The contribution of deficits in different neuropsychological domains to ADHD was examined in children (aged 7–12 years) with ADHD (n = 102) and controls (individually matched for age and sex) using assessments of executive function (working memory, inhibition, and shifting), delay aversion, reaction time variability, and emotion regulation and recognition (Sjowall et al. 2013). Children with ADHD differed significantly from controls on all measures, except for delay aversion and recognition of disgust. Executive functioning, reaction time variability, and emotional functioning all contributed independently to distinguishing between children with ADHD and controls. This study, therefore, supports the concept of ADHD as a heterogeneous disorder and highlights the importance of emotional functioning to conceptual models of the disorder.
Physiological evidence for a dissociation between attentional and affective neural pathways in individuals with ADHD was generated using resting-state functional connectivity MRI in medication-naïve children with (n = 22) or without (n = 20) ADHD. Neural connectivity in neural circuits underlying executive function and emotional regulation was found to be reduced in participants with the disorder compared with controls (Posner et al. 2013). Interestingly, reduced connectivity in the executive attention circuit was related to executive attention deficits, but not to emotional lability, whereas reduced connectivity in the emotional regulation circuit related to emotional lability but not to executive attention deficits. Thus, these imaging data add further weight to the suggestion that multiple pathways underpin the pathophysiology of ADHD.
Conclusions
Understanding of emotional dysregulation in children with ADHD is not complete, and there is currently no single definition for the phenomenon. Neuropsychological tests of emotional control (impulsivity, self-regulation of positive and negative emotions, and executive function) indicate that the processing of emotional stimuli is impaired in ADHD. Most descriptions of emotional dysregulation in ADHD include the concepts of an inability to modulate emotional responses and excessive reactions to a particular emotional trigger that would be considered inappropriate for the developmental age of the individual and the social setting. Inappropriate responses may be both internalized (e.g., the individual may be withdrawn, moody, or sad) or externalized (e.g., they may be emotionally volatile, aggressive, argumentative, and even physical). Furthermore, evidence continues to emerge that deficits in more than one neurological pathway are responsible for emotional dysregulation in ADHD.
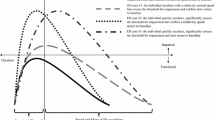
Figure 2, adapted from Gross (1998), presents a possible conceptual model which attempts to visualize how extrinsic or intrinsic stimuli may lead to emotional dysregulation, resulting in internalizing or externalizing symptoms in children with ADHD. Early-life emotion regulation is managed largely by extrinsic situation selection (e.g., parents organizing their child’s daily routine), but as children grow older, they develop their own regulatory processes. Situation modification is an attempt, either extrinsically or intrinsically, to alter the subsequent course of the emotional response. Attention deployment is where the individual selects the aspect of the situation to focus on in order to help control the emotional response. Cognitive change is where the individual changes their perception of the situation (intrinsic), or they alter someone else’s perception, or have their own perception changed by someone else (extrinsic). Response modulation refers to the attempts to directly influence the response tendencies through the action of drugs, food, exercise and relaxation, etc. or by the modulation of emotion-expressive behavior. This process may not be learned at age appropriate times, and individuals with ADHD may have poor attention deployment and impulse control, thereby leading to premature exit from the cognitive process and resulting in emotional dysregulation.
Conceptual model for emotional dysregulation in children with ADHD. ADHD attention-deficit/hyperactivity disorder. Developed and adapted from Gross (1998)
Although caregivers and patients with ADHD constantly search for explanations for emotional lability such as that described in the two case examples at the beginning of this article, there is currently no gold standard for assessing emotional dysregulation in ADHD. In many cases, individuals with ADHD and significant impairment from emotional dysregulation do not meet DSM-5 criteria for a distinct co-morbid diagnosis. Having clinically useful measures of emotional dysregulation, and furnishing clinicians with a robust definition, could help caregivers and patients to improve their understanding of the condition. Defining and measuring emotional dysregulation on a clinical level should be a priority. Novel or new applications of neuropsychological instruments, neurophysiological and imaging techniques, and biomarkers of emotional dysregulation in children with ADHD are emerging, and however, more research is needed to develop reliable and universally accepted measures in affected children and to determine which deficits are particularly problematic at a functional level in terms of their daily life and social, emotional, and cognitive development
Once such measures are developed, they could be used to test the efficacy of potential treatments in emotional dysregulation. Clinically, parents report that there is improvement in emotional regulation when ADHD is treated pharmacologically, perhaps through improvements in the areas of impulse control and attentional deployment. ADHD pharmacotherapy does not, however, address the delayed development of cognitive control skills in individuals with ADHD. Hence, in addition to pharmacotherapy, treatment should focus on the learning of cognitive skills throughout the developmental process.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). American Psychiatric Publications
Anastopoulos AD, Smith TF, Garrett ME, Morrissey-Kane E, Schatz NK, Sommer JL, Kollins SH, Ashley-Koch A (2011) Self-regulation of emotion, functional impairment, and comorbidity among children with AD/HD. J Atten Disord 15:583–592
Barkley RA (1997a) Attention-deficit/hyperactivity disorder, self-regulation, and time: toward a more comprehensive theory. J Dev Behav Pediatr 18:271–279
Barkley RA (1997b) Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 121:65–94
Barkley RA (2001) The executive functions and self-regulation: an evolutionary neuropsychological perspective. Neuropsychol Rev 11:1–29
Barkley RA (2010) Deficient emotional self-regulation: a core component of attention-deficit/hyperactivity disorder. J ADHD Relat Disord 1:5–37
Beauchaine TP, Gatzke-Kopp L, Neuhaus E, Chipman J, Reid MJ, Webster-Stratton C (2013) Sympathetic- and parasympathetic-linked cardiac function and prediction of externalizing behavior, emotion regulation, and prosocial behavior among preschoolers treated for ADHD. J Consult Clin Psychol 81:481–493
Berlin L, Bohlin G, Nyberg L, Janols L-O (2004) How well do measures of inhibition and other executive functions discriminate between children with ADHD and controls? Child Neuropsychol 10:1–13
Braaten EB, Rosen LA (2000) Self-regulation of affect in attention deficit-hyperactivity disorder (ADHD) and non-ADHD boys: differences in empathic responding. J Consult Clin Psychol 68:313
Brotman MA, Rich BA, Guyer AE, Lunsford JR, Horsey SE, Reising MM, Thomas LA, Fromm SJ, Towbin K, Pine DS, Leibenluft E (2010) Amygdala activation during emotion processing of neutral faces in children with severe mood dysregulation versus ADHD or bipolar disorder. Am J Psychiatry 167:61–69
Gordon M (1995) How to operate an ADHD clinic or subspeciality practice. DeWitt, New York
Gow RV, Sumich A, Vallee-Tourangeau F, Crawford MA, Ghebremeskel K, Bueno AA, Hibbeln JR, Taylor E, Wilson DA, Rubia K (2013) Omega-3 fatty acids are related to abnormal emotion processing in adolescent boys with attention deficit hyperactivity disorder. Prostaglandins Leukot Essent Fatty Acids 88:419–429
Gross JJ (1998) The emerging field of emotion regulation: an integrative review. Rev Gen Psychol 2:271–299
Harty SC, Miller CJ, Newcorn JH, Halperin JM (2009) Adolescents with childhood ADHD and comorbid disruptive behavior disorders: aggression, anger, and hostility. Child Psychiatry Hum Dev 40:85–97
Hulvershorn LA, Mennes M, Castellanos FX, Di Martino A, Milham MP, Hummer TA, Roy AK (2014) Abnormal amygdala functional connectivity associated with emotional lability in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 53(351–361):e351
Isquith PK, Gioia GA (2008) Behavior Rating Inventory of Executive Function® Feedback Report. http://www.psychassessments.com.au/products/280/prod280_report1.pdf Accessed: 22 Sept 2015
Jensen SA, Rosen LA (2004) Emotional reactivity in children with attention-deficit/hyperactivity disorder. J Atten Disord 8:53–61
Karalunas SL, Fair D, Musser ED, Aykes K, Iyer SP, Nigg JT (2014) Subtyping attention-deficit/hyperactivity disorder using temperament dimensions: toward biologically based nosologic criteria. JAMA Psychiatry 71:1015–1024
Laufer M, Denhoff E, Solomons G (1957) Hyperkinetic impulse disorder in children’s behavior problems. Psychosom Med 19:38–49
Maedgen JW, Carlson CL (2000) Social functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. J Clin Child Psychol 29:30–42
Martel MM, Nigg JT (2006) Child ADHD and personality/temperament traits of reactive and effortful control, resiliency, and emotionality. J Child Psychol Psychiatry 47:1175–1183
McCandless S, O’Laughlin L (2007) The Clinical Utility of the Behavior Rating Inventory of Executive Function (BRIEF) in the diagnosis of ADHD. J Atten Disord 10:381–389
Meehan KB, Ueng-McHale JY, Reynoso JS, Harris BH, Wolfson VM, Gomes H, Tuber SB (2008) Self-regulation and internal resources in school-aged children with ADHD symptomatology: an investigation using the Rorschach inkblot method. Bull Menn Clin 72:259–282
Melnick SM, Hinshaw SP (2000) Emotion regulation and parenting in AD/HD and comparison boys: linkages with social behaviors and peer preference. J Abnorm Child Psychol 28:73–86
Musser ED, Backs RW, Schmitt CF, Ablow JC, Measelle JR, Nigg JT (2011) Emotion regulation via the autonomic nervous system in children with attention-deficit/hyperactivity disorder (ADHD). J Abnorm Child Psychol 39:841–852
Musser ED, Galloway-Long HS, Frick PJ, Nigg JT (2013) Emotion regulation and heterogeneity in attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 52:163–171
Nigg JT, Goldsmith HH, Sachek J (2004) Temperament and attention deficit hyperactivity disorder: the development of a multiple pathway model. J Clin Child Adolesc Psychol 33:42–53
Posner J, Rauh V, Gruber A, Gat I, Wang Z, Peterson BS (2013) Dissociable attentional and affective circuits in medication-naive children with attention-deficit/hyperactivity disorder. Psychiatry Res 213:24–30
Rhodes SM, Coghill DR, Matthews K (2005) Neuropsychological functioning in stimulant-naive boys with hyperkinetic disorder. Psychol Med 35:1109–1120
Ricard M, Kamberk-Kilicci M (1995) Children's empathic responses to emotional complexity. Int J Behav Dev 18:211–225
Rosen PJ, Epstein JN, Van Orden G (2013) I know it when I quantify it: ecological momentary assessment and recurrence quantification analysis of emotion dysregulation in children with ADHD. Atten Defic Hyperact Disord 5:283–294
Rydell AM, Berlin L, Bohlin G (2003) Emotionality, emotion regulation, and adaptation among 5- to 8-year-old children. Emot 3:30–47
Semrud-Clikeman M, Walkowiak J, Wilkinson A, Butcher B (2010) Executive functioning in children with Asperger syndrome, ADHD-combined type, ADHD-predominately inattentive type, and controls. J Autism Dev Disord 40:1017–1027
Seymour KE, Chronis-Tuscano A, Halldorsdottir T, Stupica B, Owens K, Sacks T (2012) Emotion regulation mediates the relationship between ADHD and depressive symptoms in youth. J Abnorm Child Psychol 40:595–606
Seymour KE, Chronis-Tuscano A, Iwamoto DK, Kurdziel G, Macpherson L (2014) Emotion regulation mediates the association between ADHD and depressive symptoms in a community sample of youth. J Abnorm Child Psychol 42:611–621
Shaw P, Stringaris A, Nigg J, Leibenluft E (2014) Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry 171:276–293
Sjowall D, Roth L, Lindqvist S, Thorell LB (2013) Multiple deficits in ADHD: executive dysfunction, delay aversion, reaction time variability, and emotional deficits. J Child Psychol Psychiatry 54:619–627
Sonuga-Barke EJS (2002) Psychological heterogeneity in AD/HD—a dual pathway model of behaviour and cognition. Behav Brain Res 130:29–36
Sonuga-Barke EJ (2005) Causal models of attention-deficit/hyperactivity disorder: from common simple deficits to multiple developmental pathways. Biol Psychiatry 57:1231–1238
Sorensen L, Plessen KJ, Nicholas J, Lundervold AJ (2011) Is behavioral regulation in children with ADHD aggravated by comorbid anxiety disorder? J Atten Disord 15:56–66
Stringaris A (2011) Irritability in children and adolescents: a challenge for DSM-5. Eur Child Adolesc Psychiatry 20:61–66
Stringaris A, Goodman R (2009) Three dimensions of oppositionality in youth. J Child Psychol Psychiatry 50:216–223
Toplak ME, Bucciarelli SM, Jain U, Tannock R (2009) Executive functions: performance-based measures and the behavior rating inventory of executive function (BRIEF) in adolescents with attention deficit/hyperactivity disorder (ADHD). Child Neuropsychol 15:53–72
Wahlstedt C, Thorell LB, Bohlin G (2008) ADHD symptoms and executive function impairment: early predictors of later behavioral problems. Dev Neuropsychol 33:160–178
Walcott CM, Landau S (2004) The relation between disinhibition and emotion regulation in boys with attention deficit hyperactivity disorder. J Clin Child Adolesc Psychol 33:772–782
Ward MF, Wender PH, Reimherr FW (1993) The Wender Utah Rating Scale: an aid in the retrospective. Am J Psychiatry 150:885–890
Wiersema JR, Roeyers H (2009) ERP correlates of effortful control in children with varying levels of ADHD symptoms. J Abnorm Child Psychol 37:327–336
Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF (2005) Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry 57:1336–1346
Acknowledgments
Shire International GmbH provided funding to Oxford PharmaGenesis for support in writing and editing this manuscript. Under the direction of the author, Dr Eric Southam and Dr. Jim Purvis, employees of Oxford PharmaGenesis, provided writing assistance for this publication. Editorial assistance in formatting, proofreading, copyediting, and fact-checking was also provided by Oxford PharmaGenesis. Although Shire Development LLC and Shire International GmbH were involved in the topic concept and fact checking of information, the content of this manuscript, the interpretation, and the decision to submit the manuscript for publication in ADHD Attention-Deficit/Hyperactivity Disorder was made by the author independently.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JvS has received compensation for serving as a consultant or speaker for Bristol-Myers Squibb, Janssen-Cilag, Purdue and Shire and has received research grants from Janssen-Cilag, Purdue and Shire.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
van Stralen, J. Emotional dysregulation in children with attention-deficit/hyperactivity disorder. ADHD Atten Def Hyp Disord 8, 175–187 (2016). https://doi.org/10.1007/s12402-016-0199-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-016-0199-0