Abstract
Purpose
Dry eye disease (DED) is a highly prevalent ocular condition with a significant burden on affected patients. Regardless of the underlying etiology, DED is associated with increased ocular surface inflammation. We investigated the safety and efficacy of a short-term treatment with topical low dose hydrocortisone in patients with chronic DED and ocular surface inflammation.
Methods
A total of 60 patients (mean age 51 ± 14 years) with chronic DED and conjunctival hyperemia greater than grade 2 on the Efron scale were included. Patients were randomized to receive either preservative-free hydrocortisone 0.335% (Softacort, Laboratories Thea, France) for 12 days four times daily followed by 2 days twice daily instillation (intense treatment group) or 8 days three times daily followed by 3 days twice daily treatment (standard treatment group). Ocular redness was assessed at baseline, day 14, and day 28. Measurement of intraocular pressure (IOP) and clinical tests to assess signs and symptoms of DED were performed.
Results
Conjunctival hyperemia and Ocular Surface Disease Index (OSDI) significantly decreased in both treatment groups (p < 0.001 each) after hydrocortisone treatment. A significant increase in tear film thickness was seen 4 weeks after treatment start (p = 0.03 and p = 0.04, respectively). IOP did not change in either of the two treatment groups (p = 0.45).
Conclusion
Treatment with low dose hydrocortisone 0.335% reduced ocular inflammation and decreased OSDI score. No change in IOP was observed in either of the two treatment schedules. Because of its good safety profile, low dose hydrocortisone may be an interesting alternative to standard corticosteroid treatment in DED.
Funding
Laboratories Thea.
Trial Registration
Clinicaltrials.gov registry: NCT03907865.
Similar content being viewed by others
Why carry out this study? |
Dry eye disease (DED) is a common ocular condition of the ocular surface and the tear film. |
The prevalence of DED is high with 5–30% being affected. |
Anti-inflammatory agents are warranted for patients not sufficiently treated with topical lubricants alone. |
This study set out to investigate the safety and efficacy of two different treatment regimens (standard and intense) of a recently introduced low dose preservative-free formulation of hydrocortisone 0.335%. |
What was learned from the study? |
Ocular redness and DED symptoms significantly decreased in both treatment groups after hydrocortisone treatment accompanied by a significant increase in tear film thickness. |
Because of its good safety profile, low dose hydrocortisone may be an interesting alternative to standard corticosteroid treatment in DED. |
Introduction
Dry eye disease (DED) is a common ocular condition of the ocular surface and the tear film caused by tear deficiency or excessive evaporation, leading to damage to the interpalpebral ocular surface [1]. The prevalence of DED is high, especially in the elderly. Data from epidemiological studies report a prevalence for DED between 5% and 30%, depending on the method of evaluation and the definition of the disease [2]. From a pathophysiological point of view, ocular surface inflammation, hyperosmolarity, and tear film instability have been identified as the main triggers for the development and progression of the disease [3, 4].
Currently, topical lubricants are the mainstay for therapy in particular for mild and moderate forms of DED [5]. However, since topical lubricants have no pharmacologically active ingredient, their effect on pathogenetic factors such as ocular surface inflammation is limited and only secondary to their moistening effects. Thus, in particular for patients with chronic DED, where the inflammatory component is predominant in their clinical manifestation, concomitant pulse therapy with potent anti-inflammatory agents may be useful. This is also reflected in the guidelines of the Dry Eye Workshop II (DEWS II) report recommending pharmacological treatment with anti-inflammatory agents in cases where topical lubricants alone are not sufficient [6].
Although anti-inflammatory agents such as cyclosporine or lifitegrast have been shown to be effective for the treatment of DED with severe keratitis, topical preservative-free (PF) corticosteroids still remain an interesting therapy option. The major advantages of corticosteroid treatment including their well-known anti-inflammatory potential and the fast onset of the therapeutic effect have to outweigh their potential side effects most importantly the increase of intraocular pressure (IOP) and cataract formation [7]. New formulations of low dosage topical PF soft steroids with limited penetration in the cornea may overcome these limitations and have evoked interest in corticosteroid treatment for DED.
Thus, the current study set out to investigate the safety and efficacy of two different treatment regimens of a recently introduced low dose formulation of hydrocortisone 0.335% (Softacort®, Laboratories Thea, France). Although its active agent hydrocortisone has been known for a long time, the low solubility and the low penetration through the ocular surface have limited its use for the treatment of intraocular inflammatory conditions. However, as for the treatment of DED the site of action of the drug is not within the eye but on the ocular surface, the low penetration of the drug is a key advantage because it may limit the unwanted ocular side effects caused by high corticosteroid concentration in the anterior chamber such as increase of IOP and cataract formation.
Methods
Patients
Sixty patients with chronic DED were included in this study. The study protocol was approved by the Ethics Committee of the Medical University of Vienna. The study was performed in adherence to the guidelines of the Declaration of Helsinki including all revisions as well as Good Clinical Practice guidelines. Written informed consent was obtained from all study participants prior to participation and Springer’s policy concerning informed consent has been followed.
All patients included in the study passed a screening examination 14 days prior to study start. Screening included medical history, a pregnancy test in women of childbearing potential, followed by subjective assessment of symptoms of DED using the Ocular Surface Disease Index (OSDI). In addition, an ophthalmic examination was performed, including best corrected visual acuity (BCVA), slit lamp biomicroscopy with indirect funduscopy, measurement of tear film break-up time (TFBUT), corneal fluorescein staining, and measurement of IOP. Redness of the eye was assessed by slit lamp biomicroscopy and graded as described in detail later.
Only patients who were diagnosed by a trained ophthalmologist as having DED and who were already under topical lubricant treatment for at least 3 months were included. The exact inclusion parameters for the study were as follows: age of at least 18 years, normal ophthalmic findings except history of DED for at least 3 months, and current therapy with topical lubricants for at least 3 months. Further inclusion criteria were OSDI score of at least 22 points and conjunctival hyperemia of at least grade 3 on the Efron scale.
The study eye was defined as the eye with the higher score on the Efron scale at visit 1. If the score was identical for both eyes, the eye with the higher corneal fluorescein staining score was chosen. If also those results were identical for both eyes, the right eye was used for analysis.
Patients were excluded if they fulfilled at least one of the following criteria: clinically significant slit lamp findings at screening visit except DED, participation in a clinical trial in the 4 weeks preceding the screening visit, and symptoms of a clinically relevant illness in the 3 weeks before the screening visit. Further, patients with presence or history of a severe medical or surgical condition as judged by the clinical investigator, with intake of parasympathomimetic or antipsychotic drugs, wearing of contact lenses, glaucoma in the medical history, history of IOP increase caused by systemic or topical treatment with corticosteroids, IOP greater than 22 mmHg, treatment with corticosteroids in the 4 weeks preceding the study, or topical treatment with any ophthalmic drug except topical lubricants in the 4 weeks preceding the study were excluded. Further exclusion criteria were ocular infection or clinically significant inflammation, ocular surgery in the 3 months preceding the study, Sjögren’s syndrome, Stevens-Johnson syndrome, history of allergic conjunctivitis, pregnancy, planned pregnancy or lactating, or known hypersensitivity to any component of study medication.
Eye Drops
On the first study day, patients were randomized to receive hydrocortisone 0.335% eye drops (Softacort, Laboratories Thea, Clermont-Ferrand, France) in two different application schemes: Group 1 was treated for 12 days four times a day followed by 2 days two times a day (14 days in total, intense treatment group). Group 2 received treatment for 8 days three times a day and 3 days two times a day resulting in a total treatment period of 11 days (standard treatment group). Patients in both groups were asked to continue and document the use of their own topical lubricants in a diary.
Description of Study Days
For included patients four study visits were scheduled. On the first visit (visit 1) a pregnancy test was performed in women with childbearing potential, followed by the assessment of symptoms using the OSDI test and a dry eye visual analogue scale (VAS). Then, measurements of tear film thickness (TFT) using the ultra-high resolution spectral domain optical coherence tomography (UHR-OCT) system were performed. After the assessment of TFT, slit lamp biomicroscopy including grading of conjunctival hyperemia was done, followed by measurements of tear osmolarity, TFBUT, corneal fluorescein staining, impression cytology for human leukocyte antigen-DR (HLA-DR) assessment, and measurement of IOP. On visit 2, 7 days after the first visit, patients returned to the department for IOP measurement only. At day 14 (visit 3) and day 28 (visit 4) all examinations were repeated as described for visit 1. All examinations were scheduled at the same time of the day and were performed in exactly the same order as described for visit 1.
Measurement Techniques
Assessment of Conjunctival Hyperemia
Conjunctival hyperemia was assessed by the investigator during slit lamp examination according to the 5-grade hyperemia scale introduced by Efron [8] as follows: 0 = none, 1 = trace, 2 = mild, 3 = moderate, 4 = severe hyperemia.
Intraocular Pressure
IOP was measured using a Goldmann applanation tonometer after topical anesthesia with oxybuprocaine hydrochloride combined with sodium fluorescein.
Ocular Surface Disease Index
For the assessment of symptoms, the well-described OSDI was used [9]. This questionnaire is specifically designed for patients with DED and asks patients about the frequency of specific symptoms and their impact on vision-related tasks of daily life.
Dry Eye Visual Analogue Scales
Subjects were asked to rate their ocular symptoms (both eyes simultaneously) by placing a vertical mark on a horizontal line to indicate the level of discomfort (0 corresponding to “no symptoms” and 100 corresponding to “maximal symptoms”). The assessment line length of the scale was 100 mm. Patients were asked to rate the following questions: “I feel satisfied using this treatment”, “With these eye drops, I have a feeling of freshness”, “With these eye drops, I have a feeling of relief”, “This product contributed to reduce my pain due to eye dryness”, “This product is comfortable”.
Best Corrected Visual Acuity
BCVA was measured using the standard Early Treatment Diabetic Retinopathy Study (ETDRS) acuity chart and reported in ETDRS letters.
Tear Film Break-Up Time
TFBUT was assessed following the guidelines published in the report of the DEWS 2007 using Minims fluorescein sodium 2.0% eye drops [10]. Measurements were repeated three times and the mean value was used.
Corneal Fluorescein Staining
Minims fluorescein sodium 2.0% eye drops were used to detect corneal epithelial defects. Corneal staining was graded according to the Oxford scale [11].
Tear Film Thickness as Measured with Optical Coherence Tomography
To assess precorneal TFT a previously developed UHR-OCT system for imaging of the anterior segment was used. The technique and data regarding the reproducibility have been published in detail previously [12]. In principle the UHR-OCT is based on a broadband Ti:sapphire laser operating at 800 nm with spectral bandwidth 170 nm allowing for an axial resolution in tissue of about 1.2 µm. For measurement of TFT, 3-dimensional data sets centered on the apex of the cornea and with a size of 4 mm × 4 mm × 1 mm (horizontal × vertical × depth), each containing 512 × 128 × 1024 pixels were acquired. Central TFT was assessed using the tomograms around the central reflex of the probe at the corneal apex.
To obtain reliable measurements, the subjects followed the same measurement procedures: subjects were asked to look onto an internal fixation target and blink normally. Data acquisition started immediately after reopening of the eye and patients were asked to keep the eye open until the end of the measurement. A total of three volumes were acquired during the measurement period of 3 s. TFT was then calculated on the basis of the second and third recorded volume.
Impression Cytology for HLA-DR Assessment
Two samples were taken from the upper conjunctiva of the study eye using EYEPRIM™ (Opia Technologies S.A.S., Paris, France). The subject was instructed to look down and the device was positioned upon the conjunctiva. Then, the push-button was pressed until the stop position was reached and the device was held in this position for 2–3 s. Afterwards, the pressure was released and the device was removed from the eye. The sampling membrane was ejected in a storage container by pressing the push-button once again. The samples were stored according to the manufacturer’s instructions and were sent under observer-blinded conditions to an independent laboratory (Eyenostics, La Gaude, France) for analysis and assessment of HLA-DR levels.
Tear Film Osmolarity
Tear film osmolarity was measured using a non-invasive, commercially available instrument (TearLab®, OcuSens Inc, San Diego, USA) at the indicated time points. Reproducibility of the instrument has been published previously [13, 14].
Sample Size Considerations and Statistical Analysis
As the effect of hydrocortisone on the inflammatory component of DED was of particular interest, the primary outcome of the study was defined as change in conjunctival hyperemia at visit 3 (2 weeks after treatment start). A total of 60 patients entered the study. This sample size was calculated on the basis of a power of 95% and a two-sided alpha-level of 0.05. A clinically relevant change in conjunctival hyperemia grading was considered 20% or more compared to baseline. The sample size calculation was based on the assumption that the standard deviation of the main outcome variable is 15% or less as published previously [8].
Additional outcome variables were OSDI, TFBUT, corneal staining, TFT, percentage of HLA-DR-positive cells, and frequency of artificial tear instillation. IOP was measured at three time points after treatment start as safety variable. Statistical analysis was carried out as a “per protocol” analysis. To detect differences between treatments, a repeated-measures analysis of variance (ANOVA) model was applied for analysis of all outcome parameters. Planned comparisons within the ANOVA model were performed to assess contrasts between time points and treatment groups. A p ≤ 0.05 was considered significant. All statistical analyses were carried out using CSS Statistica (version 6.0; Tulsa, OK, USA). All data are presented as mean ± SD.
Results
Demographics
A total of 60 patients were included (mean age 51 ± 14 years) and finished the study according to the protocol. Of those participants, 20 patients were male and 40 patients were female. The mean duration of DED in the study population was 8.2 ± 8.7 years. All included patients completed the screening visit and the first study day within 2 weeks.
Outcome Variables
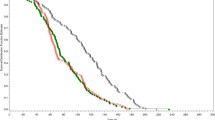
As shown in Fig. 1, conjunctival hyperemia as assessed using the Efron scale significantly decreased in the study eye by − 25.0 ± 24.2% in the intense treatment group and by − 18.6 ± 18.8% in the standard treatment group, at the end of the treatment period (visit 3). At visit 4, this effect was still present (− 23.9 ± 21.2% in the intense treatment group and − 27.5 ± 23.3% in the standard treatment group, p < 0.001 each vs. baseline). No statistically significant difference in the change in Efron scale was observed between the two treatment groups (p = 0.26, intense and standard treatments).
OSDI decreased during the study period in both study groups (intense treatment group: − 10.8 ± 37.8%, p = 0.08 vs. baseline; standard treatment group: − 41.3 ± 28.2%, p < 0.001 vs. baseline) 14 days after treatment start. A significant decrease was seen 4 weeks after treatment start in both groups (− 19.5 ± 39.1% and − 24.1 ± 33.9%, p < 0.01 vs. baseline each, Fig. 2).
TFT tended to increase from baseline to visit 3, but this effect did not reach the level of significance (+ 2.0 ± 8.6% in the intense treatment group, p = 0.24 and + 3.8 ± 9.5% in the standard treatment group, p = 0.11, Fig. 3). At visit 4, however, a significant increase in TFT was observed in both groups (5.3 ± 8.9%, p = 0.03 vs. baseline and 5.6 ± 13.1%, p = 0.04 vs. baseline, respectively). No difference in the TFT changes was observed between the two dose groups (p = 0.94).
As shown in Table 1, a significant decrease in corneal fluorescein staining was observed in the intense treatment group at visit 4 only. No change in tear osmolarity, TFBUT, or percentage of HLA-DR-positive cells was observed in either of the two dosage groups (Table 1).
Frequency of artificial tear instillation was 3.0 ± 2.4 drops/day at baseline in the intense treatment group and significantly decreased to 1.2 ± 2.3 drops/day at visit 3 (p < 0.001 vs. baseline) and to 2.5 ± 2.2 drops/day at visit 4 (p = 0.04 vs. baseline). In the standard treatment group, frequency of artificial tear instillation decreased from 3.4 ± 3.1 drops/day at baseline to 0.9 ± 1.2 at visit 3 and 2.4 ± 3.1 drops/day at visit 4 (p < 0.001 vs. baseline each). No difference was observed between the two groups (p = 0.42).
Assessment of subjective parameters revealed that patients were satisfied with the treatment in both groups with no differences between groups (Table 2).
Safety Evaluation
As illustrated in Fig. 4, IOP did not change at the end of the treatment period in either the intense dose (baseline, 14.1 ± 1.8; day 14, 13.9 ± 2.0 mmHg) or in the standard dose group (baseline, 12.8 ± 1.9; day 14, 13.3 ± 2.1 mmHg). No difference between the two groups was observed (p = 0.45).
No serious adverse events (AEs) were observed during the study. Most AEs were mild and none was severe. No AE was judged as “definitely” or “probably” related to the study drug. Most frequent eye-related AEs that were judged as “possibly” or “unlikely” related to the study drug were burning sensation in the eyes (n = 4), burning sensation (n = 3), and blurred vision (n = 2).
Discussion
The results of the current study show that the new formulation of low dose PF hydrocortisone 0.335% improves the signs and symptoms in patients with DED. This was observed using an intense as well as the standard treatment schedule with no difference between these two groups. In addition, the safety analysis shows that the formulation is safe and does not affect IOP. The safety profile with respect to potential effects on IOP is of critical importance when using corticosteroids as an anti-inflammatory therapy for DED. Finally, our study shows that treatment with a topic anti-inflammatory drug increases TFT and re-establishes a normal tear film in patients with DED while also reducing the concomitant use of artificial tears.
Both preclinical and clinical trials show that topical corticosteroids are effective in treating the inflammation associated with DED. According to the current pathophysiological concept of DED this allows one to break the vicious circle that includes tear film hyperosmolarity and instability [3]. On a cellular basis, corticosteroids exert their biological effects on several different molecular mechanisms including the lipocortin-1-induced suppression of phospholipase A2, thereby reducing eicosanoid production and the inhibition of various leukocyte-related inflammatory events [15]. Reducing both inflammatory mediators and cellular immune response explains their fast onset of action and their strong anti-inflammatory effect at the ocular surface.
The data of the current study shows that the new low dose PF formulation of hydrocortisone 0.335% reduces signs and symptoms of DED in both an intense treatment scheme and a 12-day standard treatment. In particular, our data indicate that treatment with hydrocortisone for 12 days four times daily or 8 days three times daily followed by a short taper off phase significantly reduces ocular redness as measured using the Efron scale. Furthermore, this reduction is accompanied by the decrease of OSDI up to − 25%, indicating also pronounced amelioration of subjective symptoms for DED as well as an increase in TFT.
The current study is the first to show in a longitudinal design that a hydrocortisone treatment for 2 weeks significantly increases TFT thickness over time. Although the observed change in TFT is small, the strength of the OCT-based measurement of TFT is that with a coefficient of variation of less than 4% the instrument is capable of detecting subtle changes in TFT in patients with DED [12]. As such, we have reported in previous experiments using the same UHR-OCT system that treatment with topical lubricants leads to a short-time increase in TFT depending on the physical properties of the agent applied [16,17,18,19]. The data of the current experiment extend these previous findings, showing that a short-time topical anti-inflammatory therapy can increase precorneal TFT. Whereas we have previously shown that there is a correlation between TFT and the severity of DED [20], the threshold TFT value that differentiates DED from normal has not been established. In this context, it needs to be further investigated to what extent changes in TFT reflect clinical changes in DED. Nevertheless our data indicate that hydrocortisone treatment leads to an improvement of TFT towards normal values, which is accompanied by a decrease in hyperemia and may reflect tear film homeostasis.
With respect to the change in subjective parameters, our data shows that there is a significant decrease in OSDI symptoms score in both treatment groups indicating a reduction of symptoms after treatment. However, the OSDI score was still in the pathological range at the end of the study period, indicating that patients still experience symptoms at the end of the study that require clinical follow-up. On the basis of the data in the current study, it remains unclear whether a longer treatment period would have led to a further reduction in symptom scores. However, it needs to be considered that patients were generally satisfied with the treatment as reflected in the VAS scores.
In this context, it needs to be mentioned that the treatment effects on conjunctival redness, OSDI, and TFT were still visible 14 days after the end of the instillation period. This indicates that low dose corticosteroid treatment as used in the current study has a prolonged effect not limited to the actual treatment period and may help to break the viscous circle in patients with DED, which is in keeping with previous reports indicating a long disease-free state after pulse therapy with topical corticosteroids [21]. In contrast to our findings on OSDI, Efron scale, and TFT, no effect on TFBUT or tear film osmolarity was observed after low dose corticosteroid treatment. The reason why the decreases of symptoms and redness are not reflected in signs of DED such as TFBUT or tear film osmolarity is not entirely clear, but might be related to the high variation of these measurements [14, 22]. Further, it is generally known that there is a poor correlation between different signs and symptoms in DED [23].
Finally, although we observed a decrease in HLA-DR expression at the end of the treatment period, this effect did not reach significance. Data from clinical trials show that soluble and cellular inflammatory mediators such as HLA-DR, Intercellular adhesion molecule 1 (ICAM1) and others are increased on the ocular surface of patients with DED [24] and decrease in response to corticosteroid [25] or cyclosporine A treatment [26]. The current study was, however, not designed and powered to detect changes in HLA-DR. Patients included in the aforementioned studies had longer treatment periods and more severe DED compared to the current study, which might well explain the more pronounced reduction in HLA-DR.
Our data is comparable with previous results investigating the effect of corticosteroids on the signs and symptoms of DED. As such, it has been shown in an experimental model of murine dry eye that treatment with topical corticosteroids reduces inflammation paralleled by an improvement of ocular surface damage [27, 28]. These findings are also reflected by data from human studies. Studies mostly performed in patients with severe DED show that treatment with methylprednisolone 1% improves symptoms and corneal staining [29, 30]. Further, data from prospective randomized clinical trials show that with both prednisolone 0.1% and loteprednol etabonate 0.5% administered for 1 month there is an improvement of symptoms, hyperemia, and impression cytology scores in patients with DED [31, 32]. In addition, more recent data show that treatment with loteprednol etabonate or fluorometholone up to 2 months significantly reduces symptoms and conjunctival redness in patients with Sjögren’s syndrome or meibomian gland disease [33, 34].
Although treatment with topical corticosteroids is effective, the side effects of commonly used topical steroids such prednisolone or dexamethasone limit their long-term use for the treatment of DED. These adverse effects include ocular hypertension, cataract formation, and infections of the ocular surface, even after short-time administration [29]. Thus, topical corticosteroid treatment is usually recommended only as a short-term pulse therapy in patients not sufficiently responsive to treatment with topical lubricants.
In contrast to the commonly used corticosteroids, the formulation tested in the current study offers considerable advantages. First, the low concentration of only 0.335% and the low penetration of hydrocortisone through the ocular surface reduce the risk of side effects, in particular with respect to IOP increase and cataract formation. Data from the literature suggest that corticosteroids that show less pronounced penetration through the ocular surface such as loteprednol or hydrocortisone are associated with a reduced likelihood for side effects such as IOP increase [35]. This is also in keeping with the good safety profile seen in the current study. Most importantly, our results show that no change in IOP occurred at any of time points within the 4-week study period. Secondly, in contrast to most of the available topical corticosteroid-containing eye drops, the current formulation is PF, which avoids toxic side effect and leads to good tolerability on the ocular surface.
Two different treatment regimens were tested in the current study. Patients received either hydrocortisone for 12 days four times daily followed by 2 days twice daily instillation or alternatively for 8 days three times daily followed by 3 days twice daily. Interestingly, both treatments showed efficacy and a good safety profile, with no statistical difference between the two dosage groups in any of the outcome parameters. As a reduced instillation frequency increases patients’ compliance, reduces topical drug exposure, and is more convenient for the patients, the standard treatment regimen with a three times daily administration might be more appropriate for clinical use.
Some limitations have to be considered when interpreting the results of the current study. First, the study did not include a formal control group. Although a randomized, placebo-controlled study is the gold standard for clinical trials, a placebo selection for dry eye studies is difficult since pharmacologically inactive agents also exert a lubricant effect on the ocular surface. However, the data of the current study may form a basis for a further active controlled randomized study. Furthermore, only a total of 60 patients were included in this trial and the observation time was limited to 14 days after cessation of treatment. A higher number of subjects with a longer observation period may be required to detect changes in clinical signs of DED such as TFBUT. Finally, patients were recruited at different seasons of the year. As environmental conditions could affect DED tests outcomes [36], we cannot fully exclude that different outdoor conditions may have an impact on the study outcome variables.
Conclusion
It was demonstrated in the study that low dose PF hydrocortisone reduces conjunctival redness, increases TFT, and improves symptoms of DED after both treatment schemes. Further, the treatment effect was also visible 2 weeks after the active phase, indicating a prolonged effect of the hydrocortisone treatment. Finally, no change in IOP was seen, which underlines the good safety profile of the hydrocortisone formulation. In conclusion, treatment with low dose PF hydrocortisone appears to be a safe and well-tolerated novel therapeutic approach with corticosteroids for patients with chronic DED.
Change history
10 December 2019
The article “Topical Low Dose Preservative-Free Hydrocortisone Reduces Signs and Symptoms in Patients with Chronic Dry Eye: A Randomized Clinical Trial”, written by Martin Kallab, Stephan Szegedi, Nikolaus Hommer, Hannes Stegmann, Semira Kaya, René M. Werkmeister, Doreen Schmidl, Leopold Schmetterer, Gerhard Garhöfer was originally published electronically on the publisher’s internet portal (currently SpringerLink) on November 19, 2019 without open access.
References
Lemp MA. Report of the national eye institute/industry workshop on clinical trials in dry eyes. CLAO J. 1995;21:221–32.
Lemp MA. Advances in understanding and managing dry eye disease. Am J Ophthalmol. 2008;146:350–6.
Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15:438–510.
Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
Yavuz B, Bozdag Pehlivan S, Unlu N. An overview on dry eye treatment: approaches for cyclosporin a delivery. Sci World J. 2012;2012:194848.
Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15:575–628.
Bielory BP, O’Brien TP, Bielory L. Management of seasonal allergic conjunctivitis: guide to therapy. Acta Ophthalmol. 2012;90:399–407.
Efron N. Grading scales for contact lens complications. Ophthalmic Physiol Opt. 1998;18:182–6.
Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000;118:615–21.
DEWS. Methodologies to diagnose and monitor dry eye disease: report of the Diagnostic Methodology Subcommittee of the International Dry Eye WorkShop. Ocul Surf. 2007;5:108–52.
Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003;22:640–50.
Werkmeister RM, Alex A, Kaya S, et al. Measurement of tear film thickness using ultrahigh-resolution optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54:5578–83.
Nolfi J, Caffery B. Randomized comparison of in vivo performance of two point-of-care tear film osmometers. Clin Ophthalmol. 2017;11:945–50.
Khanal S, Millar TJ. Barriers to clinical uptake of tear osmolarity measurements. Br J Ophthalmol. 2012;96:341–4.
Goppelt-Struebe M. Molecular mechanisms involved in the regulation of prostaglandin biosynthesis by glucocorticoids. Biochem Pharmacol. 1997;53:1389–95.
Wozniak PA, Schmidl D, Bata AM, et al. Effect of different lubricant eye gels on tear film thickness as measured with ultrahigh-resolution optical coherence tomography. Acta Ophthalmol. 2017;95:e307–13.
Schmidl D, Schmetterer L, Witkowska KJ, et al. Tear film thickness after treatment with artificial tears in patients with moderate dry eye disease. Cornea. 2015;34:421–6.
Schmidl D, Werkmeister R, Kaya S, et al. A controlled, randomized double-blind study to evaluate the safety and efficacy of chitosan-N-acetylcysteine for the treatment of dry eye syndrome. J Ocul Pharmacol Ther. 2017;33:375–82.
Kaya S, Schmidl D, Schmetterer L, et al. Effect of hyaluronic acid on tear film thickness as assessed with ultra-high resolution optical coherence tomography. Acta Ophthalmol. 2015;93:439–43.
Schmidl D, Witkowska KJ, Kaya S, et al. The association between subjective and objective parameters for the assessment of dry-eye syndrome. Invest Ophthalmol Vis Sci. 2015;56:1467–72.
Hong S, Kim T, Chung SH, Kim EK, Seo KY. Recurrence after topical nonpreserved methylprednisolone therapy for keratoconjunctivitis sicca in Sjogren’s syndrome. J Ocul Pharmacol Ther. 2007;23:78–82.
Nichols JJ, Nichols KK, Puent B, Saracino M, Mitchell GL. Evaluation of tear film interference patterns and measures of tear break-up time. Optom Vis Sci. 2002;79:363–9.
Sullivan BD, Crews LA, Messmer EM, et al. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications. Acta Ophthalmol. 2014;92:161–6.
Pflugfelder SC, Stern M, Zhang S, Shojaei A. LFA-1/ICAM-1 Interaction as a therapeutic target in dry eye disease. J Ocul Pharmacol Ther. 2017;33:5–12.
Aragona P, Spinella R, Rania L, et al. Safety and efficacy of 01% clobetasone butyrate eyedrops in the treatment of dry eye in Sjogren syndrome. Eur J Ophthalmol. 2013;23:368–76.
Leonardi A, Van Setten G, Amrane M, et al. Efficacy and safety of 0.1% cyclosporine A cationic emulsion in the treatment of severe dry eye disease: a multicenter randomized trial. Eur J Ophthalmol. 2016;26:287–96.
De Paiva CS, Corrales RM, Villarreal AL, et al. Corticosteroid and doxycycline suppress MMP-9 and inflammatory cytokine expression, MAPK activation in the corneal epithelium in experimental dry eye. Exp Eye Res. 2006;83:526–35.
Lekhanont K, Leyngold IM, Suwan-Apichon O, Rangsin R, Chuck RS. Comparison of topical dry eye medications for the treatment of keratoconjunctivitis sicca in a botulinum toxin B-induced mouse model. Cornea. 2007;26:84–9.
Marsh P, Pflugfelder SC. Topical nonpreserved methylprednisolone therapy for keratoconjunctivitis sicca in Sjogren syndrome. Ophthalmology. 1999;106:811–6.
Sainz MD, Simon Castellvi C, Kabbani O. Nonpreserved topical steroids and lacrimal punctal occlusion for severe keratoconjunctivitis sicca. Arch Soc Esp Oftalmol. 2000;75:751–6.
Pflugfelder SC, Maskin SL, Anderson B, et al. A randomized, double-masked, placebo-controlled, multicenter comparison of loteprednol etabonate ophthalmic suspension, 0.5%, and placebo for treatment of keratoconjunctivitis sicca in patients with delayed tear clearance. Am J Ophthalmol. 2004;138:444–57.
Lee HK, Ryu IH, Seo KY, Hong S, Kim HC, Kim EK. Topical 0.1% prednisolone lowers nerve growth factor expression in keratoconjunctivitis sicca patients. Ophthalmology. 2006;113:198–205.
Kheirkhah A, Dohlman TH, Amparo F, et al. Effects of corneal nerve density on the response to treatment in dry eye disease. Ophthalmology. 2015;122:662–8.
Pinto-Fraga J, Lopez-Miguel A, Gonzalez-Garcia MJ, et al. Topical fluorometholone protects the ocular surface of dry eye patients from desiccating stress: a randomized controlled clinical trial. Ophthalmology. 2016;123:141–53.
Sheppard JD, Comstock TL, Cavet ME. Impact of the topical ophthalmic corticosteroid loteprednol etabonate on intraocular pressure. Adv Ther. 2016;33:532–52.
Teson M, Lopez-Miguel A, Neves H, Calonge M, Gonzalez-Garcia MJ, Gonzalez-Meijome JM. Influence of climate on clinical diagnostic dry eye tests: pilot study. Optom Vis Sci. 2015;92:e284–9.
Acknowledgements
Funding
The present study was sponsored by Laboratories Thea, France. The Rapid Service Fees were funded by Laboratories Thea. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Doreen Schmidl is a consultant for Laboratories Thea. Leopold Schmetterer is a consultant for Laboratories Thea. Gerhard Garhöfer is a consultant for Laboratories Thea. Martin Kallab, Stephan Szegedi, Nikolaus Hommer, Hannes Stegmann, Semira Kaya, and René M. Werkmeister declare that they have no conflict of interest.
Compliance with Ethics Guidelines
The study protocol was approved by the Ethics Committee of the Medical University of Vienna. The study was performed in adherence to the guidelines of the Declaration of Helsinki including all revisions as well as Good Clinical Practice guidelines. Written informed consent was obtained from all study participants prior to participation and Springer’s policy concerning informed consent has been followed.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original version of this article was revised due to retrospective open access.
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.10013162.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kallab, M., Szegedi, S., Hommer, N. et al. Topical Low Dose Preservative-Free Hydrocortisone Reduces Signs and Symptoms in Patients with Chronic Dry Eye: A Randomized Clinical Trial. Adv Ther 37, 329–341 (2020). https://doi.org/10.1007/s12325-019-01137-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-019-01137-8