Summary
This short review reflects on a personal selection of three abstracts on colorectal cancer (CRC) presented at the 2021 ESMO Congress: (1) KRASG12C as a new therapeutic target in metastatic CRC, supported by data from the KRYSTAL‑1 and CodeBreaK101 trials, (2) positive phase 3 data on the possible role of selective internal radiotherapy (SIRT) in the second-line treatment of liver-limited metastatic CRC, and (3) the impact of the coronavirus disease 2019 (COVID-19) pandemic on CRC screening, management and mortality, now and in the upcoming years.
Similar content being viewed by others
Targeted therapy in KRAS G12C-mutated metastatic CRC
Although KRAS is one of the most frequently mutated genes in colorectal cancer (CRC), only 3–4% of all patients with metastatic CRC exhibit a KRAS G12C mutation [1]. KRAS G12C is a point mutation in the KRAS gene resulting in a glycine-to-cysteine amino acid substitution at codon 12, thereby, leading to constitutive activation and oncogenesis. These patients show a worse prognosis when compared to patients with non-KRAS G12C mutated disease.
Adagrasib is a covalent inhibitor of KRAS G12C which irreversibly and selectively binds to KRAS G12C [2]. In the KRYSTAL‑1 phase 1/2 trial, adagrasib was investigated as monotherapy (n = 46) or in combination with the anti-EGFR antibody cetuximab (n = 32) in heavily pretreated KRAS G12C-mutated metastatic CRC [3]. This combination is based on the rationale that EGFR signaling has been identified as the dominant mechanism of CRC resistance to KRAS G12C inhibitors [4].
Adagrasib alone resulted in an overall response rate (ORR) of 22% and disease control rate (DCR) of 87% among 45 evaluable patients. Median progression-free survival (PFS) for monotherapy was 5.6 months (95% confidence interval [CI] 4.1–8.3). The addition of cetuximab could increase clinical efficacy to an ORR of 43% and DCR of 100% among 28 evaluable patients. Here, median time to response was 1.3 months and 71% of patients remained on treatment at the time of analysis. Grade 3/4 adverse events for combination therapy could be observed in 16% of patients, with diarrhea, acneiform rash, stomatitis and QTc prolongation being the most frequent (each 3%).
Based on these results, adagrasib and cetuximab is compared to standard chemotherapy plus/minus antiangiogenic agent in the KRYSTAL-10 trial, a phase 3 randomized trial in patients with KRAS G12C mutated metastatic CRC who have progressed after first-line treatment (NCT04793958).
These data are supported by another trial: in the phase Ib CodeBreaK101 trial, sotorasib, another KRAS G12C inhibitor, was investigated in combination with the anti-EGFR antibody panitumumab in 31 chemorefractory patients [5]. The investigators reported a confirmed plus unconfirmed ORR of 27% and a DCR of 81%.
Sotorasib is already approved by the European Medicines Agency for the treatment of patients with advanced non-small cell lung cancer whose tumors harbor a KRAS G12C mutation and who have progressed after at least one prior line of systemic therapy [6].
The combination of sotorasib and panitumumab will be investigated in the CodeBreak300 trial, a phase 3 randomized trial in patients with KRAS G12C mutated metastatic CRC in the third-line setting (NCT04793958).
First positive phase 3 trial for selective internal radiotherapy in CRC
Selective internal radiotherapy (SIRT) or radioembolization describes the transarterial delivery of microscopic glass beads containing radioactive yttrium (Y-90) to liver metastases through hepatic tumor-feeding arteries.
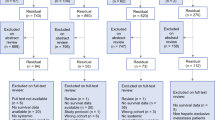
The EPOCH trial investigated the role of SIRT when added to standard second-line chemotherapy in patients with metastatic CRC limited to the liver [7].
In this phase 3 study, 428 patients were randomized to either chemotherapy alone or the combination with SIRT applied in a single setting, before or after the first cycle of chemotherapy. Both primary endpoints were met, with a slight increase in median PFS (8.0 vs 7.2 months, hazard ratio [HR] 0.69; 95% CI, 0.54–0.88; p = 0.0013) as well as in median hepatic PFS (9.1 vs 7.2 months, HR 0.59, p = 0.0019) when adding SIRT. Moreover, ORR was also higher in the combination arm with 34.0% compared to 21.1% with chemotherapy alone. However, this did not translate into an increased median overall survival (14.0 vs 14.4 months, HR 1.07, p = 0.7229).
Grade 3 adverse events—especially neutropenia—were reported more frequently with SIRT (68.4% vs 49.3%) but not leading to dose reductions in chemotherapy.
So after failing to show an improvement in PFS or OS in the first-line setting [8], adding SIRT to standard chemotherapy to liver-limited metastatic CRC may be beneficial in the second-line setting.
Impact of the COVID-19 pandemic on CRC screening and diagnosis
Due to the immense challenges posed by the coronavirus disease 2019 (COVID-19) pandemic to health care systems worldwide, cancer screening programs had to be scaled back or were not sought by patients out of fear of COVID-19 infection.
At ESMO 2021, Tehfe M et al. presented their analysis of data of the Canadian province of Quebec regarding fecal occult blood test and colonoscopy for CRC screening, as well as CRC surgery [9]. When comparing the 4‑month period during the first wave of the pandemic (April–July 2020) to the same time period in the preceding year (April–July 2019), the researchers could observe a dramatic drop in CRC screening but also CRC surgeries (Table 1).
Although prior to the second wave (August–October 2020) many health care services could be resumed, CRC screening was still less than in the previous year (fecal occult blood test: −5%, colonoscopy: −11.4%) as were CRC surgeries (−28%).
These data are in line with other reports [10] and exemplify how the COVID-19 pandemic is impacting CRC management. Since CRC survival is closely linked to stage of disease [11], the delays in diagnosis of CRC are expected to lead to a stage-shift at first diagnosis as well as in an increase in emergency admissions, both known to negatively affect prognosis in CRC [12].
References
Henry J, Coker O, Chowdhury S, et al. Comprehensive clinical and molecular characterization of KRASG12C-mutant colorectal cancer. JCO Precis Oncol. 2021;5:613–21.
Hallin J, Engstrom LD, Hargi L, Calinisan A, Aranda R, Briere DM, et al. The KRAS G12C Inhibitor MRTX849 Provides Insight toward Therapeutic Susceptibility of KRAS-Mutant Cancers in Mouse Models and Patients. Cancer Discov. 2020;10(1):54–71.
Weiss J, Yaeger R, Johnson M, et al. KRYSTAL-1: adagrasib (MRTX849) as monotherapy or combined with cetuximab (Cetux) in patients (Pts) with colorectal cancer (CRC) harboring a KRASG12C mutation. Ann Oncol. 2021;32:S1283–S96.
Amodio V, Yaeger R, Arcella P, et al. EGFR blockade reverts resistance to KRAS G12C inhibition in colorectal cancer. Cancer Discov. 2020;10:1129–39.
Fakih M, Falchook G, Hong D, et al. CodeBreaK 101 subprotocol H: phase Ib study evaluating combination of sotorasib (Soto), a KRASG12C inhibitor, and panitumumab (PMab), an EGFR inhibitor, in advanced KRAS p.G12C-mutated colorectal cancer (CRC). Ann Oncol. 2021;32:S530–S82.
Skoulidis F, Li B, Dy G, et al. Sotorasib for lung cancers with KRAS p.G12C mutation. N Engl J Med. 2021;384:2371–81.
Radioembolization with chemotherapy for colorectal liver metastases: A randomized, open-label, international, multicenter, phase III trial (EPOCH s…) | OncologyPRO. https://oncologypro.esmo.org/meeting-resources/esmo-congress/radioembolization-with-chemotherapy-for-colorectal-liver-metastases-a-randomized-open-label-international-multicenter-phase-iii-trial-epoch-s. Accessed 15 Feb 2022.
Wasan HS, Gibbs P, Sharma N, Taieb J, Heinemann V, Ricke J, et al. First-line selective internal radiotherapy plus chemotherapy versus chemotherapy alone in patients with liver metastases from colorectal cancer (FOXFIRE, SIRFLOX, and FOXFIRE-Global): a combined analysis of three multicentre, randomised, phase 3 trials. Lancet Oncol. 2017;18(9):1159–71.
Colorectal (CRC) cancer screening and diagnosis during the COVID-19 pandemic in Quebec, Canada | OncologyPRO. https://oncologypro.esmo.org/meeting-resources/esmo-congress/colorectal-crc-cancer-screening-and-diagnosis-during-the-covid-19-pandemic-in-quebec-canada. Accessed 20 Feb 2022.
Morris EJA, Goldacre R, Spata E, Mafham M, Finan PJ, Shelton J, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021;6(3):199–208.
Bowel cancer survival statistics | Cancer Research UK. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer/survival. Accessed 20 Feb 2022.
Mcphail S, Elliss-Brookes L, Shelton J, Ives A, Greenslade M, Vernon S, et al. Emergency presentation of cancer and short-term mortality. Br J Cancer. 2013;109(8):2027–34.
Funding
Open access funding provided by Paracelsus Medical University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
L. Weiss: Honoraria: Amgen, Bayer, BMS, Lilly, Merck, MSD, Nordic Pharma, Roche, Sanofi; Consulting: Lilly, Merck; Research Funding: Roche, Novocure.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.