Abstract
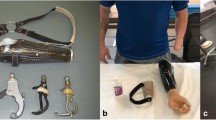
Loss of an isolated upper limb is an emotionally and physically devastating event that results in significant impairment. Patients who lose both upper extremities experience profound disability that affects nearly every aspect of their lives. While prosthetics and surgery can eventually provide the single limb amputee with a suitable assisting hand, limited utility, minimal haptic feedback, weight, and discomfort are persistent problems with these techniques that contribute to high rates of prosthetic rejection. Moreover, despite ongoing advances in prosthetic technology, bilateral amputees continue to experience high levels of dependency, disability, and distress. Hand and upper extremity transplantation holds several advantages over prosthetic rehabilitation. The missing limb is replaced with one of similar skin color and size. Sensibility, voluntary motor control, and proprioception are restored to a greater degree, and afford better dexterity and function than prosthetics. The main shortcomings of transplantation include the hazards of immunosuppression, the complications of rejection and its treatment, and high cost. Hand and upper limb transplantation represents the most commonly performed surgery in the growing field of Vascularized Composite Allotransplantation (VCA). As upper limb transplantation and VCA have become more widespread, several important challenges and controversies have emerged. These include: refining indications for transplantation, optimizing immunosuppression, establishing reliable criteria for monitoring, diagnosing, and treating rejection, and standardizing outcome measures. This article will summarize the historical background of hand transplantation and review the current literature and concepts surrounding it.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Grob M, Papadopulos NA, Zimmerman A, et al. The psychological impact of severe hand injury. J Hand Surg Eur. 2008;33:358–62.
Grunert BK, Smith CJ, Devine CA, et al. Early psychological aspects of severe hand injury. J Hand Surg (Br). 1998;13:177–80.
Wright TW, Hagen AD, Wood MB. Prosthetic usage in major upper extremity amputations. J Hand Surg [Am]. 1995;20:619–22.
Foroohar A, Elliott RM, Kim TWB, et al. The history and evolution of hand transplantation. Hand Clin. 2011;27:405–9.
Peacock EE. A review of composite tissue allografts of the digital flexor mechanism. TPS. 1976;8:119–27.
Peacock EE. Homologous composite tissue grafts of the digital flexor mechanism in human beings. Transplant Bull. 1960;7:418–21.
Peacock EE, Madden JW. Human composite flexor tendon allografts. Ann Surg. 1967;166:624–9.
Gilbert R. Transplant is successful with a cadaver forearm. Med Trib Med News. 1964;5:20–3.
Benhaim P, Anthony JP, Lin LY, et al. A long-term study of allogenic rat hindlimb transplants immunosuppressed with RS-61443. Transplantation. 1993;56:911–7.
Ustuner ET, Zdichavsky M, Ren X, et al. Long-term composite tissue allograft survival in a porcine model with cyclosporine/mycophenolate mofetil therapy. Transplantation. 1998;66:1581–7.
Jones Jr JW, Ustuner ET, Zdichavsky, et al. Long-term survival of an extremity composite tissue allograft with FK506-mycophenolate mofetil therapy. Surgery. 1999;126:384–8.
Dubernard JM, Owen E, Lefranois N, et al. First human hand transplantation case report. Transpl Int. 2000;13:S521–7.
Dubernard JM, Owen E, Herzberg G, et al. Human hand allograft: report on first 6 months. Lancet. 1999;353:1315–20.
Jones JW, Gruber SA, Barker JH, et al. Successful hand transplantation. One year follow-up. Louisville hand transplant team. N Engl J Med. 2000;343:468–73.
Breidenbach WC, Gonzales R, Kaufman CL, et al. Outcomes of the first 2 American hand transplants at 8 and 6 years post-transplant. J Hand Surg. 2008;33:1039–47.
Pertuzzo P, Badet C, Gazarian A, et al. Bilateral hand transplantation: six years after the first case. Am J Transplant. 2006;6:1718–24.
Hollenbeck ST, Erdmann D, Levin LS. Current indications for hand and face transplantation. Transplant Proc. 2009;41:495–8.
Petruzzo P, Lanzetta M, Dubernard JM, et al. The international registry on hand and composite tissue transplantation. Transplantation. 2010;90:1590–4.
• Petruzzo P, Dubernard JM. The international registry on hand and composite tissue allotransplantation. Clin Transpl. 2011:247–53. Reports the most current aggregate data from the international hand transplant registry. Note that several leading centers do not share data with the registry.
Brandacher G, Ninkovic M, Piza-Katzer H, et al. The Innsbruck hand transplant program: update at 8 years after the first hand transplant. Transplant Proc. 2009;41:491–4.
Cavadas PC, Ibanez J, Thione A, et al. Bilateral trans-humeral arm transplantation: result at 2 years. Am J Transplant. 2011;11:1085–90.
Stangl MJ, Biemer E, Nerlich A, et al. Three year immunological follow-up of the first bilateral arm transplant world-wide. Transplantation. 2012;94:346.
Jensen SE, Butt Z, Bill A, et al. Quality of life considerations in upper limb transplantation: review and future directions. J Hand Surg [Am]. 2012;37:2126–35.
Murray JE. Organ transplantation (skin, kidney, heart) and the plastic surgeon. Plast Reconstr Surg. 1971;47:425–31.
Brouha P, Naidu D, Cunningham M, et al. Risk acceptance in composite-tissue allotransplantation reconstructive procedures. Microsurgery. 2006;26:144–9.
Brandacher G, Gorantla VS, Lee WP. Hand allotransplantation. Semin Plast Surg. 2010;24:11–7.
Schneeberger S, Gorantla VS, Hautz T, et al. Immunosuppression and rejection in human hand transplantation. Transplant Proc. 2009;41:472–5.
Shores JT, Imbriglia JE, Lee WP. The current state of hand transplantation. J Hand Surg [Am]. 2011;36:1862–7.
Hautz T, Brandacher G, Zelger B, et al. Immunologic aspects and rejection in solid organ vs reconstructive transplantation. Transplantation. 2010;42:3347–53.
•• Schneeberger S, Gorantla VS, Brandacher G, et al. Upper-extremity transplantation using a cell-based protocol to minimize immunosuppression. Ann Surg. 2013;257:345–51. Outlines the “Pittsburgh Protocol”- a novel and promising method that uses donor bone marrow infusion at the time of transplant in an attempt to induce chimerism in the recipient leading to single drug immunosuppression.
Starzl TE, Zinkernagel RM. Antigen localization and migration in immunity and tolerance. N Engl J Med. 1998;339:1905–13.
Starzl TE, Murase N, Abu-Elmagd, et al. Tolerogenic immunosuppression for organ transplantation. Lancet. 2003;361:1502–10.
Fontes P. Bone marrow augmentation of donor-cell chimerism in kidney, liver, heart, and pancreas islet transplantation. Lancet. 1994;344:151–5.
Ciancio G, Miller J, Garcia-Morales RO, et al. Six-year clinical effect of donor bone marrow infusions in renal transplant patients. Transplantation. 2001;71:827–35.
Ildstad ST, Sachs DH. Reconstitution with syngeneic plus allogeneic or xenogeneic bone marrow leads to specific acceptance of allografts or xenografts. Nature. 1984;307:168–70.
Wu S, Xu H, Ravindra K, et al. Composite tissue allotransplantation: past, present, and future-the history and expanding applications of CTA as a new frontier in transplantation. Transplant Proc. 2009;41:463–5.
Birch R. Nerve repair. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, editors. Green’s operative hand surgery. Philadelphia: Elsevier; 2011. p. 1035–74.
Tanaka K, Fujita N, Higashi Y, et al. Neuroprotective and antioxidant properties of FKBP-binding immunophilin ligands are independent on the FKBP12 pathway in human cells. Neurosci Lett. 2002;330:147–50.
Yan Y, Sun HH, Hunter DA, et al. Efficacy of short-term FK506 administration on accelerating nerve regeneration. Neurorehabil Neural Repair. 2012;26:570–80.
Moore AM, Ray WZ, Chenard KE, et al. Nerve allotransplantation as it pertains to composite tissue transplantation. Hand. 2009;4:239–44.
Mackinnon SE, Doolabh VB, Novack CB, et al. Clinical outcome following nerve allograft transplantation. Plast Reconstr Surg. 2001;107:1419–29.
Compliance with Ethics Guidelines
Conflict of Interest
River M. Elliott declares that he has no conflict of interest. Scott M. Tintle declares that he has no conflict of interest. L. Scott Levin declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elliott, R.M., Tintle, S.M. & Levin, L.S. Upper extremity transplantation: current concepts and challenges in an emerging field. Curr Rev Musculoskelet Med 7, 83–88 (2014). https://doi.org/10.1007/s12178-013-9191-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-013-9191-x