Abstract
Purpose
We report an update of current methods for colorectal cancer (CRC) screening based on fecal sample analysis.
Methods
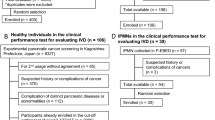
A systematic review of the literature was performed in MEDLINE, EMBASE, and Science Direct electronic databases.
Results
Blood in the stools is the first and most used strategy. Fecal occult blood test (FOBT) and fecal immunochemical test (FIT) are the main methods. Both are economic, easy to perform with high specificity, and low sensitivity. Based on CRC multi-step process with genetic and epigenetic alterations in large bowel cell DNA, single mutations or panels of alterations have been detected. These tests have the advantage of a marked improvement of the sensitivity when compared to fecal blood. However, high costs, poor availability, and correct choice of marker panel represent the major limits. A specific sDNA panel including aberrantly methylated BMP3 and NDRG4 promoter regions, mutant k-ras and β-actin (a reference gene for human DNA quantity), and an immunochemical assay for human hemoglobin has been recently approved by Food and Drug Administration. Novel promising biomarkers for CRC screening are represented by microRNAs (miRNAs), a group of 18-25 nucleotide non-coding RNA molecules that regulate gene expression. Reports on these fecal biomarkers are case-control studies, and each of them evaluates single miRNAs or multi-target panels. On the other hand, some fecal proteins have been studied as possible CRC screening markers, even though they demonstrated poor results. Finally, alterations of estrogen receptor-beta (i.e., dramatic reduction in the early stage of CRC) have been demonstrated in tissue samples.
Conclusions
Specific investigations are warranted in order to add further noninvasive markers to the panel of CRC screening tools.

Similar content being viewed by others
References
Ferlay J, Shin HR, Bray F, et al. GLOBOCAN 2008 v2.0, cancer incidence and mortality worldwide: IARC cancer base no. 10 [internet]. Lyon, France: International Agency for Research on Cancer; 2010.
Lofano K, Principi M, Scavo MP, Pricci M, Ierardi E, Di Leo A. Dietary lifestyle and colorectal cancer onset, recurrence, and survival: myth or reality? J Gastrointest Cancer. 2013;44(1):1–11.
Barone M, Lofano K, De Tullio N, Licinio R, Albano F, Di Leo A. Dietary, endocrine, and metabolic factors in the development of colorectal cancer. J Gastrointest Cancer. 2012;43(1):13–9.
Loughrey MB, Shepherd NA. The pathology of bowel cancer screening. Histopathology. 2015;66(1):66–77.
Kaemmerer E, Klaus C, Jeon MK, Gassler N. Molecular classification of colorectal carcinomas: the genotype-to-phenotype relation. World J Gastroenterol. 2013;19(45):8163–7.
Garborg K, Holme Ø, Løberg M, Kalager M, Adami HO, Bretthauer M. Current status of screening for colorectal cancer. Ann Oncol. 2013;24(8):1963–72.
Young GP. Population-based screening for colorectal cancer: Australian research and implementation. J Gastroenterol Hepatol. 2009;24 Suppl 3:S33–42.
Sinatra MA, St John DJ, Young GP. Interference of plant peroxidases with guaiac-based fecal occult blood tests is avoidable. Clin Chem. 1999;45:123–6.
Ciatto S, Martinelli F, Castiglione G, et al. Association of FOBT-assessed faecal Hb content with colonic lesions detected in the Florence screening programme. Br J Cancer. 2007;96(2):218–21.
Parente F, Bargiggia S, Boemo C, et al. Anatomic distribution of cancers and colorectal adenomas according to age and sex and relationship between proximal and distal neoplasms in an i-FOBT-positive average-risk Italian screening cohort. Int J Colorectal Dis. 2014;29(1):57–64.
Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134(5):1570–95.
Hardcastle JD, Chamberlain JO, Robinson MH, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348:1472–7.
Kronborg O, Fenger C, Olsen J, et al. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348:1467–71.
Lindholm E, Brevinge H, Haglind E. Survival benefit in a randomized clinical trial of faecal occult blood screening for colorectal cancer. Br J Surg. 2008;95:1029–36.
Mandel JS, Church TR, Ederer F, et al. Colorectal cancer mortality: effectiveness of biennial screening for fecal occult blood. J Natl Cancer Inst. 1999;91:434–7.
Scholefield JH, Moss SM, Mangham CM, et al. Nottingham trial of faecal occult blood testing for colorectal cancer: a 20-year follow-up. Gut. 2012;61:1036–40.
Mandel JS, Church TR, Bond JH, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343:1603–7.
Kronborg O, Jorgensen OD, Fenger C, et al. Randomized study of biennial screening with a faecal occult blood test: results after nine screening rounds. Scand J Gastroenterol. 2004;39:846–51.
Hewitson P, Glasziou P, Irwig L, et al. Screening for colorectal cancer using the faecal occult blood test, Hemoccult. Cochrane Database Syst Rev. 2007;1, CD001216.
Segnan N, Patnick J, Karsa L. European guidelines for quality assurance in colorectal cancer screening and diagnosis. Luxembourg: Office for Official Publications of the European Communities; 2010.
Hundt S, Haug U, Brenner H. Comparative evaluation of immunochemical fecal occult blood tests for colorectal adenoma detection. Ann Intern Med. 2009;150:162–9.
Guittet L, Bouvier V, Mariotte N, et al. Comparison of a guaiac and an immunochemical faecal occult blood test for the detection of colonic lesions according to lesion type and location. Br J Cancer. 2009;100:1230–5.
Grazzini G, Visioli CB, Zorzi M, et al. Immunochemical faecal occult blood test: number of samples and positivity cutoff. What is the best strategy for colo-rectal cancer screening? Br J Cancer. 2009;100:259–65.
Levi Z, Rozen P, Hazazi R, et al. A quantitative immunochemical fecal occult blood test for colorectal neoplasia. Ann Intern Med. 2007;146:244–55.
Whitlock EP, Lin JS, Liles E, et al. Screening for colorectal cancer: a targeted, updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149:638–58.
Hol L, van Leerdam ME, van Ballegooijen M, et al. Screening for colorectal cancer: randomised trial comparing guaiac-based and immunochemical faecal occult blood testing and flexible sigmoidoscopy. Gut. 2010;59:62–8.
Levi Z, Birkenfeld S, Vilkin A, et al. A higher detection rate for colorectal cancer and advanced adenomatous polyp for screening with immunochemical fecal occult blood test than guaiac fecal occult blood test, despite lower compliance rate. A prospective, controlled, feasibility study. Int J Cancer. 2011;128:2415–24.
Levi Z, Hazazi R, Rozen P, et al. A quantitative immunochemical faecal occult blood test is more efficient for detecting significant colorectal neoplasia than a sensitive guaiac test. Aliment Pharmacol Ther. 2006;23:1359–64.
Dawson MA, Kouzarides T. Cancer epigenetics: from mechanism to therapy. Cell. 2012;150:12–27.
Sidransky D, Tokino T, Hamilton SR, et al. Identification of ras oncogene mutations in the stool of patients with curable colorectal tumors. Science. 1992;256:102–5.
Robertson DJ, Imperiale TF. Stool testing for colorectal cancer. Gastroenterology. 2015. doi:10.1053/j.gastro.2015.05.045 [article in press].
Villa E, Dugani A, Rebecchi AM, et al. Identification of subjects at risk for colorectal carcinoma through a test based on K-ras determination in the stool. Gastroenterology. 1996;110:1346–53.
Ratto C, Flamini G, Sofo L, et al. Detection of oncogene mutation from neoplastic colonic cells exfoliated in feces. Dis Colon Rectum. 1996;39(11):1238–44.
Traverso G, Shuber A, Levin B, et al. Detection of APC mutations in fecal DNA from patients with colorectal tumors. N Engl J Med. 2002;346(5):311–20.
Notarnicola M, Cavallini A, Cardone R, Pezzolla F, Demma I, Di Leo A. K-ras and p53 mutations in DNA extracted from colonic epithelial cells exfoliated in faeces of patients with colorectal cancer. Dig Liver Dis. 2000;32(2):131–6.
Coppedè F, Lopomo A, Spisni R, Migliore L. Genetic and epigenetic biomarkers for diagnosis, prognosis and treatment of colorectal cancer. World J Gastroenterol. 2014;20(4):943–56.
Luo YX, Chen DK, Song SX, Wang L, Wang JP. Aberrant methylation of genes in stool samples as diagnostic biomarkers for colorectal cancer or adenomas: a meta-analysis. Int J Clin Pract. 2011;65:1313–20.
Yang H, Xia BQ, Jiang B, et al. Diagnostic value of stool DNA testing for multiple markers of colorectal cancer and advanced adenoma: a meta-analysis. Can J Gastroenterol. 2013;27(8):467–75.
Guo Q, Song Y, Zhang H, Wu X, Xia P, Dang C. Detection of hypermethylated fibrillin-1 in the stool samples of colorectal cancer patients. Med Oncol. 2013;30:695.
Toyota M, Suzuki H. Epigenetic drivers of genetic alterations. Adv Genet. 2010;70:309–23.
You JS, Jones PA. Cancer genetics and epigenetics: two sides of the same coin? Cancer Cell. 2012;22:9–20.
Imperiale TF, Ransohoff DF, Itzkowitz SH, et al. Fecal DNA versus fecal occult blood for colorectal-cancer screening in an average-risk population. N Engl J Med. 2004;351:2704–14.
Ahlquist DA, Sargent DJ, Loprinzi CL, et al. Stool DNA and occult blood testing for screen detection of colorectal neoplasia. Ann Intern Med. 2008;149:441–50. w81.
Ahlquist DA, Zou H, Domanico M, et al. Next-generation stool DNA test accurately detects colorectal cancer and large adenomas. Gastroenterology. 2012;142:248–56.
Imperiale TF, Ransohoff DF, Itzkowitz SH, et al. Multitarget stool DNA testing for colorectal-cancer screening. N Engl J Med. 2014;370(14):1287–97.
Smith RA, Manassaram-Baptiste D, Brooks D, et al. Cancer screening in the United States, 2015: a review of current American cancer society guidelines and current issues in cancer screening. CA Cancer J Clin. 2015;65(1):30–54.
Bartel DP, Lee R, Feinbaum. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–97.
Ren A, Dong Y, Tsoi H, et al. Detection of miRNA as non-invasive biomarkers of colorectal cancer. Int J Mol Sci. 2015;16:2810–23.
Wu CW, Ng SC, Dong Y, et al. Identification of microRNA-135b in stool as a potential noninvasive biomarker for colorectal cancer and adenoma. Clin Cancer Res. 2014;20:2994–3002.
Wu CW, Ng SSM, Dong YJ, et al. Detection of miR-92a and miR-21 in stool samples as potential screening biomarkers for colorectal cancer and polyps. Gut. 2012;61:739–45.
Koga Y, Yasunaga M, Takahashi A, et al. MicroRNA expression profiling of exfoliated colonocytes isolated from feces for colorectal cancer screening. Cancer Prev Res. 2010;3:1435–42.
Ahmed FE, Ahmed NC, Vos PW, et al. Diagnostic microRNA markers to screen for sporadic human colon cancer in stool: I. Proof of principle. Cancer Genomics Proteomics. 2013;10:93–113.
Hoff G, Grotmol T, Thiis-Evensen E, et al. Testing for faecal calprotectin (PhiCal) in the Norwegian Colorectal Cancer Prevention trial on flexible sigmoidoscopy screening: comparison with an immunochemical test for occult blood (FlexSure OBT). Gut. 2004;53:1329–33.
Uppara M, Adaba F, Askari A, Clark S, Hanna G, Athanasiou T, et al. A systematic review and meta-analysis of the diagnostic accuracy of pyruvate kinase M2 isoenzymatic assay in diagnosing colorectal cancer. World J Surg Oncol. 2015;13:48.
Huang JX, Zhou Y, Wang CH, Yuan WW, Zhang ZD, Zhang XF. Tumor M2-pyruvate kinase in stool as a biomarker for diagnosis of colorectal cancer: a meta-analysis. J Cancer Res Ther. 2014;10(Suppl):C225–8.
Leen R, Seng-Lee C, Holleran G, O’Morain C, McNamara D. Comparison of faecal M2-PK and FIT in a population-based bowel cancer screening cohort. Eur J Gastroenterol Hepatol. 2014;26(5):514–8.
Karl J, Wild N, Tacke M, et al. Improved diagnosis of colorectal cancer using a combination of fecal occult blood and novel fecal protein markers. Clin Gastroenterol Hepatol. 2008;6:1122–8.
Olson J, Whitney DH, Durkee K, Shuber AP. DNA stabilization is critical for maximizing performance of fecal DNA-based colorectal cancer tests. Diagn Mol Pathol. 2005;14(3):183–91.
Zauber AG, Lansdorp-Vogelaar I, Wilschut J, Knudsen AB, van Ballegooijen M, Kuntz KM. Cost-effectiveness of DNA stool testing to screen for colorectal cancer [Internet]. Rockville: Agency for Healthcare Research and Quality (US); 2007.
Special report: fecal DNA analysis for colon cancer screening. Technol Eval Cent Asses Program Exec Summ. 2006;21(6):1–2.
Pignone M, Saha S, Hoerger T, Mandelblatt J. Cost-effectiveness analyses of colorectal cancer screening: a systematic review for the U.S. preventive services task force. Ann Int Med. 2002;137(2):96–104.
Fernandez E, La Vecchia C, Balducci A, Chatenoud L, Franceschi S, Negri E. Oral contraceptives and colorectal cancer risk: a meta-analysis. Br J Cancer. 2001;84:722–7.
Chlebowski RT, Wactawski-Wende J, Ritenbaugh C, et al. Women’s health initiative investigators. Estrogen plus progestin and colorectal cancer in postmenopausal women. N Engl J Med. 2004;350:991–1004.
Hendifar A, Yang D, Lenz F, Lurje G, Pohl A, Lenz C, et al. Gender disparities in metastatic colorectal cancer survival. Clin Cancer Res. 2009;15:6391–7.
Long MD, Martin CF, Galanko JA, Sandler RS. Hormone replacement therapy, oral contraceptive use, and distal large bowel cancer: a population-based case-control study. Am J Gastroenterol. 2010;105:1843–50.
Principi M, Scavo MP, Piscitelli D, et al. The sharp decline of beta estrogen receptors expression in long-lasting ulcerative-associated carcinoma. Scand J Gastroenterol. 2015;50(8):1002–10.
Principi M, Barone M, Pricci M, De Tullio N, Losurdo G, Ierardi E, et al. Ulcerative colitis: from inflammation to cancer. Do estrogen receptors have a role? World J Gastroenterol. 2014;20(33):11496–504.
Di Leo A, Barone M, Maiorano E, et al. ER-beta expression in large bowel adenomas: implications in colon carcinogenesis. Dig Liver Dis. 2008;40:260–6.
Weige CC, Allred KF, Allred CD. Estradiol alters cell growth in nonmalignant colonocytes and reduces the formation of preneoplastic lesions in the colon. Cancer Res. 2009;69:9118–24.
Bringiotti R, Ierardi E, De Tullio N, et al. Education and imaging. Gastroenterology: video capsule endoscopy disclosure of unprecedented therapeutic effect of Eviendep on small bowel polyposis in Lynch syndrome. J Gastroenterol Hepatol. 2015;30(5):801.
Calabrese C, Praticò C, Calafiore A, et al. Eviendep(R) reduces number and size of duodenal polyps in familial adenomatous polyposis patients with ileal pouch-anal anastomosis. World J Gastroenterol. 2013;19:5671–7.
Barone M, Tanzi S, Lofano K, et al. Dietary induced ERbeta upregulation counteracts intestinal neoplasia development in intact male ApcMin/+ mice. Carcinogenesis. 2010;31:269–74.
Principi M, Di Leo A, Pricci M, Barone M, et al. Phytoestrogens/insoluble fibers and colonic estrogen receptor β: randomized, double-blind, placebo-controlled study. World J Gastroenterol. 2013;19:4325–33.
Tu Z, Ma Y, Tian J, Li H, Akers W, Achilefu S, et al. Estrogen receptor β potentiates the antiproliferative effect of raloxifene and affects the cell migration and invasion in HCT-116 colon cancer cells. J Cancer Res Clin Oncol. 2012;138:1091–103.
Edvardsson K, Ström A, Jonsson P, Gustafsson JÅ, Williams C. Estrogen receptor beta induces anti-inflammatory and anti-tumorigenic networks in colon cancer cells. Mol Endocrinol. 2011;25:969–79.
Berner C, Aumüller E, Gnauck A, Nestelberger M, Just A, Haslberger AG. Epigenetic control of estrogen receptor expression and tumor suppressor genes is modulated by bioactive food compounds. Ann Nutr Metab. 2010;57(3–4):183–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Iannone, A., Losurdo, G., Pricci, M. et al. Stool Investigations for Colorectal Cancer Screening: From Occult Blood Test to DNA Analysis. J Gastrointest Canc 47, 143–151 (2016). https://doi.org/10.1007/s12029-016-9810-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-016-9810-z