Abstract
Introduction
Recently, there have been several retrospective reports suggesting an increased frequency in seizures after cardiopulmonary bypass, associated with increased patient morbidity. We sought to prospectively investigate the incidence of electrographic seizures without clear convulsive clinical correlates and subsequent neurologic injury following cardiac surgery.
Methods
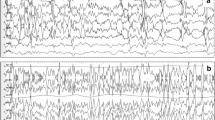
This single-center, prospective, observational study used continuous subhairline electroencephalographic (cEEG) monitoring in the intensive care unit following routine cardiac surgery, ranging from coronary bypass surgery to complex aortic arch reconstruction. The primary outcome was the proportion of patients developing postoperative seizures, as confirmed on cEEG monitoring. Secondary outcomes included neurologic injury, post-operative complications, mortality, and ICU and hospital lengths of stay.
Results
101 consenting patients were included and 3 patients had seizures (2 focal and convulsive, 1 generalized and electrographic). All three patients with seizures were ≥65 years old, had “open-chamber” procedures, and had cardiopulmonary bypass times >120 min. One of the 3 patients with seizures was exposed to higher doses of tranexamic acid. None of the patients with seizures had permanent neurologic sequelae and all were doing well at 1-year follow-up. There was no increased morbidity or mortality in patients with seizures.
Conclusions
Electrographic seizures occur infrequently after cardiac surgery and are generally associated with a good prognosis. Prophylactic cEEG monitoring is unlikely to be cost-effective in this population. (ClinicalTrials.gov Identifier: NCT01291992).



Similar content being viewed by others
References
Roach GW, Kanchuger M, Mangano CM, et al. Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med. 1996;335:1857–63.
Schlag MG, Hopf R, Zifko U, Redl H. Epileptic seizures following cortical application of fibrin sealants containing tranexamic acid in rats. Acta Neurochir. 2002;144:63–9.
Coffey CE, Massey EW, Roberts KB, Curtis S, Jones RH, Pryor DB. Natural history of cerebral complications of coronary artery bypass graft surgery. Neurology. 1983;33:1416–21.
Sugimoto M, Uchida I, Mashimo T, et al. Evidence for the involvement of GABA(A) receptor blockade in convulsions induced by cephalosporins. Neuropharmacology. 2003;45:304–14.
Kalavrouziotis D, Voisine P, Mohammadi S, Dionne S, Dagenais F. High-dose tranexamic acid is an independent predictor of early seizure after cardiopulmonary bypass. Ann Thorac Surg. 2012;93:148–54.
Montes FR, Pardo DF, Carreno M, Arciniegas C, Dennis RJ, Umana JP. Risk factors associated with postoperative seizures in patients undergoing cardiac surgery who received tranexamic acid: a case-control study. Ann Card Anaesth. 2012;15:6–12.
Manji RA, Grocott HP, Leake J, et al. Seizures following cardiac surgery: the impact of tranexamic acid and other risk factors. Can J Anaesth. 2012;59:6–13.
Murkin JM, Falter F, Granton J, Young GB, Burt C, Chu M. High-dose tranexamic acid is associated with nonischemic clinical seizures in cardiac surgical patients. Anesth Analg. 2010;110:350–3.
Martin K, Knorr J, Breuer T, et al. Seizures after open heart surgery: comparison of epsilon-aminocaproic acid and tranexamic acid. J Cardiothorac Vasc Anesth. 2011;25:20–5.
Keyl C, Uhl R, Beyersdorf F, et al. High-dose tranexamic acid is related to increased risk of generalized seizures after aortic valve replacement. Eur J Cardiothorac Surg. 2011;39:e114–21.
Goldstone AB, Bronster DJ, Anyanwu AC, et al. Predictors and outcomes of seizures after cardiac surgery: a multivariable analysis of 2,578 patients. Ann Thorac Surg. 2011;91:514–8.
Bell D, Marasco S, Almeida A, Rowland M. Tranexamic acid in cardiac surgery and postoperative seizures: a case report series. Heart Surg Forum. 2010;13(E257–9):13.
Young GB, Doig GS. Continuous EEG monitoring in comatose intensive care patients: epileptiform activity in etiologically distinct groups. Neurocrit Care. 2005;2:5–10.
Towne AR, Waterhouse EJ, Boggs JG, et al. Prevalence of nonconvulsive status epilepticus in comatose patients. Neurology. 2000;54:340–5.
Gupta SK, Parihar A. Seizures in the Intesive Care Unit. JK Sci. 2000;2:81.
DeLorenzo RJ, Waterhouse EJ, Towne AR, et al. Persistent nonconvulsive status epilepticus after the control of convulsive status epilepticus. Epilepsia. 1998;39:833–40.
Young GB, Jordan KG. Do nonconvulsive seizures damage the brain?–Yes. Arch Neurol. 1998;55:117–9.
Goldstone AB, Bronster DJ, Chikwe J. Seizures after adult cardiac surgery. J Cardiothorac Vasc Anesth. 2011;25:e25–6.
Claassen J, Mayer SA, Kowalski RG. Detection of electrographic seizures with continuous EEG monitoring in critically ill patients. Neurology. 2004;62:1743–8.
Bleck TP, Smith MC, Pierre SJ, Jares JJ, Murray J, Hansen CA. Neurologic complications of critical medical illnesses. Crit Care Med. 1993;21:98–103.
Young GB, Sharpe MD, Savard M, Al Thenayan E, Norton L, Davies-Schinkel C. Seizure detection with a commercially available bedside EEG monitor and the subhairline montage. Neurocrit Care. 2009;11:411–6.
Young GB, McLachlan RS, Kreeft JH, Demelo JD. An electroencephalographic classification for coma. Can J Neurol Sci. 1997;24:320–5.
Levey AS, Greene T. A simplified equation to predict glomerular filtration rate from serum creatinine (Abstr). J Am Soc Nephrol. 2000;11:155A.
Constant I, Seeman R, Murat I. Sevoflurane and epileptiform EEG changes. Paediatr Anaesth. 2005;15(4):266–74.
Murkin JM, Moldenhauer CC, Hug CC Jr, Epstein CM. Absence of seizures during induction of anesthesia with high-dose fentanyl. Anesth Analg. 1984;63(5):489–94.
Kalavrouziotis D, Voisine P, Mohammadi S, Dionne S, Dagenais F. Reply. Ann Thorac Surg. 2012;94:1038–9.
Akula KK, Dhir A, Kulkarni SK. Pro-convulsant effect of cefazolin sodium against pentylenetetrazol- or picrotoxin-induced convulsions in mice. Indian J Exp Biol. 2007;45:720–5.
Furtmuller R, Schlag MG, Berger M, et al. Tranexamic acid, a widely used antifibrinolytic agent, causes convulsions by a gamma-aminobutyric acid(A) receptor antagonistic effect. J Pharmacol Exp Ther. 2002;301:168–73.
Acknowledgments
Many thanks to Drs. Bob Kiaii, Ray Guo, Richard Novick, Neil McKenzie, and Mackenzie Quantz who had patients under their care participate in this study.
Funding Sources
No external funding was received for this study. None of the study authors received compensation, financial or otherwise, for completion of the study.
Sources of Support
None.
Conflict of interest/Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gofton, T.E., Chu, M.W.A., Norton, L. et al. A Prospective Observational Study of Seizures After Cardiac Surgery Using Continuous EEG Monitoring. Neurocrit Care 21, 220–227 (2014). https://doi.org/10.1007/s12028-014-9967-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-9967-x