Abstract
Purpose of Review
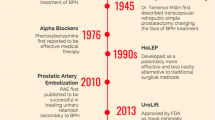
We have reviewed the available evidence on the impact of long-term pharmacological treatment of lower urinary tract symptoms on the outcomes of benign prostatic hyperplasia surgery.
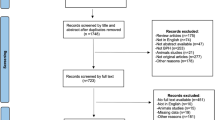
Evidence Acquisition
A systematic literature search from January 1990 to May 2017 was performed. Only references in the English language and peer-reviewed manuscripts were considered.
Recent Findings
Over time, the ever-increasing use of long-term pharmaceutical treatments has considerably reduced the rate of BPH surgery in most countries. In addition, patients undergoing surgery are now generally older, more fragile and with larger prostates. Nevertheless, progress in the surgical field may have compensated for this critical picture and no pejorative trend has been recorded in peri- and post-operative complications and functional outcomes.
Summary
The question whether long-term pharmacological treatment has altered the outcomes of surgical interventions of BPH remains with no clear answer. The call for randomized studies of long-term pharmacological vs surgical treatment of lower urinary tract symptoms due to BPH pharmacological treatment remains valid.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
De Nunzio C, Presicce F, Tubaro A. Combination therapies for improved management of lower urinary tract symptoms/benign prostatic hyperplasia. Drugs Today (Barc). 2016;52(9):501–17.
AUA Practice Guidelines Committee. AUA guideline on management of benign prostatic hyperplasia (2003). Chapter 1: diagnosis and treatment recommendations. J Urol 2003;170:530–47.
•• De Nunzio C, Presicce F, Tubaro A. Inflammatory mediators in the development and progression of benign prostatic hyperplasia. Nat Rev Urol. 2016;13(10):613–26. Inflammatory disorders of the prostate have been considered of importance in the pathophysiology of LUTS but this review makes the case for their possible role in the progression of BPH.
• Denys MA, Decalf V, Goessaert AS, Petrovic M, Van Kerrebroeck P, Everaert K. Lower urinary tract symptoms in an older population: novel concepts for future research. Minerva Urol Nefrol 2016:314-5. An interesting and novel perspective into an old subject.
De Nunzio C, Presicce F, Pirozzi L, Castellan P, Schips L, Cindolo L, et al. The current indications and the benefits of combining a β3-agonist with an anticholinergic for the treatment of OAB. Curr Drug Targets. 2015;16:1198–206.
Pirozzi L, Sountoulides P, Castellan P, Presicce F, Lombardo R, Romero M, et al. Current pharmacological treatment for male LUTS due to BPH: dutasteride or finasteride? Curr Drug Targets. 2015;16:1165–71.
Souverein PC, Erkens JA, de la Rosette JJ, Leufkens HG, Herings RM. Drug treatment of benign prostatic hyperplasia and hospital admission for BPH-related surgery. Eur Urol. 2003;43:528–34.
Malaeb BS, Yu X, AM MB, Elliott SP. National trends in surgical therapy for benign prostatic hyperplasia in the United States (2000–2008). Urology. 2012;79:1111–6.
Izard J, Nickel JC. Impact of medical therapy on transurethral resection of the prostate: two decades of change. BJU Int. 2011;108:89–93.
Vela-Navarrete R, Gonzalez-Enguita C, Garcia-Cardoso JV, Manzarbeitia F, Sarasa-Corral JL, Granizo JJ. The impact of medical therapy on surgery for benign prostatic hyperplasia: a study comparing changes in a decade (1992–2002). BJU Int. 2005;96:1045–8.
•• Cindolo L, Pirozzi L, Fanizza C, Romero M, Sountoulides P, Roehrborn CG, et al. Actual medical management of lower urinary tract symptoms related to benign prostatic hyperplasia: temporal trends of prescription and hospitalization rates over 5 years in a large population of Italian men. Int Urol Nephrol. 2014;46:695–701. This is an administrative database study highlighting the problem of patient compliance to medications for LUTS/BPH and showing how poor adherence to the prescribed medications increases the risk of hospital admission for BPH and BPH surgery. A novel perspective.
Oelke M, Bachmann A, Descazeaud A, Emberton M, Gravos S, Michel MC, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013;64(1):118–40.
Choi SY, Kim TH, Myung SC, Moon YT, Kim KD, Kim YS, et al. Impact of changing trends in medical therapy on surgery for benign prostatic hyperplasia over two decades. Korean J Urol. 2012;53:23–8.
Elkoushy MA, Elshal AM, Elhilali MM. Changing patients’ profile presenting for surgical management of benign prostatic hyperplasia over the past 16 years: a single-centre perspective. Can Urol Assoc J. 2015;9:372–8.
Borth CS, Beiko DT, Nickel JC. Impact of medical therapy on transurethral resection of the prostate: a decade of change. Urology. 2001;57(6):1082–5.
Mayer EK, Kroeze SG, Chopra S, Bottle A, Patel A. Examining the ‘gold standard’: a comparative critical analysis of three consecutive decades of monopolar transurethral resection of the prostate (TURP) outcomes. BJU Int. 2012;110(11):1595–601.
Flanigan RC, Reda DJ, Wasson JH, Anderson RJ, Abdellatif M, Bruskewitz RC. 5-year outcome of surgical resection and watchful waiting for men with moderately symptomatic benign prostatic hyperplasia: a Department of Veterans Affairs cooperative study. J Urol. 1998;160:12–6. >discussion 16–7
He LY, Zhang YC, He JL, Li LX, Wang Y, Tang J, et al. The effect of immediate surgical bipolar plasmakinetic transurethral resection of the prostate on prostatic hyperplasia with acute urinary retention. Asian J Androl. 2016;18:134–9.
Reich O, Gratzke C, Bachmann A, Seitz M, Schlenker B, Hermanek P, et al. Urology Section of the Bavarian Working Group for Quality Assurance. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol 2008;180:246–249.
Djavan B, Madersbacher S, Klingler C, Marberger M. Urodynamic assessment of patients with acute urinary retention: is treatment failure after prostatectomy predictable? J Urol. 1997;158:1829–33.
Negro CL, Muir GH. Chronic urinary retention in men: how we define it, and how does it affect treatment outcome. BJU Int. 2012;110:1590–4.
• Van Koeveringe GA, Rademakers KL. Factors impacting bladder underactivity and clinical implications. Minerva Urol Nefrol. 2015;67:139–48. An interesting read on one of the hottest subject in LUTS and voiding dysfunction.
Blatt AH, Brammah S, Tse V, Chan L. Transurethral prostate resection in patients with hypocontractile detrusor—what is the predictive value of ultrastructural detrusor changes? J Urol. 2012;188:2294–9.
Presicce F, De Nunzio C, Gacci M, Sosnowsky R, Lombardo R, Porpiglia F, et al. The influence of the medical treatment of LUTS on benign prostatic hyperplasia surgery: do we operate too late? Minerva Urol Nefrol. 2017;69(3):242–52.
Oelke M, Kirschner-Hermanns R, Thiruchelvam N, Heesakkers J. Can we identify men who will have complications from benign prostatic obstruction (BPO)? ICI-RS 2011. Neurourol Urodyn. 2012;31:322–6.
Tubaro A, De Nunzio C, Puccini F, Presicce F. The evolving picture of lower urinary tract symptom management. Eur Urol. 2015;67(2):271–2.
Presicce F, De Nunzio C, Gacci M, Finazzi Agrò E, Tubaro A. Non-invasive ultrasound measurements in male patients with LUTS and benign prostatic obstruction: implication for diagnosis and treatment. Minerva Urol Nefrol. 2017;69(3):220–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Fabrizio Presicce declares no potential conflicts of interest.
Cosimo De Nunzio reports personal fees from Jannsen and Pierre Fabre.
Andrea Tubaro reports personal fees from Allergan, Astellas, Bayer and Boston Scientific. Dr. Tubaro is a consultant and/or investigator for Bayer, Boston Scientific, Jannsen and Pierre Fabre and is an unpaid speaker for GSK.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Benign Prostatic Hyperplasia
Rights and permissions
About this article
Cite this article
Presicce, F., De Nunzio, C. & Tubaro, A. Can Long-term LUTS/BPH Pharmacological Treatment Alter the Outcomes of Surgical Intervention?. Curr Urol Rep 18, 72 (2017). https://doi.org/10.1007/s11934-017-0721-8
Published:
DOI: https://doi.org/10.1007/s11934-017-0721-8