Abstract
The disorders of the central nervous system associated with cancer by remote immune-mediated mechanisms are a heterogeneous group. These disorders encompass the classic paraneoplastic disorders and the recently recognized autoimmune encephalitis associated with antibodies against neuronal cell surface or synaptic proteins that occur with or without cancer association. In the last decade, the new surge of interest in neuronal diseases associated with anti-neuronal antibodies led to the rapid discovery of new forms of disease that have different manifestations and were not previously suspected to be immune mediated. The recognition of these syndromes is important because it may lead to early detection of an underlying malignancy and prompt initiation of treatment, improving chances for a better outcome.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lancaster E. Paraneoplastic disorders. Contin Minneap Minn. 2015;21(2 Neuro-oncology):452–75.
Darnell RB, Posner JB. Paraneoplastic syndromes involving the nervous system. N Engl J Med. 2003;349(16):1543–54.
Vedeler CA, Antoine JC, Giometto B, Graus F, Grisold W, Hart IK, et al. Management of paraneoplastic neurological syndromes: report of an EFNS Task Force. Eur J Neurol. 2006;13(7):682–90.
Rosenfeld MR, Titulaer MJ, Dalmau J. Paraneoplastic syndromes and autoimmune encephalitis five new things. Neurol Clin Pract. 2012;2(3):215–23.
Brain WR, Norris FH. The remote effects of cancer on the nervous system. New York: Grune and Stratton; 1965.
Dalmau J, Graus F. Paraneoplastic syndromes: from remote to clear and present knowledge. Brain. 2012;135(5):1650–553.
Wilkinson PC, Zeromski J. Immunofluorescent detection of antibodies against Neurones in sensory carcinomatous neuropathy. Brain. 1965;88(3):529–38.
Trotter JL, Hendin BA, Osterland CK. Cerebellar degeneration with Hodgkin disease: an immunological study. Arch Neurol. 1976;33(9):660–1.
Corsellis JA, Goldberg GJ, Norton AR. “Limbic encephalitis” and its association with carcinoma. Brain J Neurol. 1968;91(3):481–96.
Dalmau J, Furneaux HM, Rosenblum MK, Graus F, Posner JB. Detection of the anti-Hu antibody in specific regions of the nervous system and tumor from patients with paraneoplastic encephalomyelitis/sensory neuronopathy. Neurology. 1991;41(11):1757–64.
Sillevis Smitt P, Manley G, Dalmau J, Posner J. The HuD paraneoplastic protein shares immunogenic regions between PEM/PSN patients and several strains and species of experimental animals. J Neuroimmunol. 1996;71(1–2):199–206.
Voltz R, Dalmau J, Posner JB, Rosenfeld MR. T-cell receptor analysis in anti-Hu associated paraneoplastic encephalomyelitis. Neurology. 1998;51(4):1146–50.
Pellkofer H, Schubart AS, Höftberger R, Schutze N, Pagany M, Schüller M, et al. Modelling paraneoplastic CNS disease: T-cells specific for the onconeuronal antigen PNMA1 mediate autoimmune encephalomyelitis in the rat. Brain. 2004;127(8):1822–30.
Dalmau J, Tüzün E, Wu H, Masjuan J, Rossi JE, Voloschin A, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36.
Lai M, Hughes EG, Peng X, Zhou L, Gleichman AJ, Shu H, et al. AMPA receptor antibodies in limbic encephalitis alter synaptic receptor location. Ann Neurol. 2009;65(4):424–34.
Lancaster E, Lai M, Peng X, Hughes E, Constantinescu R, Raizer J, et al. Antibodies to the GABA B receptor in limbic encephalitis with seizures: case series and characterisation of the antigen. Lancet Neurol. 2010;9(1):67–76.
Lai M, Huijbers MG, Lancaster E, Graus F, Bataller L, Balice-Gordon R, et al. Investigation of LGI1 as the antigen in limbic encephalitis previously attributed to potassium channels: a case series. Lancet Neurol. 2010;9(8):776–85.
Irani SR, Alexander S, Waters P, Kleopa KA, Pettingill P, Zuliani L, et al. Antibodies to Kv1 potassium channel-complex proteins leucine-rich, glioma inactivated 1 protein and contactin-associated protein-2 in limbic encephalitis, Morvan’s syndrome and acquired neuromyotonia. Brain. 2010;133(9):2734–48.
Lancaster E, Huijbers MGM, Bar V, Boronat A, Wong A, Martinez-Hernandez E, et al. Investigations of caspr2, an autoantigen of encephalitis and neuromyotonia. Ann Neurol. 2011;69(2):303–11.
•• Leypoldt F, Armangue T, Dalmau J. Autoimmune encephalopathies. Ann N Y Acad Sci. 2015;1338:94–114. Outstanding review of the autoimmune encephalitis syndromes, clinical features, and immune associations
Vitaliani R, Mason W, Ances B, Zwerdling T, Jiang Z, Dalmau J. Paraneoplastic encephalitis, psychiatric symptoms, and hypoventilation in ovarian teratoma. Ann Neurol. 2005;58(4):594–604.
Sabater L, Gaig C, Gelpi E, Bataller L, Lewerenz J, Torres-Vega E, et al. A novel non-rapid-eye movement and rapid-eye-movement parasomnia with sleep breathing disorder associated with antibodies to IgLON5: a case series, characterisation of the antigen, and post-mortem study. Lancet Neurol. 2014;13(6):575–86.
Dale RC, Irani SR, Brilot F, Pillai S, Webster R, Gill D, et al. N-methyl-D-aspartate receptor antibodies in pediatric dyskinetic encephalitis lethargica. Ann Neurol. 2009;66(5):704–9.
Lancaster E, Dalmau J. Neuronal autoantigens—pathogenesis, associated disorders and antibody testing. Nat Rev Neurol. 2012;8(7):380–90.
Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010;10(12):835–44.
Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA. The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California Encephalitis Project. Clin Infect Dis. 2012;54(7):899–904.
Granerod J, Cousens S, Davies NWS, Crowcroft NS, Sara L. Thomas. New estimates of incidence of encephalitis in England. Emerg Infect Dis. 2013;19(9):1455–62.
Vora NM, Holman RC, Mehal JM, Steiner CA, Blanton J, Sejvar J. Burden of encephalitis-associated hospitalizations in the United States, 1998–2010. Neurology. 2014;82(5):443–51.
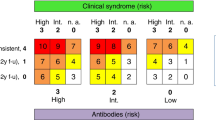
Graus F. Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry. 2004;75(8):1135–40.
Titulaer MJ, Soffietti R, Dalmau J, Gilhus NE, Giometto B, Graus F, et al. Screening for tumours in paraneoplastic syndromes: report of an EFNS Task Force: screening for tumours in PNS. Eur J Neurol. 2011;18(1):19–27.
Honnorat J, Antoine J-C. Paraneoplastic neurological syndromes. Orphanet J Rare Dis. 2007;2:22.
Simabukuro MM, Petit-Pedrol M, Castro LH, Nitrini R, Lucato L, Zambon AA, et al. GABAA receptor and LGI1 antibody encephalitis in a patient with thymoma. Neurol-Neuroimmunol Neuroinflammation. 2015;2(2):e73.
Schmitt SE, Pargeon K, Frechette ES, Hirsch LJ, Dalmau J, Friedman D. Extreme delta brush: a unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology. 2012;79(11):1094–100.
Giometto B, Grisold W, Vitaliani R, Graus F, Honnorat J, Bertolini G. Paraneoplastic neurologic syndrome in the PNS Euronetwork database: a European study from 20 centers. Arch Neurol. 2010;67(3):330–5.
de Graaff E, Maat P, Hulsenboom E, van den Berg R, van den Bent M, Demmers J, et al. Identification of delta/notch-like epidermal growth factor-related receptor as the Tr antigen in paraneoplastic cerebellar degeneration. Ann Neurol. 2012;71(6):815–24.
Rosenfeld MR, Dalmau JO. Paraneoplastic disorders of the CNS and autoimmune synaptic encephalitis. Contin Lifelong Learn Neurol. 2012;18(2, Neuro-oncology):366–83.
•• Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15(4):391–404. A position letter based on literature review and gathered the experience of a team of experts with the aims of developing a practical, syndrome-based diagnostic approach to autoimmune encephalitis and providing guidelines to navigate through the differential diagnosis
Gresa-Arribas N, Titulaer MJ, Torrents A, Aguilar E, McCracken L, Leypoldt F, et al. Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis: a retrospective study. Lancet Neurol. 2014;13(2):1672177.
Dalmau J. Clinical analysis of anti-Ma2-associated encephalitis. Brain. 2004 Jun 16;127(8):1831–1844.
Dalmau J, Graus F, Rosenblum MK, Posner JB. Anti-Hu-associated paraneoplastic encephalomyelitis/sensory neuronopathy. A clinical study of 71 patients. Medicine (Baltimore). 1992;71(2):59–72.
Graus F. Anti-Hu-associated paraneoplastic encephalomyelitis: analysis of 200 patients. Brain. 2001 Jun 1;124(6):1138–1348.
Saiz A, Bruna J, Stourac P, Vigliani MC, Giometto B, Grisold W, et al. Anti-Hu-associated brainstem encephalitis. J Neurol Neurosurg Psychiatry. 2009 Apr;80(4):404–407.
Honnorat J, Cartalat-Carel S, Ricard D, Camdessanche JP, Carpentier AF, Rogemond V, et al. Onco-neural antibodies and tumour type determine survival and neurological symptoms in paraneoplastic neurological syndromes with Hu or CV2/CRMP5 antibodies. J Neurol Neurosurg Psychiatry. 2009 Apr;80(4):412–416.
Mason WP, Graus F, Lang B, Honnorat J, Delattre JY, Valldeoriola F, et al. Small-cell lung cancer, paraneoplastic cerebellar degeneration and the Lambert-Eaton myasthenic syndrome. Brain. 1997 Aug 1;120(8):1279–1300.
Wirtz PW, Lang B, Graus F, van den Maagdenberg AMJM, Saiz A, Gans PA de K, et al. P/Q-type calcium channel antibodies, Lambert–Eaton myasthenic syndrome and survival in small cell lung cancer. J Neuroimmunol. 2005 Jul 1;164(1):161–165.
Graus F, Lang B, Pozo-Rosich P, Saiz A, Casamitjana R, Vincent A. P/Q type calcium-channel antibodies in paraneoplastic cerebellar degeneration with lung cancer. Neurology. 2002 Sep 10;59(5):764–766.
Sabater L, Höftberger R, Boronat A, Saiz A, Dalmau J, Graus F. Antibody Repertoire in Paraneoplastic Cerebellar Degeneration and Small Cell Lung Cancer. PLOS ONE. 2013 Mar 25;8(3):e60438.
Graus F, Ariño H, Dalmau J. Paraneoplastic neurological syndromes in Hodgkin and non-Hodgkin lymphomas. Blood. 2014;123:3230–3238.
Smitt PS, Kinoshita A, De Leeuw B, Moll W, Coesmans M, Jaarsma D, et al. Paraneoplastic Cerebellar Ataxia Due to Autoantibodies against a Glutamate Receptor. N Engl J Med. 2000 Jan 6; 342(1):21–27.
Marignier R, Chenevier F, Rogemond V, et al. Metabotropic glutamate receptor type 1 autoantibody–associated cerebellitis: A primary autoimmune disease? Arch Neurol. 2010 May 1;67(5):627–630.
Iorio R, Damato V, Mirabella M, Vita MG, Hulsenboom E, Plantone D, et al. Cerebellar degeneration associated with mGluR1 autoantibodies as a paraneoplastic manifestation of prostate adenocarcinoma. J Neuroimmunol. 2013 Oct 15;263(1–2):155–158.
• Lopez-Chiriboga AS, Komorowski L, Kümpfel T, Probst C, Hinson SR, Pittock SJ, et al. Metabotropic glutamate receptor type 1 autoimmunity Clinical features and treatment outcomes. Neurology. 2016 Mar 15;86(11):1009–1013. It retrospectively describes the clinical associations of immunoglobulin G (IgG) targeting metabotropic glutamate receptor 1 (mGluR1-IgG). The largest series of patients with mGLUr1 ataxia.
Gultekin SH, Rosenfeld MR, Voltz R, Eichen J, Posner JB, Dalmau J. Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients. Brain. 2000 Jul 1;123(7):1481–1494.
• van Sonderen A, Thijs RD, Coenders EC, Jiskoot LC, Sanchez E, de Bruijn MAAM, et al. Anti-LGI1 encephalitis: Clinical syndrome and long-term follow-up. Neurology. 2016 Oct 4;87(14):1449–1456. A nationwide study; a detailed description of the clinical features and long-term outcome of a LGI1 encephalitis.
• Ariño H, Armangué T, Petit-Pedrol M, Sabater L, Martinez-Hernandez E, Hara M, et al. Anti-LGI1–associated cognitive impairment Presentation and long-term outcome. Neurology. 2016 Aug 23;87(8):759–765. This paper determines the clinical presentation, long-term outcome, and LGI1 encephalitis evolution.
van Sonderen A, Ariño H, Petit-Pedrol M, Leypoldt F, Körtvélyessy P, Wandinger K-P, et al. The clinical spectrum of Caspr2 antibody-associated disease. Neurology. 2016 Aug 2;87(5):521–528.
Höftberger R, Titulaer MJ, Sabater L, Dome B, Rózsás A, Hegedus B, et al. Encephalitis and GABAB receptor antibodies Novel findings in a new case series of 20 patients. Neurology. 2013;81(17):1500–1506.
Höftberger R, van Sonderen A, Leypoldt F, Houghton D, Geschwind M, Gelfand J, et al. Encephalitis and AMPA receptor antibodies Novel findings in a case series of 22 patients. Neurology. 2015 Jun 16;84(24):2403–2412.
Caviness JN, Forsyth PA, Layton DD, McPhee TJ. The movement disorder of adult opsoclonus. Mov Disord Off J Mov Disord Soc. 1995 Jan;10(1):22–27.
Klaas JP, Ahlskog J, Pittock SJ, et al. Adult-onset opsoclonus-myoclonus syndrome. Arch Neurol. 2012 Dec 1;69(12):1598–1607.
Kinsbourne M. Myoclonic encephalopathy of infants. J Neurol Neurosurg Psychiatry. 1962 Aug;25(3):271–276.
Sahu JK, Prasad K. The opsoclonus–myoclonus syndrome. Pract Neurol. 2011 Jun 1;11(3):160–166.
• Armangué T, Sabater L, Torres-Vega E, Martínez-Hernández E, Ariño H, Petit-Pedrol M, et al. Clinical and Immunological Features of Opsoclonus-Myoclonus Syndrome in the Era of Neuronal Cell Surface Antibodies. JAMA Neurol. 2016 Apr;73(4):417–424. Report of the clinical and immunological features of idiopathic OMS (I-OMS) andparaneoplastic OMS (P-OMS), the occurrence of antibodies to cell surface antigens, and the discovery of a novel cell surface epitope.
Bataller L, Graus F, Saiz A, Vilchez JJ, Spanish Opsoclonus-Myoclonus Study Group. Clinical outcome in adult onset idiopathic or paraneoplastic opsoclonus-myoclonus. Brain J Neurol. 2001 Feb;124(Pt 2):437–443.
Dalakas MC. Stiff person syndrome: advances in pathogenesis and therapeutic interventions. Curr Treat Options Neurol. 2009;11(2):102–110.
Saiz A, Blanco Y, Sabater L, González F, Bataller L, Casamitjana R, et al. Spectrum of neurological syndromes associated with glutamic acid decarboxylase antibodies: diagnostic clues for this association. Brain. 2008 Oct 1;131(10):2553–2263.
Murinson BB, Guarnaccia JB. Stiff-person syndrome with amphiphysin antibodies Distinctive features of a rare disease. Neurology. 2008;71(24):1955–1958.
Whiteley AM, Swash M, Urich H. Progressive encephalomyelitis with rigidity. Brain J Neurol. 1976 Mar;99(1):27–42.
Carvajal-González A, Leite MI, Waters P, Woodhall M, Coutinho E, Balint B, et al. Glycine receptor antibodies in PERM and related syndromes: characteristics, clinical features and outcomes. Brain. 2014 Aug
Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011 Jan;10(1):63–74.
Schmitt SE, Pargeon K, Frechette ES, Hirsch LJ, Dalmau J, Friedman D. Extreme delta brush A unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology. 2012;79(11):1094–1100.
Petit-Pedrol M, Armangue T, Peng X, Bataller L, Cellucci T, Davis R, et al. Encephalitis with refractory seizures, status epilepticus, and antibodies to the GABAA receptor: a case series, characterisation of the antigen, and analysis of the effects of antibodies. Lancet Neurol. 2014;13(3):276–86.
• Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort . Lancet Neurol. 2013;12(2):157–65. The largest cohort of patients. It assesses the presentation of the disease, the spectrum of symptoms, immunotherapies used, timing of improvement, and long-term outcome.
Lancaster E, Martinez-Hernandez E, Titulaer MJ, Boulos M, Weaver S, Antoine J-C, et al. Antibodies to metabotropic glutamate receptor 5 in the Ophelia syndrome. Neurology. 2011;77(18):1698–16701.
Mathew RM, Vandenberghe R, Garcia-Merino A, Yamamoto T, Landolfi JC, Rosenfeld MR, et al. Orchiectomy for suspected microscopic tumor in patients with anti-Ma2-associated encephalitis. Neurology. 2007 Mar 20;68(12):900–905.
•• Dalmau J, Graus F. Antibody-Mediated Encephalitis. Ropper AH, editor. N Engl J Med. 2018 Mar;378(9):840–851. Outstanding review of the autoimmune encephalitis syndromes
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ronnyson Susano Grativvol declares that he has no conflict of interest.
Wagner Cid Palmeira Cavalcante declares that he has no conflict of interest.
Luiz Henrique Martins Castro declares that he has no conflict of interest.
Ricardo Nitrini has received research funding from FAPESP, has served on advisory boards for Janssen-Cilag and Brazilian Nutricia, has received travel funding and reimbursement from Novartis, serves as an editor for Dementia & Neuropsychologia, serves on the editorial board for Alzheimer’s Disease & Associated Disorders and International Journal of Alzheimer’s Disease, and has served as a guest speaker for Novartis and Danone (Nutricia).
Mateus Mistieri Simabukuro declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Neuro-oncology
Rights and permissions
About this article
Cite this article
Grativvol, R.S., Cavalcante, W.C.P., Castro, L.H.M. et al. Updates in the Diagnosis and Treatment of Paraneoplastic Neurologic Syndromes. Curr Oncol Rep 20, 92 (2018). https://doi.org/10.1007/s11912-018-0721-y
Published:
DOI: https://doi.org/10.1007/s11912-018-0721-y
Keywords
- Limbic encephalitis
- Onconeuronal antibodies
- Paraneoplastic neurological syndromes
- Paraneoplastic encephalomyelitis
- Paraneoplastic cerebellar degeneration
- Autoimmune encephalitis
- Stiff person syndrome
- Progressive encephalomyelitis with rigidity and myoclonus
- Opsoclonus-myoclonus syndrome
- Morvan syndrome
- Ophelia syndrome
- N-methyl-d-aspartate receptor (NMDAR) encephalitis
- Anti-AMPA receptor (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid) encephalitis
- Anti-GABAbR (γ-aminobutyric acid receptor-B) encephalitis
- Anti-leucine-rich glioma-inactivated protein 1 (LGI1) encephalitis
- Anti-Caspr2 encephalitis (contactin-associated protein-like 2)
- Anti-glycine receptor (GlyR) antibodies
- Anti-mGluR5 (metabotropic glutamate receptor 5)
- Anti-mGLUR1 (metabotropic glutamate receptor 1)
- Anti-Hu antibodies
- Anti-Ma2 antibodies
- Anti-DNER (Delta/Notch-like epidermal growth factor-related receptor) antibodies
- Anti-CV2/CRMP5 antibodies