Abstract
Background
Single anastomosis duodenal-ileal bypass with sleeve gastrectomy (SADI-S) is a modification of Roux-en-Y duodenal switch (RYDS). Long-term data on this operation is lacking in the literature. We reviewed our mid-term data of this RYDS modification.
Purpose
To analyze the outcomes with SADI-S at 4 years.
Methods
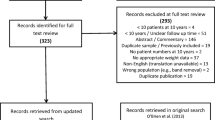
Data from patients who underwent a primary SADI-S procedure performed by three surgeons at a single institution from June 2013 through February 2018 were retrospectively reviewed. All revision bariatric surgeries were excluded. Regression analyses were performed for all follow-up weight loss data.
Results
There were 437 patients in our database. The pre-operative mean body mass index (BMI) was 49.8 ± 8.8 kg/m2. The 30-day complication rate was 7.7%. The 30-day readmission, reoperation, and mortality rates were 1.8, 1.3, and 0.2%, respectively. The long-term complication rate was 10.9%. Seventy-nine patients were 4 years post SADI-S surgery and follow-up was possible for 44 patients (55.7%). At 4 years, patients had an average change in BMI of 18.1 ± 6 units with an excess weight loss (EWL) of 85.7 ± 27.3%. At 4 years, 97.6% patients were able to maintain HbA1c < 6% with or without the use of diabetic medication. There was a statistically significant difference between most of the pre-operative and post-operative nutritional data.
Conclusions
SADI-S is a safe and effective procedure in both short- and mid-term data points. Diabetes resolution and weight loss appear similar to traditional RYDS and better than RYGB.

Similar content being viewed by others
References
Hess DS, Hess DW, Oakley RS. The biliopancreatic diversion with the duodenal switch: results beyond 10 years. Obes Surg. 2005;15(3):408–16.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Mitzman B, Cottam D, Goriparthi R, et al. Stomach intestinal pylorus sparing (SIPS) surgery for morbid obesity: retrospective analyses of our preliminary experience. Obes Surg. 2016;26(9):2098–104.
Surve A, Zaveri H, Cottam D. A safer and simpler technique of duodenal dissection and transection of the duodenal bulb for duodenal switch. Surg Obes Relat Dis. 2016;12(4):923–4.
Surve A, Zaveri H, Cottam D, et al. A retrospective comparison of biliopancreatic diversion with duodenal switch with single anastomosis duodenal switch (SIPS-stomach intestinal pylorus sparing surgery) at a single institution with two year follow-up. Surg Obes Relat Dis. 2017;13(3):415–22.
Marceau P, Hould FS, Simard S, et al. Biliopancreatic diversion with duodenal switch. World J Surg. 1998;22(9):947–54.
Sánchez-Pernaute A, Rubio Herrera MA, Pérez-Aguirre E, et al. Proximal duodenal-ileal end-to-side bypass with sleeve gastrectomy: proposed technique. Obes Surg. 2007;17(12):1614–8.
Nightingale J, Woodward JM. Guidelines for management of patients with short bowel. Gut. 2006;55(Suppl 4):v1–12.
Brown WA, Ooi G, Higa K, et al. Single anastomosis duodenal-ileal bypass with sleeve gastrectomy/one anastomosis duodenal switch (SADI-S/OADS) IFSO position statement. Obes Surg. 2018;28:1207–16.
Sánchez-Pernaute A, Rubio Herrera MA, Pérez-Aguirre ME, et al. Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). One to three-year follow-up. Obes Surg. 2010;20(12):1720–6.
Neichoy BT, Schniederjan B, Dr C, et al. Stomach intestinal pylorus-sparing surgery for morbid obesity. JSLS. 2018;22(1):e2017.00063.
Sanchez-Pernaute A, Rubio MA, Cabrerizo L, et al. Single-anastomosis duodenoileal bypass with sleeve gastrectomy (SADI-S) for obese diabetic patients. Surg Obes Relat Dis. 2015;11(5):1092–8.
Surve A, Cottam D, Sanchez-Pernaute A, et al. The incidence of complications associated with loop duodeno-ileostomy after single-anastomosis duodenal switch procedures among 1328 patients: a multicenter experience. In: Surg Obes Relat Dis, vol. 14; 2018. p. 594–601.
Sethi M, Chau E, Youn A, et al. Long-term outcomes after biliopancreatic diversion with and without duodenal switch: 2-, 5-, and 10-year data. Surg Obes Relat Dis. 2016;12(9):1697–705.
Biertho L, Lebel S, Marceau S, et al. Perioperative complications in a consecutive series of 1000 duodenal switches. Surg Obes Relat Dis. 2013;9(1):63–8.
Obied N, Malick W, Concors S, et al. Long-term outcomes after Roux-en-Y gastric bypass: 10-13 year data. Surg Obes Relat Dis. 2016;12(1):11–20.
Higa KD, Boone KB, Ho T. Complications of the laparoscopic Roux-en-Y gastric bypass: 1040 patients. What have we learned? Obes Surg. 2000;10:509–13.
Marceau P, Biron S, Marceau S, et al. Biliopancreatic diversion duodenal switch: independent contributions of sleeve resection and duodenal exclusion. Obes Surg. 2014;24:1843–9.
Cottam A, Cottam D, Roslin M, et al. A matched cohort analysis of sleeve gastrectomy with and without 300 cm loop duodenal switch with 18-month follow-up. Obes Surg. 2016;26(10):2363–9.
Surve A, Zaveri H, Cottam D, et al. Mid-term outcomes of gastric bypass weight loss failure to duodenal switch. Surg Obes Relat Dis. 2016;12(9):1663–70.
DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med. 2007;356:2176–83.
Goldner Ws SJA, Lyden E, et al. Finding the optimal dose of vitamin D following Roux-en-Y gastric bypass: a prospective, randomized, pilot clinical trial. Obes Surg. 2009;19:173–9.
Einarsdottir K, Preen DB, Clay TD, et al. Effect of a single “megadose” intramuscular vitamin D (600000 IU) injection on vitamin D concentrations and bone mineral density following biliopancreatic diversion surgery. Obes Surg. 2010;20:732–7.
Dolan K, Hatzifotis M, Newbury L, et al. A clinical and nutritional comparison of biliopancreatic diversion with and without duodenal switch. Ann Surg. 2004;240:51–6.
Abd-Elatif A, Yousser T, Farid M, et al. Nutritional markers after loop duodenal switch (SADI-S) for morbid obesity: a technique with favorable nutritional outcome. J Obes Weight Loss Ther. 2015;5(3):1000268.
Surve A, Zaveri H, Cottam D. Retrograde filling of the afferent limb as a cause of chronic nausea after single anastomosis loop duodenal switch. Surg Obes Relat Dis. 2016;12(4):e39–42.
Zhang H, Han X, Yu H, Di J, Zhang P, Jia W. Effect of Roux-en-Y gastric bypass on remission of T2D: medium-term follow-up in Chinese patients with different BMI obesity class. Obes Surg 2016:1–9.
Purnell JQ, Selzer F, Wahed AS, et al. Type 2 diabetes remission rates after laparoscopic gastric bypass and gastric banding: results of the longitudinal assessment of bariatric surgery study. Diabetes Care. 2016;39(7):1101–7.
Sjostrom L, Peltonen M, Jacobsen P, et al. Association of bariatric surgery with long term remission of type 2 diabetes with microvascular and macrovascular complications. JAMA. 2014;311(22):2297–304.
Bretheur SA, Aminian A, Romero-Talamas H, et al. Can diabetes be surgically cured. Long term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013;258(4):628–37.
Digiorgi M, Rosen DJ, Choi JJ, et al. Re-emergence of diabetes after gastric bypass in patients with mid-to long term follow-up. Surg Obes Relat Dis. 2010;6(3):254–9.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376:641–51.
Roslin MS, Gagner M, Goriparthi R, et al. The rationale for a duodenal switch as the primary surgical treatment of advanced type 2 diabetes mellitus and metabolic disease. Surg Obes Relat Dis. 2015;11:704–10.
Marceau P, Biron S, Marceau S, et al. Long-term metabolic outcomes 5 to 20 years after biliopancreatic diversion. Obes Surg. 2015;25:1584–93.
Scopinaro N. Biliopancreatic diversion: mechanisms of action and long term results. Obes Surg. 2006;16:683–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Statement of Human and Animal Rights
I certify that the manuscript did not involve the use of animal or human subjects.
Since this is a retrospective study, the formal consent is not required for this type of study.
Conflict of Interest
Daniel Cottam, the corresponding author reports personal fees and other from Medtronic, outside the submitted work.
Hinali Zaveri has no conflict of interest to declare.
Amit Surve has no conflict of interest to declare.
Austin Cottam has no conflict of interest to declare.
Walter Medlin has no conflict of interest to declare.
Christina Richards has no conflict of interest to declare.
LeGrand Belnap has no conflict of interest to declare.
Samuel Cottam has no conflict of interest to declare.
Benjamin Horsley has no conflict of interest to declare.
All other authors have no commercial associations that might be a conflict of interest in relation to this article.
Rights and permissions
About this article
Cite this article
Zaveri, H., Surve, A., Cottam, D. et al. Mid-term 4-Year Outcomes with Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy Surgery at a Single US Center. OBES SURG 28, 3062–3072 (2018). https://doi.org/10.1007/s11695-018-3358-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3358-x