Abstract
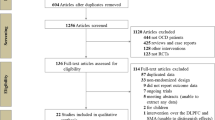
Randomised and sham-controlled trials (RCTs) of repetitive transcranial magnetic stimulation (rTMS) in the treatment of obsessive-compulsive disorder (OCD) have yielded conflicting results, which may be due to the variability in rTMS parameters used. We performed an updated systematic review and meta-analysis on the effectiveness of rTMS for the treatment of OCD and aimed to determine whether certain rTMS parameters, such as cortical target, may be associated with higher treatment effectiveness. After conducting a systematic literature review for RCTs on rTMS for OCD through to 1 December 2016 using MEDLINE, PubMed, Web of Science, PsycINFO, Google, and Google Scholar, we performed a random-effects meta-analysis with the outcome measure as pre-post changes in Yale-Brown Obsessive Compulsive Scale (Y-BOCS) scores. To determine whether rTMS parameters may have influenced treatment effectiveness, studies were further analysed according to cortical target, stimulation frequency, and length of follow-up. Data were obtained from 18 RCTs on rTMS in the treatment of OCD. Overall, rTMS yielded a modest effect in reducing Y-BOCS scores with Hedge’s g of 0.79 (95% CI = 0.43–1.15, p < 0.001). Stimulation of the supplementary motor area yielded the greatest reductions in Y-BOCS scores relative to other cortical targets. Subgroup analyses suggested that low frequency rTMS was more effective than high frequency rTMS. The effectiveness of rTMS was also greater at 12 weeks follow-up than at four weeks follow-up. Our meta-analysis implies that low frequency rTMS applied over the supplementary motor area may offer the greatest effectiveness in the treatment of OCD. The therapeutic effects of rTMS also appear to persist post-treatment and may offer beneficial long-term effectiveness. With our findings, it is suggested that future large-scale studies focus on the supplementary motor area and include follow-up periods of 12 weeks or more.







Similar content being viewed by others
References
Ruscio A, Stein D, Chiu W, Kessler R. The epidemiology of obsessive-compulsive disorder in the national comorbidity survey replication. Mol Psychiatry. 2010;15(1):53–63.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association; 2013.
Skoog G, Skoog I. A 40-year follow-up of patients with obsessive-compulsive disorder. Arch Gen Psychiatry. 1999;56(2):121–7.
DuPont RL, Rice D, Shiraki S, Rowland C. Economic costs of obsessive-compulsive disorder. Med Interface. 1995;8(4):102–9.
Fullana MA, Mataix-Cols D, Caspi A, Harrington H, Grisham JR, Moffitt TE, et al. Obsessions and compulsions in the community: prevalence, interference, help-seeking, developmental stability, and co-occurring psychiatric conditions. Am J Psychiatr. 2009;166(3):329–36.
Stein DJ, Koen N, Fineberg N, Fontenelle LF, Matsunaga H, Osser D, et al. A 2012 evidence-based algorithm for the pharmacotherapy for obsessive-compulsive disorder. Curr Psychiatry Rep. 2012;14(3):211–9. https://doi.org/10.1007/s11920-012-0268-9.
Pallanti S, Hollander E, Bienstock C, Koran L, Leckman J, Marazziti D, et al. Treatment non-response in OCD: methodological issues and operational definitions. Int J Neuropsychopharmacol. 2002;5(2):181–91.
Abramowitz JS, Franklin ME, Foa EB. Empirical status of cognitive-behavioral therapy for obsessive-compulsive disorder: a meta-analytic review. Rom J Cogn Behav Psychother. 2002;2(2):89–104.
Rauch SL, Jenike MA. Management of treatment resistant obsessive-compulsive disorder: concepts and strategies. In: Hollander E, Zohar J, Marazziti D, Olivier B, editors. Obsessive compulsive disorder. Chicester: Wiley; 1994. p. 227–44.
Blom RM, Figee M, Vulink N, Denys D. Update on repetitive transcranial magnetic stimulation in obsessive-compulsive disorder: different targets. Curr Psychiatry Rep. 2011;13(4):289–94.
Saba G, Moukheiber A, Pelissolo A. Transcranial cortical stimulation in the treatment of obsessive-compulsive disorders: efficacy studies. Curr Psychiatry Rep. 2015;17(5):1–8.
Jaafari N, Rachid F, Rotge JY, Polosan M, El-Hage W, Belin D, et al. Safety and efficacy of repetitive transcranial magnetic stimulation in the treatment of obsessive-compulsive disorder: a review. World J Biol Psychiatry. 2012;13(3):164–77.
Husain F, Nandipati G, Braun A, Cohen L, Tagamets M, Horwitz B. Simulating transcranial magnetic stimulation during PET with a large-scale neural network model of the prefrontal cortex and the visual system. NeuroImage. 2002;15(1):58–73.
Pascual-Leone A, Keenan J, Freund S, Stinchfield Z, Tormos J, Parker A, et al. Repetitive transcranial magnetic stimulation trials in depression. Eur Neuropsychopharmacol. 1998;8:S123–S4.
Speer AM, Kimbrell TA, Wassermann EM, Repella JD, Willis MW, Herscovitch P, et al. Opposite effects of high and low frequency rTMS on regional brain activity in depressed patients. Biol Psychiatry. 2000;48(12):1133–41.
Fineberg N, Chamberlain S, Hollander E, Boulougouris V, Robbins T. Translational approaches to obsessive-compulsive disorder: from animal models to clinical treatment. Br J Pharmacol. 2011;164(4):1044–61.
Milad MR, Rauch SL. Obsessive-compulsive disorder: beyond segregated cortico-striatal pathways. Trends Cogn Sci. 2012;16(1):43–51.
Del Casale A, Kotzalidis G, Rapinesi C, Serata D, Ambrosi E, Simonetti A, et al. Functional neuroimaging in obsessive-compulsive disorder. Neuropsychobiology. 2011;64(2):61–85.
Chamberlain SR, Menzies L, Hampshire A, Suckling J, Fineberg NA, del Campo N, et al. Orbitofrontal dysfunction in patients with obsessive-compulsive disorder and their unaffected relatives. Science. 2008;321(5887):421–2.
Nakao T, Nakagawa A, Yoshiura T, Nakatani E, Nabeyama M, Yoshizato C, et al. Brain activation of patients with obsessive-compulsive disorder during neuropsychological and symptom provocation tasks before and after symptom improvement: a functional magnetic resonance imaging study. Biol Psychiatry. 2005;57(8):901–10. https://doi.org/10.1016/j.biopsych.2004.12.039.
van den Heuvel OA, Veltman DJ, Groenewegen HJ, Cath DC, van Balkom AJ, van Hartskamp J, et al. Frontal-striatal dysfunction during planning in obsessive-compulsive disorder. Arch Gen Psychiatry. 2005;62(3):301–9.
Yücel M, Harrison BJ, Wood SJ, Fornito A, Wellard RM, Pujol J, et al. Functional and biochemical alterations of the medial frontal cortex in obsessive-compulsive disorder. Arch Gen Psychiatry. 2007;64(8):946–55.
Nakao T, Nakagawa A, Nakatani E, Nabeyama M, Sanematsu H, Yoshiura T, et al. Working memory dysfunction in obsessive–compulsive disorder: a neuropsychological and functional MRI study. J Psychiatr Res. 2009;43(8):784–91.
Greenberg BD, George MS, Martin JD, Benjamin J, Schlaepfer TE, Altemus M, et al. Effect of prefrontal repetitive transcranial magnetic stimulation in obsessive-compulsive disorder: a preliminary study. Am J Psychiatr. 1997;154(6):867–9.
Sachdev PS, McBride R, Loo CK, Mitchell PB, Malhi GS, Croker VM. Right versus left prefrontal transcranial magnetic stimulation for obsessive-compulsive disorder: a preliminary investigation. J Clin Psychiatry. 2001;62(12):981–4.
Alonso P, Pujol J, Cardoner N, Benlloch L, Deus J, Menchon JM, et al. Right prefrontal repetitive transcranial magnetic stimulation in obsessive-compulsive disorder: a double-blind, placebo-controlled study. Am J Psychiatry. 2001;158(7):1143–5.
Sachdev PS, Loo CK, Mitchell PB, TF MF, Malhi GS. Repetitive transcranial magnetic stimulation for the treatment of obsessive compulsive disorder: a double-blind controlled investigation. Psychol Med. 2007;37(11):1645–9.
Berlim MT, Neufeld NH, Van den Eynde F. Repetitive transcranial magnetic stimulation (rTMS) for obsessive-compulsive disorder (OCD): an exploratory meta-analysis of randomized and sham-controlled trials. J Psychiatr Res. 2013;47(8):999–1006. https://doi.org/10.1016/j.jpsychires.2013.03.022.
Trevizol AP, Shiozawa P, Cook IA, Sato IA, Kaku CB, Guimaraes FB, et al. Transcranial magnetic stimulation for obsessive-compulsive disorder: an updated systematic review and meta-analysis. J ECT. 2016;32(4):262–6. https://doi.org/10.1097/yct.0000000000000335.
Gomes PO, Rosa MA, Allam N, de Souza ER, Brasil-Neto J. A randomized double-blind trial of repetitive transcranial magnetic stimulation in obsessive -compulsive disorder with three months follow-up. J ECT. 2012;28(2):149.
Hawken ER, Dilkov D, Kaludiev E, Simek S, Zhang F, Milev R. Transcranial magnetic stimulation of the supplementary motor area in the treatment of obsessive-compulsive disorder: a multi-site study. Int J Mol Sci. 2016;17(3):420. https://doi.org/10.3390/ijms17030420.
Mantovani A, Simpson HB, Fallon BA, Rossi S, Lisanby SH. Randomized sham-controlled trial of repetitive transcranial magnetic stimulation in treatment-resistant obsessive-compulsive disorder. Int J Neuropsychopharmacol. 2010;13(2):217–27.
Nauczyciel C, Le Jeune F, Naudet F, Douabin S, Esquevin A, Verin M, et al. Repetitive transcranial magnetic stimulation over the orbitofrontal cortex for obsessive-compulsive disorder: a double-blind, crossover study. Transcult Psychiatry. 2014;4:e436.
Ruffini C, Locatelli M, Lucca A, Benedetti F, Insacco C, Smeraldi E. Augmentation effect of repetitive transcranial magnetic stimulation over the orbitofrontal cortex in drug-resistant obsessive-compulsive disorder patients: a controlled investigation. Prim Care Companion J Clin Psychiatry. 2009;11(5):226–30. https://doi.org/10.4088/PCC.08m00663.
Mantovani A, Rossi S, Bassi BD, Simpson HB, Fallon BA, Lisanby SH. Modulation of motor cortex excitability in obsessive-compulsive disorder: an exploratory study on the relations of neurophysiology measures with clinical outcome. Psychiatry Res. 2013;210(3):1026–32.
Russo M, Naro A, Mastroeni C, Morgante F, Terranova C, Muscatello MR, et al. Obsessive-compulsive disorder: a "sensory-motor" problem? Int J Psychophysiol Off J Int Org Psychophysiol. 2014;92(2):74–8. https://doi.org/10.1016/j.ijpsycho.2014.02.007.
Kumar N, Chadda RK. Augmentation effect of repetitive transcranial magnetic stimulation over the supplementary motor cortex in treatment refractory patients with obsessive compulsive disorder. Indian J Psychiatry. 2011;53(4):340–2. https://doi.org/10.4103/0019-5545.91909.
Pelissolo A, Harika-Germaneau G, Rachid F, Gaudeau-Bosma C, Tanguy ML, BenAdhira R, et al. Repetitive transcranial magnetic stimulation to supplementary motor area in refractory obsessive-compulsive disorder treatment: a sham-controlled trial. Int J Neuropsychopharmacol. 2016;19(8) https://doi.org/10.1093/ijnp/pyw025.
Berlim MT, Van den Eynde F, Daskalakis ZJ. Clinically meaningful efficacy and acceptability of low-frequency repetitive transcranial magnetic stimulation (rTMS) for treating primary major depression: a meta-analysis of randomized, double-blind and sham-controlled trials. Neuropsychopharmacology. 2013;38(4):543–51.
Prasko J, Paskova B, Zalesky R, Novak T, Kopecek M, Bares M, et al. The effect of repetitive transcranial magnetic stimulation (rTMS) on symptoms in obsessive compulsive disorder. A randomized, double blind, sham controlled study. Neuroendocrinol Lett. 2006;27(3):327–32.
Kang JI, Kim CH, Namkoong K, Lee CI, Kim SJ. A randomized controlled study of sequentially applied repetitive transcranial magnetic stimulation in obsessive-compulsive disorder. J Clin Psychiatry. 2009;70(12):1645–51.
Badawy AA, El Sawy H, El Hay MA. Efficacy of repetitive transcranial magnetic stimulation in the management of obsessive compulsive disorder. Egyptian Journal of Neurology, Psychiatry and Neurosurgery. 2010;47:393–7.
Sarkhel S, Sinha VK, Praharaj SK. Adjunctive high-frequency right prefrontal repetitive transcranial magnetic stimulation (rTMS) was not effective in obsessive-compulsive disorder but improved secondary depression. J Anxiety Disord. 2010;24(5):535–9.
Mansur CG, Myczkowki ML, Cabral SD, Sartorelli MDB, Bellini BB, Dias AM, et al. Placebo effect after prefrontal magnetic stimulation in the treatment of resistant obsessive-compulsive disorder: a randomized controlled trial. Int J Neuropsychopharmacol. 2011;14(10):1389–97. https://doi.org/10.1017/s1461145711000575.
Ma Z-R, Shi L-J. Repetitive transcranial magnetic stimulation (rTMS) augmentation of selective serotonin reuptake inhibitors (SSRIs) for SSRI-resistant obsessive-compulsive disorder (OCD): a meta-analysis of randomized controlled trials. Int J Clin Exp Med. 2014;7(12):4897.
Zhang XZ, Gu Y, Zhao EQ, Li YZ. Research on treating refractory obsessive compulsive disorder with combination of sitaplam and repetitive transcranial magnetic stimulation. Chin J Health Psychol. 2010;18:778–80.
Cheng J, Li H, Shi YZ. The efficacy of repetitive transcranial magnetic stimulation on obsessive compulsive disorder. Journal of International Psychiatry. 2013;40:148–51.
Ma X, Huang Y, Liao L, Jin Y. A randomized double-blinded sham-controlled trial of alpha electroencephalogram-guided transcranial magnetic stimulation for obsessive-compulsive disorder. Chin Med J. 2014;127(4):601–6.
Haghighi M, Shayganfard M, Jahangard L, Ahmadpanah M, Bajoghli H, Pirdehghan A, et al. Repetitive transcranial magnetic stimulation (rTMS) improves symptoms and reduces clinical illness in patients suffering from OCD: results from a single-blind, randomized clinical trial with sham cross-over condition. J Psychiatr Res. 2015;68:238–44.
Zhou D-D, Wang W, Wang G-M, Li D-Q, Kuang L. An updated meta-analysis: short-term therapeutic effects of repeated transcranial magnetic stimulation in treating obsessive-compulsive disorder. J Affect Disord. 2017;215:187–96. https://doi.org/10.1016/j.jad.2017.03.033.
Tang LY, Chu FC, Li YD, Xu ZP. Treating refractory obsessive compulsive disorder with combination of paroxetine and repetitive transcranial magnetic stimulation: a double-blind sham controlled study. Chinese Journal of Behavioral Medical and Brain Science. 2010;19(7):604–6.
Han CF, Jiang DF. Effect of slow frequency repetitive Transcranial Magnetic Stimulation (rTMS) combined with fluvoxamine on obsessivecompulsive disorder in maintenance stage. J Psychiatry. 2015;28:446–48.
Luo XF, Huang MI, Ye XJ. Controlled clinical study of sertraline alone or combined repetitive transcranial magnetic stimulation in patients with refractory obsessive-compulsive disorder. J Clin Psychiatry. 2015;25:238–240.
Elbeh KA, Elserogy YM, Khalifa HE, Ahmed MA, Hafez MH, Khedr EM. Repetitive transcranial magnetic stimulation in the treatment of obsessive-compulsive disorders: double blind randomized clinical trial. Psychiatry Res. 2016;238:264–9. https://doi.org/10.1016/j.psychres.2016.02.031.
Jahangard L, Haghighi M, Shyayganfard M, Ahmadpanah M, Bahmani DS, Bajoghli H, et al. Repetitive transcranial magnetic stimulation improved symptoms of obsessive-compulsive disorder, but also cognitive performance: results from a randomized clinical trial with a cross-over design and sham condition. Neuropsychobiology. 2016;73(4):224–32. https://doi.org/10.1159/000446287.
Seo HJ, Jung YE, Lim HK, Um YH, Lee CU, Chae JH. Adjunctive low-frequency repetitive transcranial magnetic stimulation over the right dorsolateral prefrontal cortex in patients with treatment-resistant obsessive-compulsive disorder: a randomized controlled trial. Clinical Psychopharmacology and Neuroscience. 2016;14(2):153–60. https://doi.org/10.9758/cpn.2016.14.2.153.
Zhang ZM. A control study of sertraline plus rTMS in the treatment of refractory OCD. J Clin Psychosom Dis. 2016;22:41–3.
Wassermann EM, Zimmermann T. Transcranial magnetic brain stimulation: therapeutic promises and scientific gaps. Pharmacol Ther. 2012;133(1):98–107. https://doi.org/10.1016/j.pharmthera.2011.09.003.
Moher D, Liberati A, Tetzlaff J, Altman DG. Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000.
Organization WH. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization. 1993. Report No.: 9789241544559;9241544554; Contract No.: Report.
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown obsessive compulsive scale: I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46(11):1006–11.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Higgins J, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses [journal article as teaching resource, deposited by John Flynn]. Br Med J. 2003;327:557–60.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Orwin RG. A fail-safe N for effect size in meta-analysis. J Educ Stat. 1983;8(2):157–9.
Borenstein M, Hedges LV, Higgins J, Rothstein HR. Multiple comparisons within a study. Introduction to meta-analysis. Chichester: John Wiley & Sons, Ltd.; 2009. p. 239–42.
de Wit SJ, de Vries FE, van der Werf YD, Cath DC, Heslenfeld DJ, Veltman EM, et al. Presupplementary motor area hyperactivity during response inhibition: a candidate endophenotype of obsessive-compulsive disorder. Am J Psychiatr. 2012;169(10):1100–8.
Oliveri M, Babiloni C, Filippi M, Caltagirone C, Babiloni F, Cicinelli P, et al. Influence of the supplementary motor area on primary motor cortex excitability during movements triggered by neutral or emotionally unpleasant visual cues. Exp Brain Res. 2003;149(2):214–21.
Picard N, Strick PL. Imaging the premotor areas. Curr Opin Neurobiol. 2001;11(6):663–72.
Rossi S, Bartalini S, Ulivelli M, Mantovani A, Di Muro A, Goracci A, et al. Hypofunctioning of sensory gating mechanisms in patients with obsessive-compulsive disorder. Biol Psychiatry. 2005;57(1):16–20.
van den Heuvel OA, Remijnse PL, Mataix-cols D, Vrenken H, Groenewegen HJ, HBM U, et al. The major symptom dimensions of obsessive-compulsive disorder are mediated by partially distinct neural systems. Brain. 2009;132(Pt 4):853–68.
Kedzior KK, Azorina V, Reitz SK. More female patients and fewer stimuli per session are associated with the short-term antidepressant properties of repetitive transcranial magnetic stimulation (rTMS): a meta-analysis of 54 sham-controlled studies published between 1997–2013. Neuropsychiatr Dis Treat. 2014;10:727–56.
Berlim M, Van den Eynde F, Tovar-Perdomo S, Daskalakis Z. Response, remission and drop-out rates following high-frequency repetitive transcranial magnetic stimulation (rTMS) for treating major depression: a systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. Psychol Med. 2014;44(02):225–39.
Hegde A, Ravi M, Subhasini VS, Arumugham SS, Thirthalli J, Reddy YCJ. Repetitive transcranial magnetic stimulation over presupplementary motor area may not be helpful in treatment-refractory obsessive-compulsive disorder. A Case Series Journal of ECT. 2016;32(2):139–42. https://doi.org/10.1097/yct.0000000000000291.
Angst J, Gamma A, Endrass J, Goodwin R, Ajdacic V, Eich D, et al. Obsessive-compulsive severity spectrum in the community: prevalence, comorbidity, and course. Eur Arch Psychiatry Clin Neurosci. 2004;254(3):156–64.
Ridding MC, Rothwell JC. Is there a future for therapeutic use of transcranial magnetic stimulation? Nat Rev Neurosci. 2007;8(7):559–67.
Stein DJ, Carey PD, Lochner C, Seedat S, Fineberg N, Andersen EW. Escitalopram in obsessive-compulsive disorder: response of symptom dimensions to pharmacotherapy. CNS Spectr. 2008;13(6):492–8.
Rasmussen S, Hackett E, DuBoff E, Greist J, Halaris A, Koran L, et al. A 2-year study of sertraline in the treatment of obsessive-compulsive disorder. Int Clin Psychopharmacol. 1997;12(6):309–16.
Clomipramine Collaborative Study Group. Clomipramine in the treatment of patients with obsessive-compulsive disorder. Arch Gen Psychiatry. 1991;48(8):730.
Montgomery S, Kasper S, Stein D, Hedegaard KB, Lemming O. Citalopram 20 mg, 40 mg and 60 mg are all effective and well tolerated compared with placebo in obsessive-compulsive disorder. Int Clin Psychopharmacol. 2001;16(2):75–86.
Tang W, Zhu Q, Gong X, Zhu C, Wang Y, Chen S. Cortico-striato-thalamo-cortical circuit abnormalities in obsessive-compulsive disorder: a voxel-based morphometric and fMRI study of the whole brain. Behav Brain Res. 2016;313:17–22. https://doi.org/10.1016/j.bbr.2016.07.004.
Lefaucheur J-P, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125(11):2150–206.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Association; 1994.
Acknowledgements
We would like to acknowledge the Sydney Medical School of the University of Sydney for funding a summer school placement for Simone Rehn to complete this research under the supervision of Dr. Vlasios Brakoulias.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The Authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Rehn, S., Eslick, G.D. & Brakoulias, V. A Meta-Analysis of the Effectiveness of Different Cortical Targets Used in Repetitive Transcranial Magnetic Stimulation (rTMS) for the Treatment of Obsessive-Compulsive Disorder (OCD). Psychiatr Q 89, 645–665 (2018). https://doi.org/10.1007/s11126-018-9566-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-018-9566-7